A New Era in Immunotherapy: MIT’s Synthetic Gene Circuit Hunts Cancer with Unmatched Precision
Scientists at the Massachusetts Institute of Technology (MIT) have engineered an advanced synthetic gene circuit capable of programming immune cells to identify and destroy cancer with remarkable precision, while sparing healthy tissues. Inspired by the logic of electronic “AND” gates, this genetic system activates only when it detects two distinct tumor-specific molecular signatures, allowing it to distinguish cancer cells from normal ones far more accurately than many current immunotherapies. According to MIT researchers and reports from Nature Biotechnology and MIT News, this design aims to address one of the field’s most persistent challenges: preventing harmful off-target immune attacks.
The gene circuit is delivered using a harmless, non-replicating viral vector directly into the tumor environment, ensuring that its activity is tightly restricted to the cancer site. Once inside the tumor, the DNA program initiates a coordinated response. It produces proteins that help guide T cells toward malignant cells while simultaneously disabling the tumor’s built-in immune-evasion mechanisms—barriers that ordinarily prevent the body from mounting a strong defense. This dual strategy of precision targeting and immune-system amplification mirrors the multilayered approaches advocated in recent research from the National Institutes of Health (NIH) and leading oncology journals.
In preclinical testing, including controlled laboratory experiments and mouse models, the synthetic circuit demonstrated highly encouraging results. It successfully eradicated ovarian tumors without inflicting measurable damage on surrounding healthy tissues—an outcome that has long been difficult to achieve with traditional cancer treatments such as CAR-T therapy or immune checkpoint inhibitors. Even more promising, the researchers found that the circuit could be rapidly reprogrammed to recognize