All lupus cases may be linked to a common virus, study finds
A groundbreaking new study has unveiled one of the strongest connections to date between lupus—a chronic autoimmune condition—and the Epstein-Barr virus (EBV), a virus so widespread that nearly 95% of adults worldwide carry it. This discovery helps illuminate a long-standing medical mystery and could reshape the future of lupus diagnosis, prevention, and treatment for millions of people.
The research suggests that EBV doesn’t simply coexist with lupus; it may directly contribute to triggering the disease by altering critical parts of the immune system. Experts say this finding could be one of the most significant breakthroughs in autoimmune research in decades.
Key Takeaways
-
The Epstein-Barr virus (EBV) is strongly implicated as a major trigger for lupus.
-
EBV appears to reprogram immune cells in a way that causes the immune system to mistakenly attack the body’s own tissues.
-
This discovery opens doors to new lupus treatment strategies and strengthens the case for the development of an EBV vaccine.
Unraveling the Lupus Mystery
For years, scientists have struggled to identify a clear cause of lupus. The disease has long been believed to arise from a combination of genetic susceptibility, hormonal influences, and environmental triggers. EBV has always been suspected, partly because of its high prevalence and its documented association with multiple autoimmune disorders, including multiple sclerosis and rheumatoid arthritis.
However, despite decades of suspicion, researchers lacked clear evidence of how the virus might spark autoimmune chaos—until now. This new study provides some of the most compelling mechanistic data ever published, showing that EBV may actively push the immune system toward the out-of-control response seen in lupus. The research gives scientists a clearer picture of the disease’s origin and strengthens the theory that EBV is not simply correlated with lupus—it may be a driving factor.
How EBV Triggers Lupus
EBV is best known for causing mononucleosis (“mono”), but the virus remains in the body for life, typically hiding inside B cells—white blood cells responsible for creating antibodies. In most people, EBV stays dormant and relatively harmless. But in individuals with a certain genetic or immune profile, the virus appears to do something far more dangerous.
The study shows that EBV can reprogram infected B cells, activating genes that push these cells into a highly inflammatory, abnormal state. These reprogrammed B cells begin producing antinuclear antibodies (ANAs)—a hallmark of lupus. ANAs mistakenly attack the nucleus of the body’s own cells, initiating chronic inflammation and tissue damage across organs such as the skin, joints, kidneys, and brain.
Researchers discovered that people with lupus have a significantly higher number of EBV-infected B cells compared to healthy individuals. This suggests that EBV may serve as a “spark,” awakening dormant autoreactive B cells and driving them into autoimmune overdrive.
This finding gives scientists the closest look yet at the potential origin point for the autoimmune reaction that defines lupus.
Implications for Treatment and Prevention
Identifying EBV as a potential root cause of lupus represents a massive shift in how researchers might approach future treatments. Today’s lupus medications mainly aim to suppress the immune system, control inflammation, and manage flare-ups. While these treatments can be effective, they do not address an underlying viral trigger.
With this new information, scientists can begin to explore more targeted and precise therapies, potentially focusing on:
-
eliminating EBV-infected B cells
-
blocking the viral genes that hijack immune cells
-
preventing EBV reactivation
-
interrupting the inflammatory signaling pathways initiated by the virus
The findings also add weight to ongoing efforts to develop an EBV vaccine. While such a vaccine would not cure lupus in individuals who already have it, it could help prevent EBV infection in the first place—possibly lowering the global incidence of autoimmune conditions linked to the virus. Several biotech companies are already working on early EBV vaccine candidates, some inspired by the rapid development of mRNA technology.
Interestingly, some experimental treatments, such as CAR T-cell therapy—which essentially “reboots” the immune system by eliminating certain B cells—have shown remarkable success in severe lupus cases. This new study provides a possible explanation: by removing B cells, these treatments may also be removing EBV-infected cells, indirectly shutting down the viral trigger.
Future Directions
Although this study represents a major step forward, experts emphasize that lupus is a complex, multifaceted disease. EBV may be a key trigger, but likely not the only one. Genetics, hormones, immune history, and environmental exposures still play crucial roles in shaping who develops lupus and how severe it becomes.
Future research will likely focus on:
-
mapping the exact molecular pathways EBV uses to reprogram B cells
-
examining why only certain individuals react to EBV in this autoimmune way
-
evaluating antiviral therapies and EBV-targeted treatments in lupus patients
-
tracking the long-term impact of EBV vaccines on autoimmune disease rates
What is clear, however, is that this discovery marks one of the most promising turning points in lupus research. By understanding the viral roots of autoimmune dysfunction, scientists may finally be able to develop more effective treatments—and, potentially, prevent the disease from taking hold in the first place.
News in the same category

Doctors warn: these everyday antacids could be putting your heart in danger

Doctors Reveal What Really Happens When You Use Castor Oil

The Natural Secret Doctors Never Tell You That Melts Away Uric Acid Fast
9 Convincing Reasons to Consume More Dates
Two handfuls of peanuts daily boost memory in 4 months

Prunes and bone health: surprising benefits beyond constipation relief
12 Weird Diabetes Skin Problems You Need To Know

High Cholesterol: Causes, Risks, and Natural Ways to Lower It
Acid Reflux (GERD): When Should You See a Doctor?
Hypothyroidism: The Silent Condition With Easily Overlooked Symptoms
3 pain areas on your body that might be early cancer warning signs

