
Are You Being Lied To About What Your Blood Pressure Should Be? — Read This Before You “Chase the Number”
Are You Being Lied To About What Your Blood Pressure Should Be? — Read This Before You “Chase the Number”
What If Everything You’ve Been Told About “Normal” Blood Pressure Isn’t the Full Story?
For decades, we’ve all been taught that 120/80 mmHg is the “perfect” blood pressure — the gold standard for heart health. It’s printed on posters, repeated in doctor’s offices, and drilled into public awareness as the number to aim for.
But what if that number isn’t perfect for you? What if, in some cases, chasing it could actually cause more harm than good?
It sounds counterintuitive, but mounting evidence shows that blood pressure isn’t one-size-fits-all. Your body, age, and metabolism are unique — and the rigid pursuit of a single number for every human being, regardless of their circumstances, is an oversimplified and potentially dangerous idea.
This article isn’t about denying the very real risks of high blood pressure. It’s about challenging the culture of over-treatment — where we chase textbook targets instead of listening to our bodies. With insights inspired by internal medicine expert Dr. Suneel Dhand, let’s unpack what your numbers really mean, how modern medicine got too rigid, and how to take back control of your own cardiovascular health.

Key Takeaways
-
The “120/80” goal isn’t universal. Blood pressure naturally changes with age, health, and lifestyle. What’s optimal for a 25-year-old might be too low for a 75-year-old.
-
Over-treatment is real and risky. Forcing your blood pressure too low can cause dizziness, confusion, and even harm your brain and kidneys by restricting blood flow.
-
Your ideal pressure evolves with age. As arteries stiffen over time, slightly higher numbers may actually ensure proper oxygen delivery to vital organs.
-
Home monitoring empowers you. Learning to track your blood pressure correctly at home gives you more accurate data and helps you have better conversations with your doctor.
-
Lifestyle trumps prescriptions. Diet, movement, sleep, and stress management are the most powerful tools for lifelong blood pressure balance.
-
Be your own health advocate. Ask questions, challenge assumptions, and ensure your treatment plan fits you — not just the guideline.
1. What Do Your Blood Pressure Numbers Really Mean?
When you get a reading like 120/80 mmHg, it measures two forces inside your arteries:
-
Systolic (the top number): Pressure when your heart beats and pumps blood through your arteries.
-
Diastolic (the bottom number): Pressure when your heart relaxes between beats.
Think of it as the rhythm between push and rest. Both numbers matter — but most attention is usually given to the systolic pressure because it rises more noticeably with age.
Understanding these numbers isn’t just about memorizing digits. It’s about realizing that pressure is how your body ensures blood reaches every cell. Too high for too long? It strains the arteries. Too low? Your organs don’t get the oxygen they need. The sweet spot depends on your physiology, not a chart on a wall.
2. The Trap of “Guideline Rigidity” — When Medicine Treats Numbers, Not People
Medical guidelines are helpful. They give doctors a shared framework for treating disease. But when those guidelines turn into rules without nuance, we stop treating people — and start treating paper targets.
The idea that a 25-year-old marathon runner and an 85-year-old grandmother should both have a blood pressure of 120/80 is, frankly, absurd. Yet that’s often how the system works.
This “number-chasing” mentality has led to millions of people being aggressively medicated even when they feel fine, with no regard for symptoms, context, or quality of life. As Dr. Dhand points out, the goal should be healthy function, not arbitrary perfection.
3. The Hidden Dangers of Blood Pressure That’s Too Low
We talk endlessly about high blood pressure, but low blood pressure — often caused by over-medication — is just as dangerous and far less discussed. When your pressure drops too far, your vital organs simply aren’t getting the blood and oxygen they need.
This state, known as under-perfusion, can cause:
-
Dizziness and lightheadedness
-
Blurred vision or “brain fog”
-
Weakness and chronic fatigue
-
Confusion or memory loss
-
Increased risk of falls and fractures, especially in older adults
Your brain and kidneys are especially vulnerable. Reduced blood flow to the brain can mimic dementia symptoms, while the kidneys — which already decline in function with age — can deteriorate faster when they’re under-perfused. Ironically, the very medications meant to “protect” your organs can end up damaging them if dosed too aggressively.
4. Why Age and Physiology Matter