different cancer-specific markers, enabling it to target other types of tumors, including breast cancer. This adaptability, highlighted in reports from Science and the Journal of Clinical Investigation, suggests that the platform could one day support a new generation of customizable cancer interventions.
Beyond oncology, the MIT team envisions broader medical applications. Because the system can be tuned to respond to virtually any combination of genetic or molecular cues, it may eventually be adapted to treat autoimmune disorders, chronic inflammatory diseases, or conditions where precise control of immune activity is essential. By uniting genetic logic, targeted immune activation, and modular programmability, this synthetic gene-circuit strategy represents a significant step toward safer, smarter, and more personalized treatments—an approach that aligns with the growing movement in precision medicine advocated by the NIH and major biomedical research institutions.
If successful in future clinical trials, this technology could reshape how immune therapies are designed, offering not only greater anticancer potency but also unprecedented control and safety. MIT’s breakthrough demonstrates how synthetic biology, when combined with immunology and computational design principles, has the potential to transform modern medicine and create highly tailored therapies for patients worldwide.
News in the same category
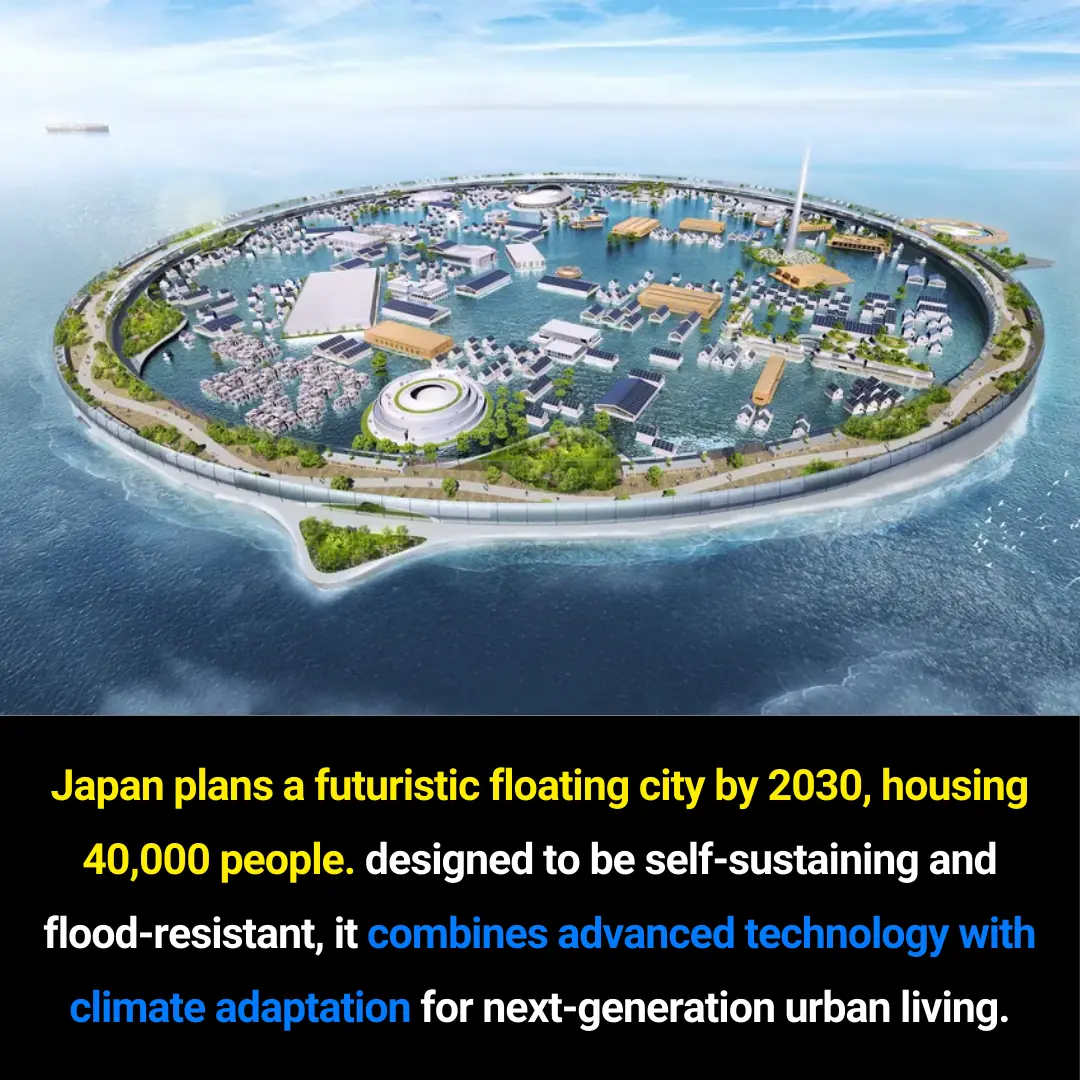
Experimental CAR-T Therapy Shows Dramatic 5-Day Regression of Glioblastoma at Massachusetts General Hospital
From Shortage to Supremacy: The Unexpected Rise of Vietnam’s Coffee Industry
Growing Concerns Over ADHD and Autism in Children: Insights, Challenges, and Evidence-Based Perspectives
Breakthrough Hydrogel Restores Damage in a Day, Mimicking Human Tissue
Inside the Science of Forgetting: How the Brain Downregulates Unwanted Memories
Surviving the Void: How Voyager 1 Still Operates Billions of Miles from Earth

