Cell Therapy Begins Human Trials to Reverse Spinal Cord Injury
For decades, the phrase “spinal cord injury” carried a profound sense of permanence. Doctors often delivered the diagnosis with heavy hearts, explaining that once neural pathways were severed, they could never regenerate. Families prepared for lifelong paralysis, wheelchairs, and a future reshaped by limitations. Yet in research centers across Shanghai and Suzhou, a group of scientists refused to accept this long-standing medical verdict.
In May, something extraordinary happened—an event that captured the attention of the global medical community. Regulatory authorities in both the United States and China made a historic, near-unprecedented decision: the FDA and China’s National Medical Products Administration simultaneously approved a groundbreaking clinical trial. Experts had been waiting for years for this moment. What they authorized was not just another experimental therapy—it was the first real attempt to reverse paralysis by transforming ordinary adult cells into regenerative neural tissue.
Hidden within this decision lies a discovery that challenges everything medicine once believed about the nervous system’s inability to heal. The upcoming trial could rewrite medical textbooks and, more importantly, reshape the futures of millions of people whose lives changed in an instant.
Global Regulators Approve a Historic Medical Breakthrough
XellSmart Biopharmaceutical achieved what few biotech companies ever attain: simultaneous approval from both the U.S. FDA and China’s NMPA for a first-in-class therapy targeting spinal cord injury. Such dual authorization is extremely rare, reflecting extraordinary confidence in the scientific foundation behind the treatment.
The approved Phase I trial will evaluate XS228, the world’s first registrational clinical trial involving an off-the-shelf, allogeneic, iPSC-derived, subtype-specific regenerative neural cell therapy for spinal cord injury. The terminology may seem technical, but at its core, it represents over a decade of innovation in stem-cell engineering and regenerative neuroscience.
The trial will be led by the Third Affiliated Hospital of Sun Yat-sen University, a global leader in spinal cord injury research. The institution brings decades of clinical experience, advanced rehabilitation programs, and a strong track record in neurological recovery studies.
Regulators approved the study only after extensive preclinical evidence demonstrated promising results in animal models, ensuring that the therapy appeared both safe and scientifically plausible. This milestone marks the culmination of more than four years of rigorous development, safety testing, and manufacturing optimization.
A Global Health Crisis: Millions Living with Spinal Cord Injuries
More than 15 million people worldwide currently live with spinal cord injuries—an often overlooked but devastating public health challenge. These injuries typically strike young and middle-aged adults during the most active years of their lives.
Traffic accidents are the leading cause, followed by sports injuries, industrial accidents, and falls. The impact is immediate and life-altering: many victims lose sensation, mobility, and independence within seconds.
According to XellSmart’s data, China sees about 100,000 new spinal cord injury cases every year, while the United States reports roughly 18,000—equivalent to nearly one new case every hour in China and two every hour in the U.S.
Current treatments focus on stabilizing the spine and preventing additional damage. Rehabilitation helps patients adapt to new limitations but cannot restore lost neural function. For decades, the inability of the central nervous system to regenerate has made meaningful recovery seem impossible.
Turning Adult Cells Into Hope: The Power of iPSC Technology
XS228 relies on induced pluripotent stem cell (iPSC) technology, a scientific breakthrough that makes it possible to reprogram normal adult cells—often simple skin cells—into stem cell–like cells capable of becoming almost any cell type.
Through advanced laboratory processes, these reprogrammed cells are guided into neural progenitor cells that can differentiate into the exact types of motor neurons destroyed in spinal cord injuries.
Key advantages include:
-
Off-the-shelf availability: The cells come from healthy donors, so treatment does not depend on harvesting cells from each patient.
-
Scalability: Large batches can be manufactured and stored, making rapid deployment possible.
-
Precision engineering: The cells are designed to become subtype-specific neurons, offering targeted restoration rather than generalized repair.
XellSmart describes its mission clearly: “to redefine possibilities for SCI recovery and bring new hope to patients.”
This standardized production method could one day make advanced neural regeneration therapies accessible worldwide, not just in elite hospitals.
Animal Studies Reveal Remarkable Recovery Potential
In preclinical testing, XS228 demonstrated the ability to integrate into injured spinal cord tissue and begin forming new neural circuits. Treated animals showed encouraging signs of regaining movement control as transplanted cells extended axons and connected with existing nerve pathways.
