
#1 hidden risk factor for heart attacks most doctors miss

You regularly check your cholesterol. You monitor your blood pressure. Your doctor says everything looks “fine.” On paper, your results might appear normal—but deep down, you still feel uneasy. Maybe it’s a gut feeling, or a strong family history of heart disease that keeps you up at night. Here’s the inconvenient truth: the standard heart health playbook is missing a crucial chapter. And that missing piece could mean the difference between prevention and a surprise heart attack.
While routine screenings are essential, they’re often focused on surface-level indicators. What they fail to capture is a deeper, more dangerous force quietly damaging your arteries from the inside out—oxidative stress. This isn’t just another health buzzword. It’s the biochemical root of inflammation, plaque buildup, and ultimately, the heart attack that no one saw coming. And yet, most conventional doctors don’t test for it.
Not because it’s unproven—quite the opposite. It’s just that the medical system hasn’t caught up with the science. In this article, we’ll uncover what oxidative stress is, why it’s ignored by the conventional model, and most importantly, how you can test for it, reduce it, and take true control of your heart health.
(This article draws from the expertise of board-certified cardiologist Dr. Jack Wolfson, a pioneer in integrative heart care.)
🔍 Key Takeaways:
-
Oxidative Stress is the Real Culprit: It damages your arteries at the cellular level, paving the way for inflammation and plaque.
-
Standard Tests Are Incomplete: Cholesterol and blood pressure alone don’t give the full picture of heart risk.
-
Conventional Medicine Often Misses It: It’s not part of standard training, insurance coverage, or the pharmaceutical model.
-
You Can Take Control: By making targeted lifestyle, diet, and supplement changes, you can reduce oxidative stress dramatically.
-
Testing is Now Accessible: Affordable, at-home urine tests can reveal your oxidative stress levels—and show you how to act.
1. What Is Oxidative Stress—and Why Should You Care?
To grasp oxidative stress, think about rust on metal. Now imagine that same process, but happening inside your body. At its core, oxidative stress is a biological imbalance between damaging molecules called free radicals and your body's natural defenses—antioxidants.
Free radicals are unstable molecules missing an electron. In their search to become stable, they steal electrons from healthy cells, damaging DNA, proteins, and cell membranes in the process. This sets off a domino effect of cellular injury.
Your body fights back using antioxidants—compounds that donate electrons to neutralize free radicals without becoming unstable themselves. But when free radicals outnumber antioxidants, oxidative stress takes over.
This “invisible inflammation” particularly harms the endothelium—the delicate lining of your arteries. Damaged endothelial cells become sticky, inflamed, and vulnerable to cholesterol buildup. Over time, this triggers the development of atherosclerosis, the hardening and narrowing of arteries.
And here’s the danger: oxidative stress often builds up silently for years, showing no symptoms until it’s too late.
2. The “Normal” Numbers Fallacy: Cholesterol Doesn’t Tell the Whole Story
We’ve been conditioned to fear high cholesterol, especially LDL (the so-called “bad” cholesterol). But that’s only part of the story. The real issue is oxidized LDL—LDL particles that have been damaged by free radicals.
When LDL cholesterol becomes oxidized, it transforms into a toxic substance. Your immune system identifies it as a threat and sends macrophages (immune cells) to engulf the oxidized LDL. These become foam cells, which get trapped in artery walls and form plaque.
This is how heart disease progresses—even in people with “normal” cholesterol levels. You could have a pristine lab report and still be on the brink of a heart attack due to unmeasured oxidative stress.
Bottom line: it’s not just how much cholesterol you have—it’s whether that cholesterol is being damaged by oxidative stress.
3. Why Your Doctor Probably Isn’t Testing for This
Reason #1: It’s Not in the Medical School Curriculum
Most doctors are well-intentioned and smart. But their education is based on a model designed to diagnose disease and treat it with standardized protocols. They’re trained to react, not prevent. Oxidative stress is a root cause issue—something that functional and integrative medicine practitioners focus on—but it’s rarely addressed in traditional training.