The Bird’s Nest: A Tiny-Home Community Redefining Aging for Women in Texas
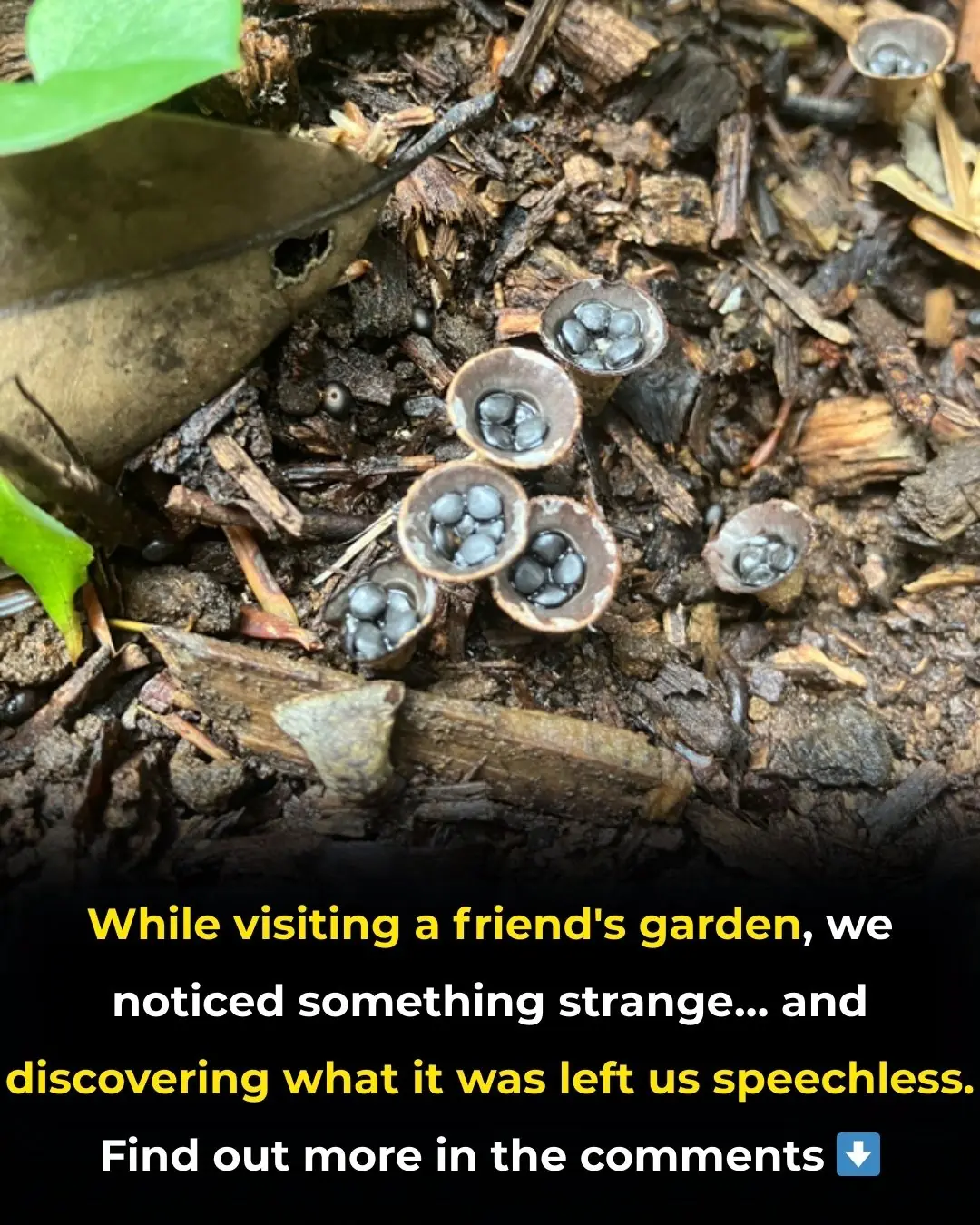
We Found Something Unexpected in the Garden