The therapy’s subtype-specific design ensures that implanted cells become the precise neuron types required for functional recovery, strengthening the biological rationale behind human trials. Researchers also monitored immune responses to ensure safety across genetically diverse recipients.
The Clinical Trial: Testing Safety and Early Effectiveness in Humans
The Phase I human trial will enroll about 60 recent spinal cord injury patients, as early treatment may yield better regenerative outcomes.
Participants will be randomly assigned to receive either XS228 or a placebo, following strict double-blind protocols. Over six months, doctors will monitor improvements in mobility, sensation, bladder and bowel function, and overall quality of life.
The primary goal is safety, as with all first-in-human studies. If successful, the therapy could progress to Phase II trials around 2028, involving hundreds of patients and more extensive functional assessments.
XellSmart’s Leadership in Regenerative Neuroscience
XellSmart has become a global pioneer in iPSC-based therapies for central nervous system disorders, with seven approved clinical trials across conditions such as Parkinson’s disease and ALS. Early results in these areas have shown encouraging safety and preliminary signs of therapeutic benefit.
Supported by investors such as Sequoia Capital China and Qiming Venture Partners, the company operates a cutting-edge, 5,000-square-meter GMP-compliant cell therapy manufacturing center. Its expertise in large-scale cell production is a major advantage in a field where many competitors struggle with consistency and cost.
In 2023, XellSmart became the first Chinese company to earn FDA approval for an iPSC-derived therapy and received global orphan drug designation for its ALS treatment.
Why Previous Treatments Failed—and Why XS228 Might Succeed
Over past decades, researchers attempted numerous strategies to repair spinal cords, including embryonic stem cells, gene therapy, electrical stimulation, and biomaterial scaffolds. Many approaches showed promise but could not progress to human trials due to safety concerns, ethical issues, or limited efficacy.
XS228 stands apart because:
-
It uses iPSC-derived cells that can be ethically sourced and manufactured at scale.
-
The cells are subtype-specific, meaning they replace exactly the neurons that spinal injuries destroy.
-
Advances in cell engineering and immune-profiling greatly reduce rejection risks.
These breakthroughs create a scientific foundation that was not available to earlier generations of researchers.
Off-the-Shelf Cell Therapy: Expanding Access Worldwide
Because XS228 uses donor-derived, universal cells, it eliminates the need for patient-specific manufacturing. This innovation allows:
-
Immediate treatment after injury
-
Lower overall treatment costs
-
Global distribution to hospitals
-
Faster clinical adoption if trials succeed
Should the therapy prove effective, it could reach widespread clinical use within five to seven years, transforming emergency care for spinal injuries.
The Long Road Ahead
Phase I results are expected next year, offering the first real indication of whether XS228 can safely integrate into the human spinal cord. If successful, larger trials will follow, each requiring meticulous evaluation over several years.
Although setbacks are possible—cell therapies are complex and technically demanding—researchers remain cautiously optimistic. Many promising treatments never make it through clinical development, but XS228 represents the most sophisticated and scientifically grounded attempt yet.
Regenerating the Central Nervous System: A Scientific Frontier
Nerve regeneration has long been one of medicine’s greatest challenges. Unlike skin, bone, or muscle, the central nervous system has almost no natural ability to heal itself.
iPSC technology is now pushing the boundaries of regenerative medicine, enabling the development of retinal cells for blindness, cardiac cells for heart failure, and now neuronal cells for spinal cord repair.
Success in spinal injury treatment would reshape how we approach stroke, traumatic brain injury, and neurodegenerative diseases.
Economic and Human Impact
The lifetime cost of caring for someone with a severe spinal cord injury can exceed $1 million, not including lost productivity or the emotional toll on families. Many patients face long-term unemployment, isolation, and mental health struggles.
A therapy that restores even partial mobility could significantly reduce healthcare costs, allow more patients to return to work, and dramatically improve quality of life.
A Future Where Walking Again Is Possible
XellSmart’s XS228 trial represents more than a scientific milestone—it embodies the hope of millions. By 2026, Phase I results will reveal whether these lab-grown neural cells are safe in humans. If progress continues, full-scale trials could begin by 2028, moving us closer to the day when paralysis is no longer a life sentence.
The journey ahead will not be easy, but the possibility of restoring movement drives researchers forward. This trial may redefine recovery not just for spinal cord injuries but for a wide range of nerve-related conditions.
Imagine a world where paralysis is not permanent.
That world may be closer than we ever thought.
News in the same category
Overripe Bananas Could Help Fight Cancer Naturally