Conventional cardiology excels at managing emergencies, like heart attacks or arrhythmias, but it often falls short when it comes to understanding why those events occur in the first place.
In most 10-minute doctor visits, there's no time or framework to explore oxidative stress—especially when it’s not part of the routine playbook.
Reason #2: Insurance Doesn’t Cover It
Insurance companies don’t prioritize prevention. They pay for procedures after a problem develops—angioplasty, stents, bypass surgeries—not the tests that could prevent those procedures from ever being needed.
Because tests for oxidative stress aren’t part of “standard of care,” they’re often dismissed as “unnecessary” or “experimental,” even when backed by solid science. This creates a frustrating catch-22: doctors don’t offer the tests because insurance won’t pay, and insurance won’t pay because doctors don’t offer them widely enough.
The result? Patients lose out on life-saving information.
Reason #3: There's No Pill for It
Let’s be blunt: pharmaceutical companies thrive on treating symptoms, not root causes. Oxidative stress doesn’t have a one-pill solution. It requires comprehensive lifestyle changes—things that don’t fit neatly into a prescription pad or generate recurring profits.
While blood pressure and cholesterol medications are important tools, they don’t heal the body—they manage it. Oxidative stress, on the other hand, can be reversed with the right combination of diet, sleep, supplementation, and stress reduction.
But that takes time, education, and patient commitment—three things often missing in today’s fast-paced medical system.
4. You Can’t Fix What You Don’t Measure: Why Testing is Vital
Trying to manage heart health without measuring oxidative stress is like driving blindfolded in a storm. You’re guessing. But now, thanks to advances in testing, you no longer have to.
Simple, at-home urine tests can now measure markers of oxidative stress—byproducts like 8-OHdG or MDA—which indicate cellular damage. These tests give you a tangible number that reflects your oxidative load. It’s actionable, repeatable, and potentially more revealing than a cholesterol panel.
Armed with this data, you’re no longer a passive participant in your healthcare. You can make informed, targeted changes and track your improvement over time.
5. Your Battle Plan Against Oxidative Stress
Here’s how to start reducing oxidative stress and protecting your heart—today.
🍇 Eat an Antioxidant-Rich Diet
Focus on whole, colorful foods. Plants contain phytochemicals—natural compounds that fight oxidative damage. Aim for:
-
Leafy greens (kale, spinach, arugula)
-
Berries (blueberries, raspberries, blackberries)
-
Cruciferous veggies (broccoli, cauliflower, Brussels sprouts)
-
Healthy fats (avocados, olives, wild-caught salmon)
🚫 Avoid Oxidative Offenders
Remove foods that fuel inflammation and free radical production:
-
Processed sugars and flours
-
Artificial trans fats
-
Refined vegetable oils (canola, corn, soybean)
-
Excess alcohol and charred meats
💊 Consider Smart Supplementation
Some key supplements shown to reduce oxidative stress include:
-
CoQ10 – Supports heart mitochondria and lowers oxidative load
-
Vitamin C & E – Potent antioxidants that regenerate each other
-
Selenium & Zinc – Crucial for antioxidant enzyme function
-
Glutathione – Known as the body’s “master antioxidant”
Work with a qualified healthcare provider to find the right dosages and forms.
🧘♀️ Manage Stress & Improve Sleep
Chronic stress and poor sleep are major pro-oxidant triggers. Prioritize:
-
Deep breathing or meditation daily
-
7–8 hours of quality, uninterrupted sleep
-
Evening wind-down routines (limit screens, caffeine, and late meals)
Even small improvements here can dramatically reduce oxidative damage.
Final Thoughts: Don't Wait for a Crisis
Your heart health is too precious to leave to outdated models and incomplete tests. While blood pressure and cholesterol are important, they only scratch the surface. If oxidative stress is the fire that’s silently burning in your arteries, then cholesterol is merely the dry wood waiting to ignite.
The good news? You can take control. Testing for oxidative stress, making powerful lifestyle changes, and shifting from symptom-management to root-cause healing puts you in the driver’s seat.
Don’t settle for “normal” when you could be thriving.
Now is the time to take your heart health into your own hands—and build a life of resilience, energy, and true prevention.
News in the same category