How to Know Your Rotisserie Chicken Is Truly Fresh
The HPV Vaccine Does Prevent Cervical Cancer, Scientists Confirm
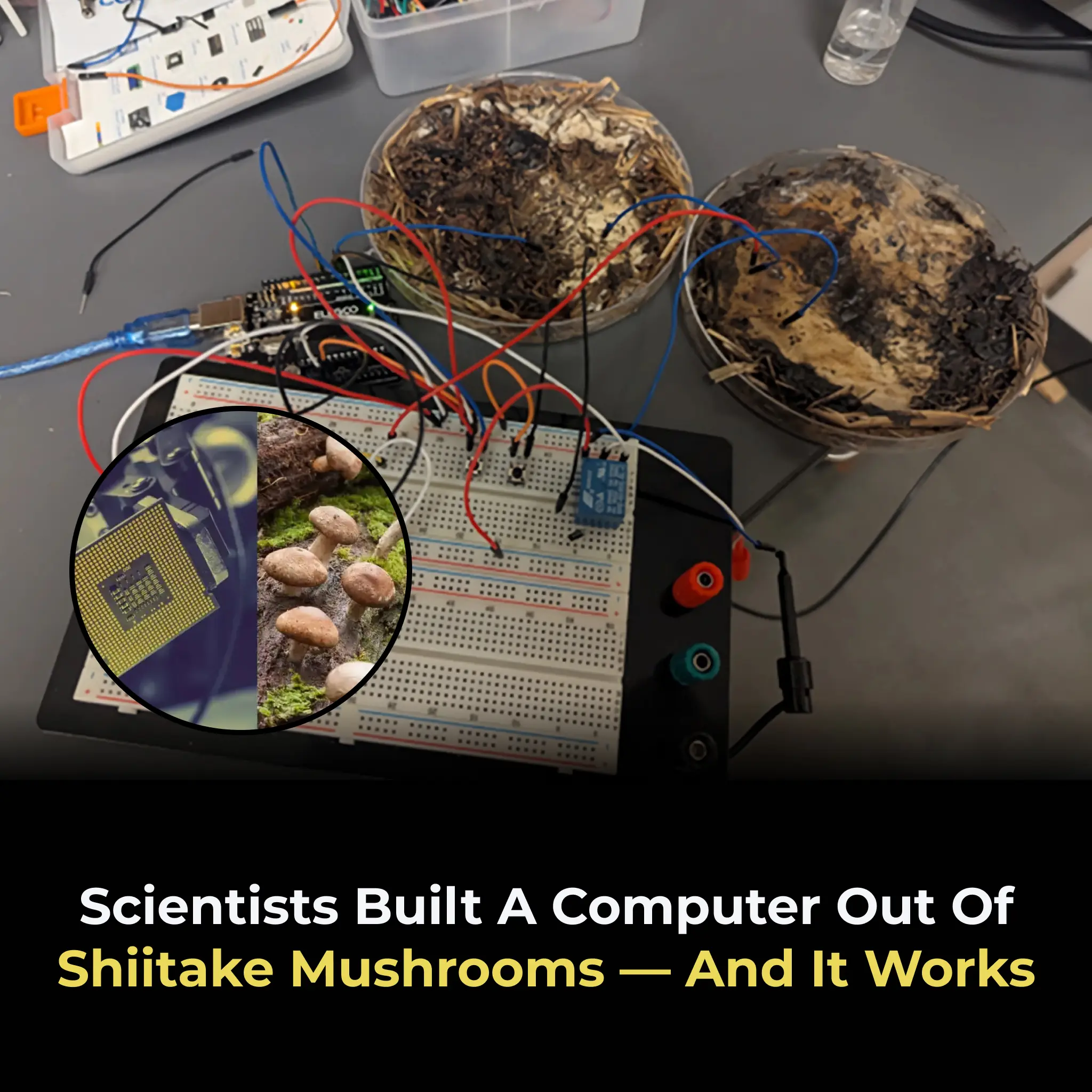
Scientists Built A Computer Out Of Shiitake Mushrooms — and It Works