A New Era of Near Vision Clarity Through VIZZ Eye Drops

Vaping harms your heart more than you realize
Ever Wake Up But Can’t Move

Gout Disease: The Untold Truth and 5 Common Treatment Mistakes
Arthritis Explained: Types, Causes, and Natural Pain Relief Methods
High Blood Pressure: Why It’s Dangerous and How to Stabilize It Naturally
MEDICATIONS YOU SHOULD NEVER TAKE WITH COFFEE
10 Best Foods to Detox Your Kidneys and Protect Renal Health
News Post

A Nearby Earth-Sized World Raising New Hopes for Habitability

How Finnish Forest Kindergartens Let Kids Thrive in Any Weather
Taiwan Researchers Develop Promising Hair-Regrowth Serum With Dramatic Lab Result
Pick the Breakfast You’d Eat

What Happens to Your Body When You Eat Canned Tuna Every Day

Why Some Children Don’t Visit Their Parents Often
The Hidden Fish Puzzle That’s Stumping the Internet
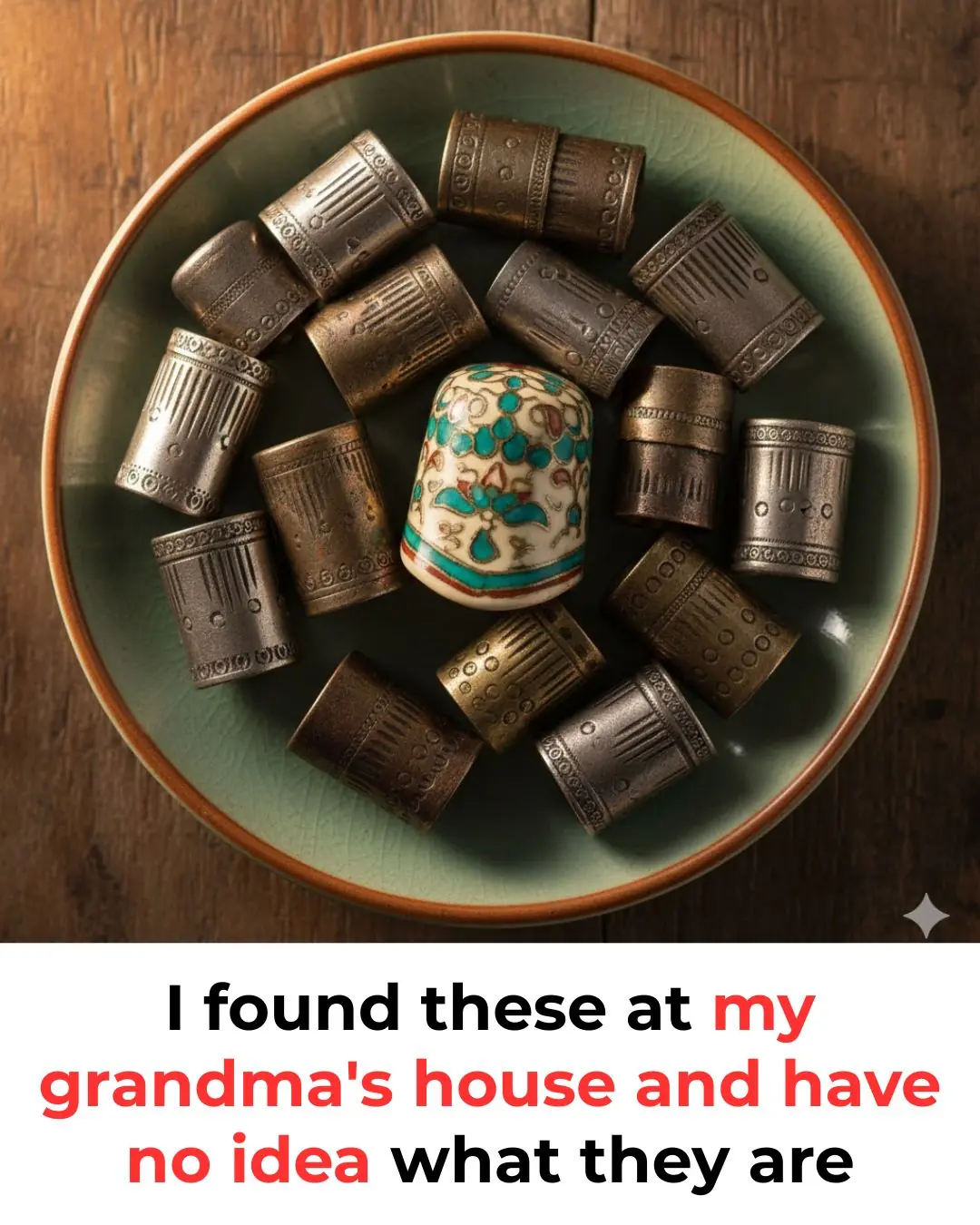
So this is what it does, here is the answer

The Hidden Details in Women’s Underwear — And What They Really Mean

Experts reveal that eating bananas in the morning cause

Why Cutting Your Own Hair Is About More Than Just Saving Money

Why Are Tree Trunks Painted White

Penguins Reject Cheaper Fish as Japanese Aquarium Tries to Cut Costs

I Thought I Found Insect Eggs Under My Bed

This is the correct way to wash grapes; washing them wrong can make them even dirtier

Emirates Airlines: A Legacy of Unmatched Safety and Reliability in Aviation

Dragon Bravo Fire: Arizona's Megafire Threatens the Grand Canyon and Beyond
The zodiac signs with a supernatural sixth sense… See now

Mussel Beds: New Zealand's Natural Solution for Ocean Health and Sustainability