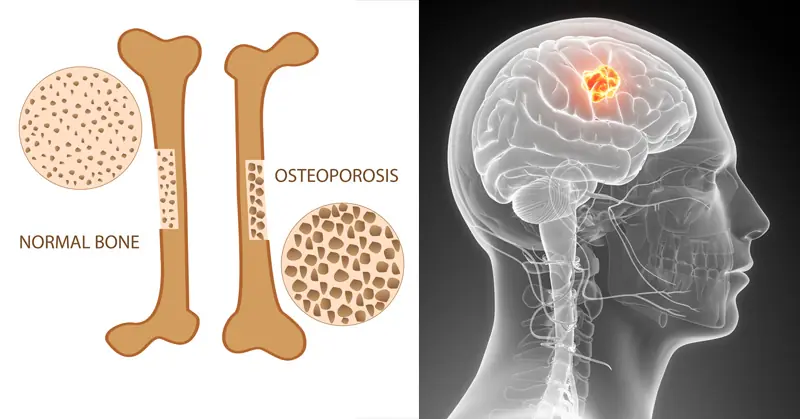
Top 15 Natural Collagen-Boosting Foods That Rebuild Skin, Joints, and Bones Fast

Cleanse Your Kidneys of Toxins With 2 Effective 1-Ingredient Drinks

Top 6 Natural Remedies to Fight Neuropathic Pain (Peripheral Neuropathy Home Remedies)

Revitalize Your Kidneys with This Ancient Amazonian Infusion
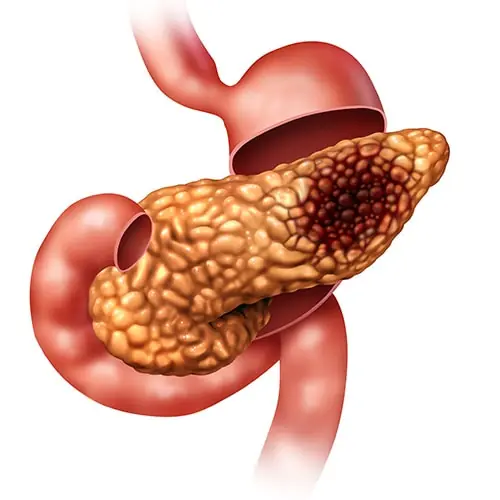
5 Early Warning Signs of Pancreatic Cancer, According to Survivors

Drink Water On An Empty Stomach Immediately After Waking Up – 8 Powerful Benefits

17 Worst Foods for Diabetics
Man has stroke after bathing right after meal: 3 mistakes you shouldn’t make

4 foods to eat on an empty stomach in the morning to cleanse the gut, boost digestion, and lower cancer risk

Discover the Healing Power of Acupressure
Remedy For Falling Asleep Quickly
This Drink Destroys Your Bones From the Inside and Harms Every Organ on Its Way Out
Stop Ignoring These 8 Subtle Signs of Heart Trouble Before It’s Too Late
1 Teaspoon of Baking Soda Can Do This to Your Body!

Still Waking Up Tired? This Simple 3g Bedtime Mix Beats Melatonin for Deep Sleep

Here’s How to Starve Cancer to Death By Removing One Thing From Your Diet

This Super Tea Kills Parasites And Cleanses The Body of Toxins
News Post

Rafael Nadal’s Greatest Match: Fighting for Forgotten Dogs

The Officer, the Boy, and the Box of Pokémon Cards.

Grandma’s “Stray Cat” Turns Out to Be a Cougar.

The Walmart Employee Who Became a Hero to a Struggling Mom

Two Wounds, One Journey: The Woman and Dog Who Taught Each Other Grace

A Prom Filled With Love: Young Man’s Selfless Gesture Becomes Unforgettable

A Brother’s Sacrifice: How MJ Became a Hero in a Split Second

K-9 Apollo: A Hero’s Fight for Life and the Community That Saved Him

“One Last Climb: A Man, His Dog, and a Wheelbarrow Full of Love”

The Stranger Who Stopped: How One Man’s Kindness Saved a Puppy’s Life

Why You Should Avoid Leaving a Glass of Water Near Your Bed

Reason Why You Should Always Shower At Night

Place a plate of salted lemon at the head of the bed: Get 5 great benefits and secrets that unfortunately few people know

Add this to the water. Even when you don’t clean the floor in a week
💖 My Nana Knew What She Was Doing — Time-Honored Skincare Wisdom (And What Really Works Today)