As you get older, your arteries naturally stiffen — a process called arteriosclerosis. Think of it as trying to pump water through a stiff pipe instead of a flexible hose. To keep blood flowing to your organs through those stiffer arteries, your body sometimes needs a bit more pressure.
That’s why, for many older adults, a systolic pressure in the 130s or 140s might be perfectly normal — even optimal. Studies have even found that in people over 85, those with systolic readings around 150 mmHg sometimes lived longer than those forced into the 110s.
This doesn’t mean “higher is better,” but it proves the danger of the blanket “lower is always best” approach. A moderate increase can be your body’s healthy adaptation — not a disease.
5. The Over-Medication Epidemic: When Good Intentions Go Wrong
Take this real-world story: A 78-year-old man who’d been on blood pressure medication since his 40s gradually began feeling dizzy, sluggish, and “foggy.” One morning, after breakfast, he nearly fainted. When checked, his systolic blood pressure was in the 70s — a dangerously low level.
After reviewing his history, doctors discovered years of medication stacking: every new physician added another drug but rarely removed one. Once his regimen was simplified, his symptoms vanished, and his energy returned.
This is called polypharmacy — the piling on of drugs without proper re-evaluation. It’s one of the most under-acknowledged public health crises, fueled by a medical system focused more on numbers than on people’s daily well-being.
6. How to Take Back Control: Become Your Own Data Source
If you’re on blood pressure medication, the smartest step you can take is to measure your blood pressure accurately at home. This puts you in control and gives you reliable data that reflects your real-life readings — not just the stress-induced ones at the clinic.
Here’s how to do it right:
-
Choose the right device. Use an upper-arm cuff (brands like Omron are well-validated). Avoid wrist or finger monitors — they’re less accurate.
-
Set the scene. Sit comfortably for at least five minutes before measuring. No coffee, smoking, or exercise 30 minutes beforehand. Keep your arm at heart level.
-
Take multiple readings. Do three measurements, one minute apart, and average them.
-
Track your trends. Record readings twice a day (morning and evening) for two weeks, then share the log — and your device — with your doctor.
By monitoring consistently, you and your doctor can make smarter, more personalized adjustments to your treatment.
7. “White Coat Hypertension” — Real, But Not an Excuse
Ever notice your blood pressure seems higher at the doctor’s office? That’s white coat hypertension, caused by anxiety or stress during the visit. It’s very common — and a perfect example of why context matters.
If your readings are high in the clinic but normal at home, your doctor may choose to observe rather than medicate immediately. Still, don’t ignore elevated numbers entirely — confirm the trend with home monitoring or ambulatory testing.
A good tip: ask your doctor to re-check your blood pressure after your appointment, when you’ve relaxed. The difference can be dramatic.
8. The True Solution: Fixing the Root Cause of High Blood Pressure
For most people, high blood pressure isn’t caused by a “medication deficiency.” It’s a symptom of metabolic imbalance — most often driven by insulin resistance, poor diet, stress, and inactivity.
The beauty is that it’s reversible. The pillars of heart health are within your control:
-
Eat whole, unprocessed foods. Focus on vegetables, lean proteins, healthy fats, and low-glycemic carbs.
-
Move daily. Even a 20-minute brisk walk can lower blood pressure and improve insulin sensitivity.
-
Sleep deeply. Less than seven hours a night increases stress hormones and blood pressure.
-
Manage stress. Meditation, nature walks, and deep breathing all lower sympathetic nervous activity — your body’s “fight or flight” mode.
When you optimize these habits, your blood pressure often normalizes naturally — sometimes to the point where you can safely reduce medication (always under your doctor’s supervision).
Conclusion: You Are Not a Number
It’s time to move beyond the industrial, “assembly-line” approach to medicine. You are not a statistic, and your ideal blood pressure shouldn’t be decided by a generic chart.
If your numbers look perfect on paper but you feel tired, dizzy, or unwell, that is not optimal health. Your true goal should be vibrant energy, clear thinking, and a body that feels balanced — not simply chasing “120/80.”
Ask questions. Stay curious. Bring your data. Partner with a physician who listens. And remember: the healthiest blood pressure is the one that supports you — not the one that satisfies a textbook guideline.
News in the same category