Female Dogs Can Accurately Detect Levels of Human Incompetence

How Finland’s Libraries Became Models of Creativity, Sustainability, and Community Innovation

The Hidden Lymphatic System in the Brain: A Discovery That Redefines Modern Neuroscience

The 1943 Spearfish Temperature Shock: A Record-Breaking Weather Whiplash

How Dung Beetles Navigate by the Milky Way: A Breakthrough in Insect Celestial Orientation

Japan’s Johatsu: The Quiet Disappearance Phenomenon Behind a Culture of Privacy and Pressure
News Post

7 Powerful Bay Leaf Benefits for Heart Health and Smoother Blood Flow

Stop Counting Calories — The “100g Protein Rule” That Boosts Energy and Crushes Cravings

How Cats Use Smell and Earth’s Magnetic Field to Navigate Home Over Long Distances

10 Supplement Combinations You Should Never Take Together
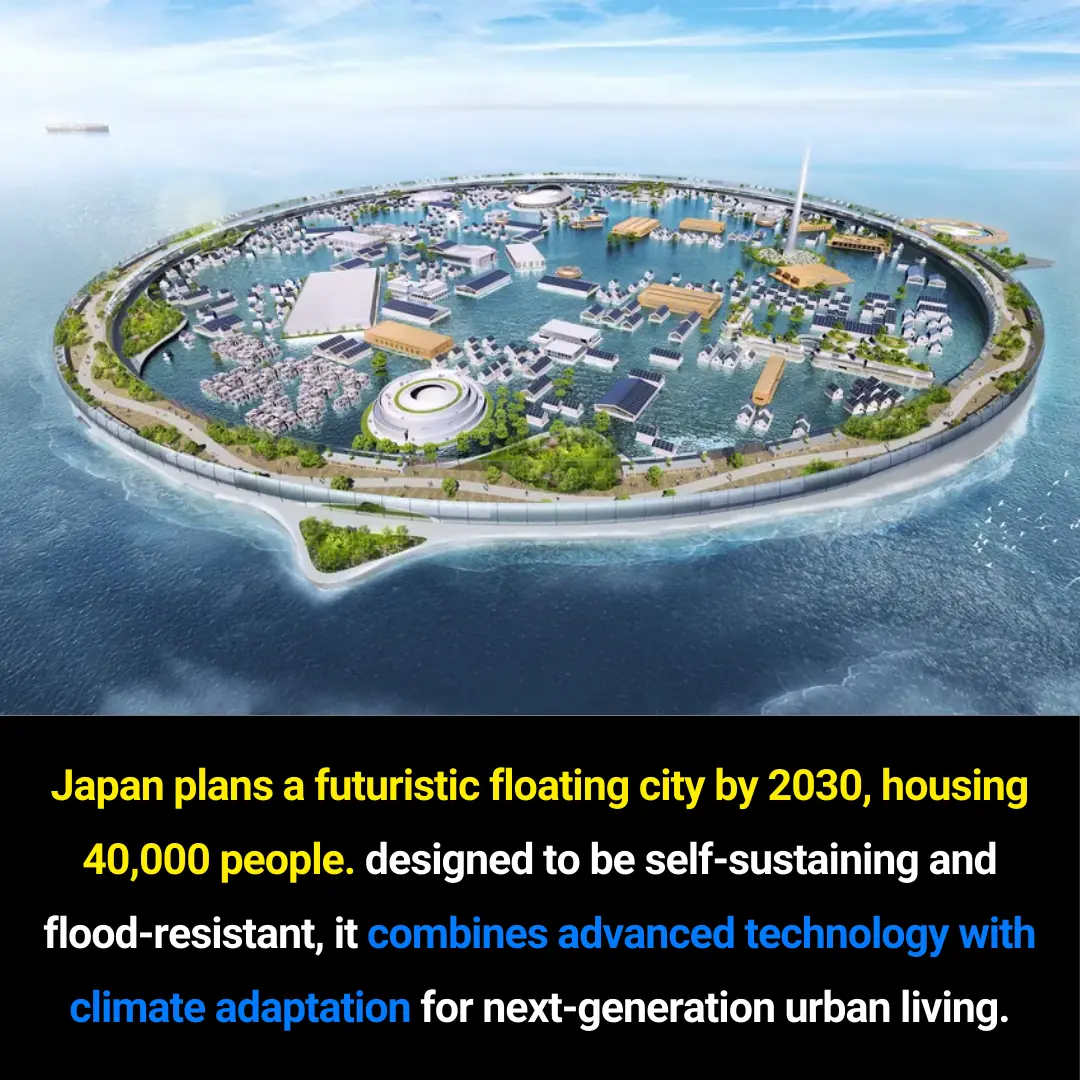
Japan’s Visionary Floating City: A Sustainable Urban Model for 2030 and Beyond
🦴 This Could Be the Vitamin Your Body Is Missing When Your Legs and Bones Hurt