Know this trick to distinguish real honey from fake honey, don't be afraid of being tricked into buying poor quality products
Add a few slices of fresh lemon to the pot of boiled eggs: Get great benefits, many people do not know

Extraordinary Visual Skills If You Can Spot The Cat
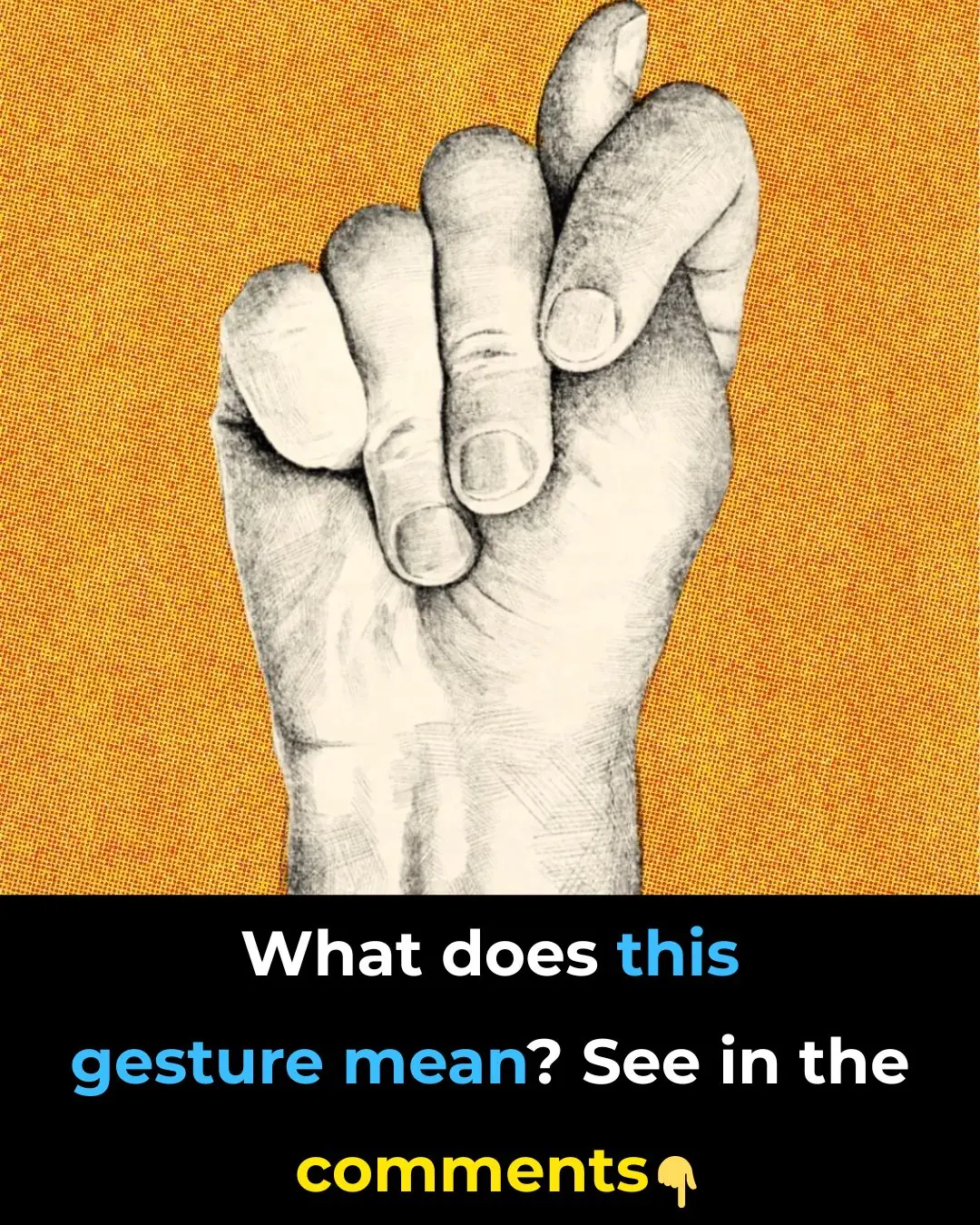
What does this gesture signify?