SHOCKING NEW STUDY REVEALS WHAT MIGHT BE SILENTLY DESTROYING HUMAN FERTILITY

POPULAR SHAMPOO URGENTLY RECALLED BECAUSE IT CONTAINS BACTERIA THAT KILLS UP TO ONE IN TEN PATIENTS

Nurse who's witnessed 'so many deaths' explains spine-chilling moment she realised 'what happens after we die'
The influenza flu virus is being used to cure pancreatic cancer

Eye Doctor Reveals What To Do If You Start Seeing ‘Floaters’
If cancer cells are present in the body, these 3 symptoms often appear in the morning everyone should pay attention

3 foods you thought were bad for diabetes (but aren’t!)

CANCER IS PAINLESS AT FIRST, BIT IF YOU SEE THESE 8 SIGNS WHEN GOING TO THE TOILET, YOU SHOULD SEE A DOCTOR IMMEDIATELY
Sleeping Naked: 8 Surprising Benefits

What Happens To Your Skin When You Rub An Ice Cube On Your Face

🤢 The Real Causes of Constant Phlegm and Mucus in Throat — And How to Get Rid of It

The Tennis Ball Trick That Can Relieve Back, Neck Or Knee Pain In Seconds

One scoop a day heals your body from the inside out — watch what happens

🧠 A Stroke Can Happen Suddenly — But Your Body Might Send Early Warnings (Know the Signs)

The 7 silent causes of bad leg circulation
4 simple moves after eating that flatten blood sugar spikes

This Miraculous Drink Will Work Wonders for Your Thyroid

This Starves Colon Cancer Cells — and Strengthens Your Body’s Natural Defenses
News Post
Tragus Piercing What Does It Mean

9 Health Benefits of Pine Needles

Unlock The Incredible Health Benefits of Garlic, Ginger and Lemon for Men

A special method to grow garlic in plastic bottles

7 Benefits of the Miracle Leaf of Life

7 Amazing Health Benefits of Banana Blossoms

Boiling Sweet Potatoes: Don’t Just Add Plain Water—Add This Spoonful for Perfectly Fluffy, Sweet Results