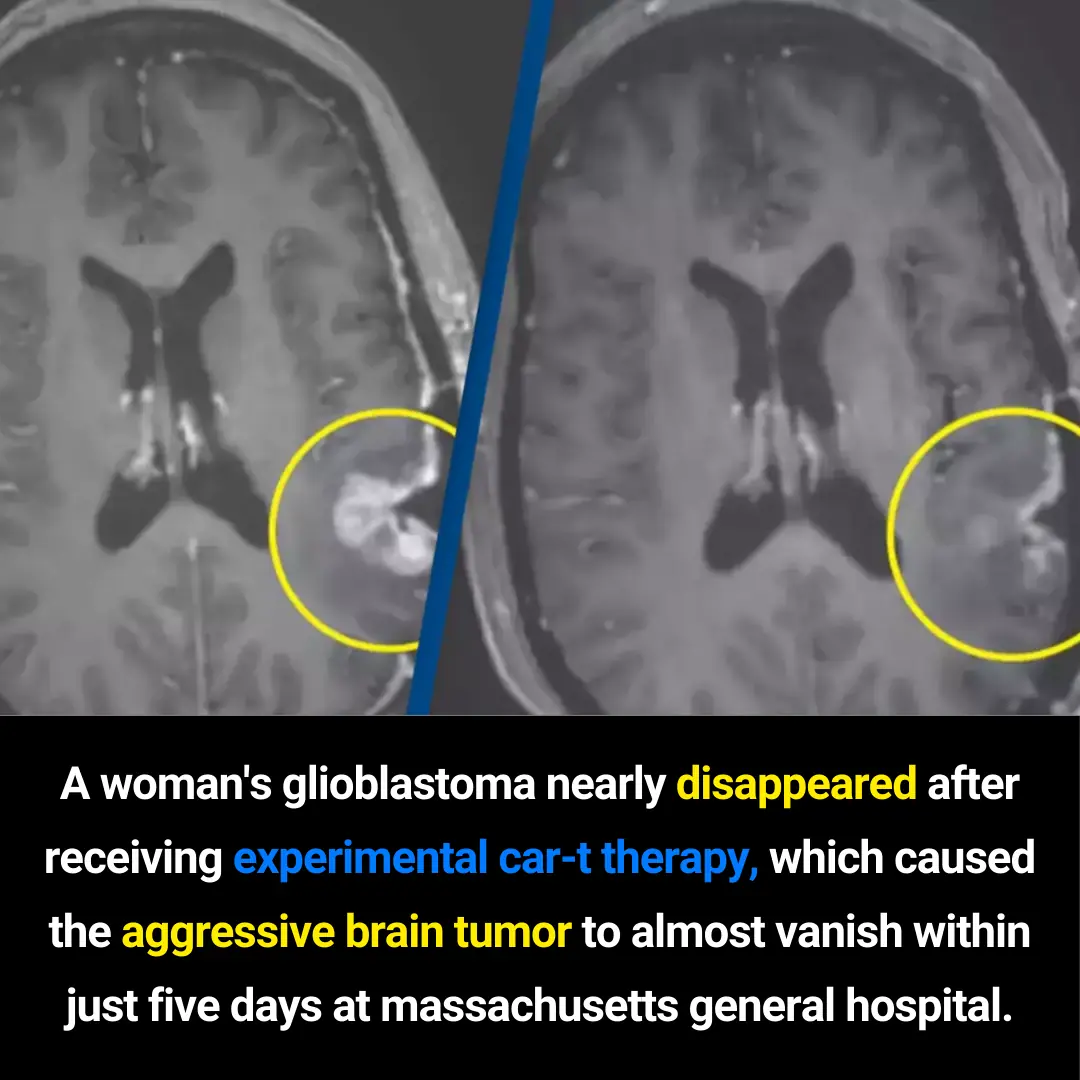
Experimental CAR-T Therapy Shows Dramatic 5-Day Regression of Glioblastoma at Massachusetts General Hospital
From Shortage to Supremacy: The Unexpected Rise of Vietnam’s Coffee Industry
Growing Concerns Over ADHD and Autism in Children: Insights, Challenges, and Evidence-Based Perspectives
Breakthrough Hydrogel Restores Damage in a Day, Mimicking Human Tissue
Inside the Science of Forgetting: How the Brain Downregulates Unwanted Memories
Surviving the Void: How Voyager 1 Still Operates Billions of Miles from Earth
6 Surprising Ways to Use Dishwasher Pods Around the House

Keep chilies fresh for months with this simple method — they’ll stay as vibrant and crisp as the day you picked them
Top 8 Longevity-Boosting Foods: Fish Only Ranks Second—And the #1 Food Might Already Be on Your Table

Remembering Saman Kunan: A Hero of Unwavering Courage

Goosegrass (Eleusine indica) and Stomach Pain: Can It Help or Hurt? The Complete Guide

The Bird’s Nest: A Tiny-Home Community Redefining Aging for Women in Texas