The Science Behind Putting a Cotton Swab in a Menthol Oil Bottle

More People Are Struggling with Visceral Fat — Doctors Reveal 9 Foods That Help Burn It Naturally
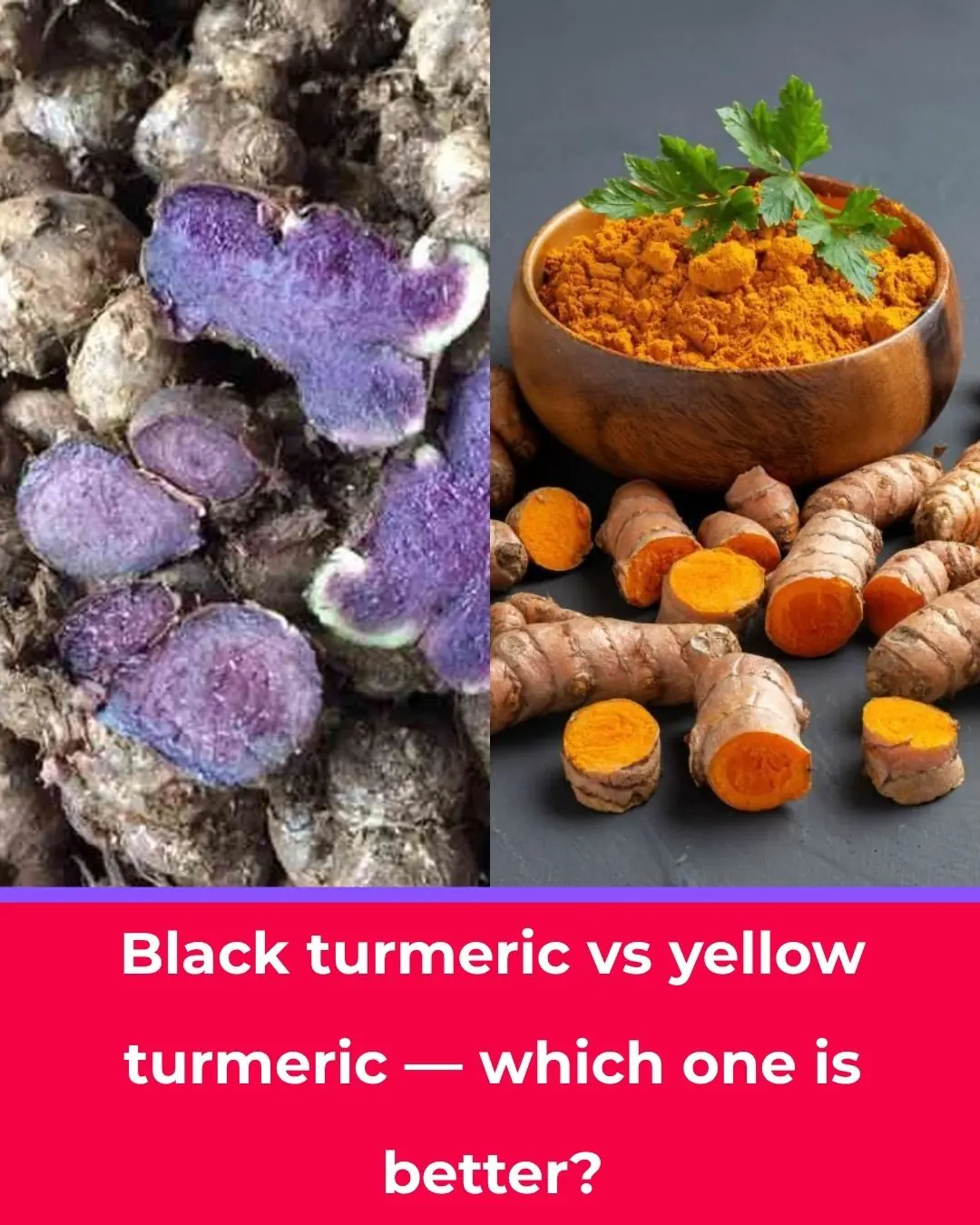
Black Turmeric vs. Yellow Turmeric: Which One Is Better?

Starve cancer: the diet rotation strategy you need to know

Like to see more from Tips for the Home
💪 Sarcopenia: Why Muscle Loss Happens & How to Fight It (After 50)
I Had No Idea About This!

These Ideas Are Amazing: 10 Clever Ways to Use Dryer Sheets Beyond the Laundry Room

Most Don’t Know: 13 Brilliant Ways to Use WD-40 Around the House

Garlic Mustard: The Overlooked Herb That Can Boost Your Health — Especially Your Eyes

SHOCKING NEW STUDY REVEALS WHAT MIGHT BE SILENTLY DESTROYING HUMAN FERTILITY

POPULAR SHAMPOO URGENTLY RECALLED BECAUSE IT CONTAINS BACTERIA THAT KILLS UP TO ONE IN TEN PATIENTS