Chinese Scientists Created a ‘Bone Glue’ That Repairs Fractures in Minutes With a Single Injection
Could a Nearly Universal Virus Be the Root Cause of Lupus
Castor Oil for Peripheral Neuropathy Relief: A Natural Remedy Worth Trying?
The New Science Behind Killing Cancer

Beware: U.S Salmon May be Crawling with Japanese Tapeworm, Say Scientists
How to Use Guava for Eye Comfort | Natural Remedies for Healthy Eyes

Top 10 foods that improve blood circulation in legs

Orthopedist’s Secret: How to Support Natural Cartilage Repair in Just 24 Hours
15 visible signs of low thyroid you can see – don’t ignore #7!
The new vitamin D findings forcing experts to rethink heart health
Diabetes? Just Boil These Leaves to Lower Blood Sugar (Without Medications!)

These 9 Nutrients Will Shockingly Heal Nerve Damage!
6 Physical Changes That Happen When Your Heart is In Serious Danger
5 Common Habits That Quietly Damage Your Kidneys

Rosemary Tea: Drink It for 15 Days and See What Happens

What happens to the body after gallbladder removal? 3 diseases that may follow — avoid surgery if possible
News Post
10 Amazing Health Benefits of Dates (and Why You Need To Start Eating Them!)

The Surprising Truth: Wooden Boards Kill Bacteria Better Than Plastic
Overripe Bananas Could Help Fight Cancer Naturally

When frying eggs, don't just add onions: Combine with these two types of leaves, both delicious and good for your health.

Chinese Scientists Created a ‘Bone Glue’ That Repairs Fractures in Minutes With a Single Injection

Making pickled eggplant must know this secret to keep the white eggplant crispy and keep it from getting scum.
Could a Nearly Universal Virus Be the Root Cause of Lupus

Mattresses used for a long time are dirty and smelly. Sprinkle this on the surface and it will be clean as new without washing.

Don't throw away sprouted potatoes, do it this way, it's surprisingly effective

Add this handful of leaves to the fish stew pot: The fish will be soft, no longer fishy, and have a beautiful color.
Castor Oil for Peripheral Neuropathy Relief: A Natural Remedy Worth Trying?
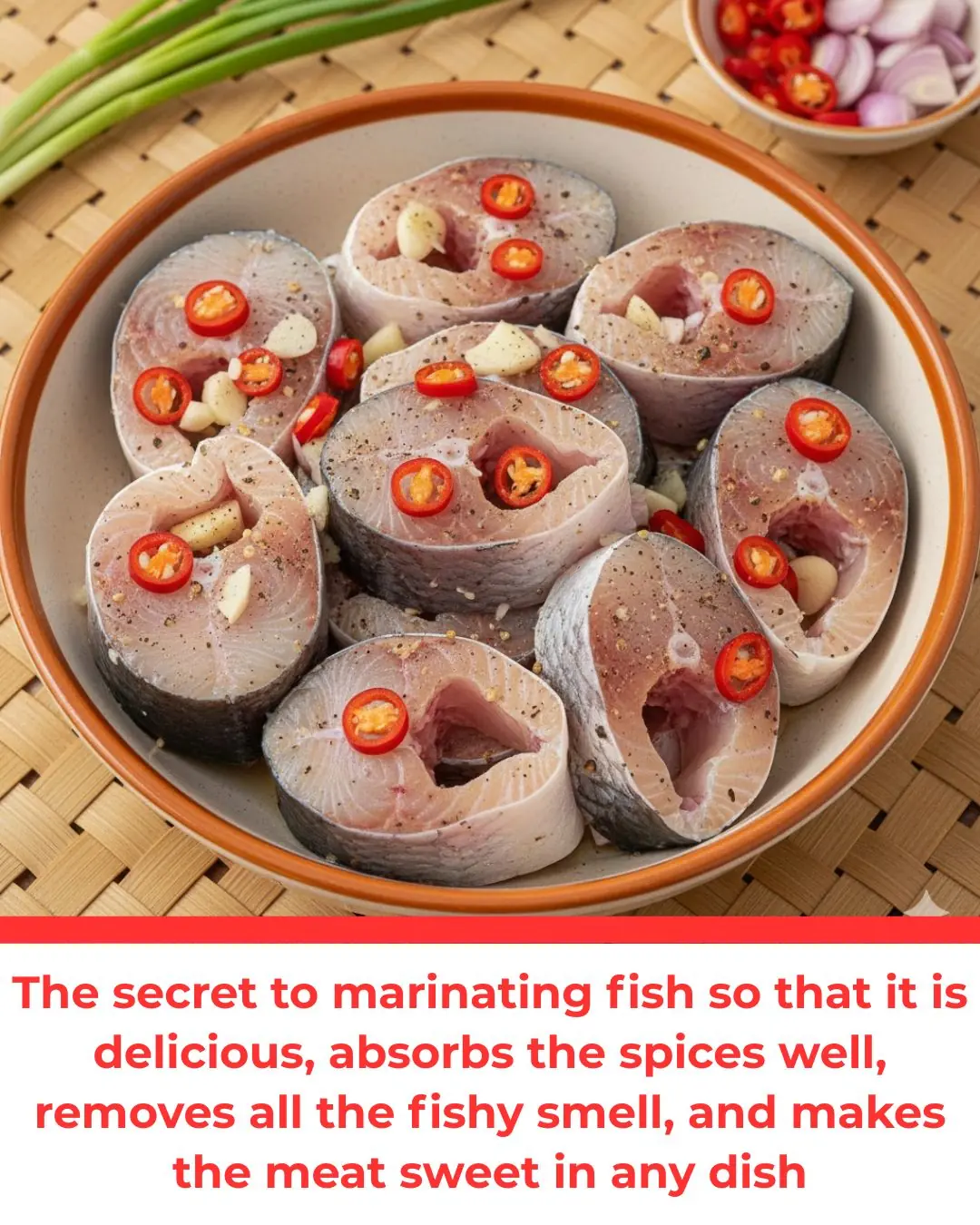
The secret to marinating fish so that it is delicious, absorbs the spices well, removes all the fishy smell, and makes the meat sweet in any dish
Boiled chicken is boring to eat forever: This good mother makes chicken with rich flavor and sweet meat, everyone loves it

Tips to remove grease from an air fryer using something available in every home
The HPV Vaccine Does Prevent Cervical Cancer, Scientists Confirm
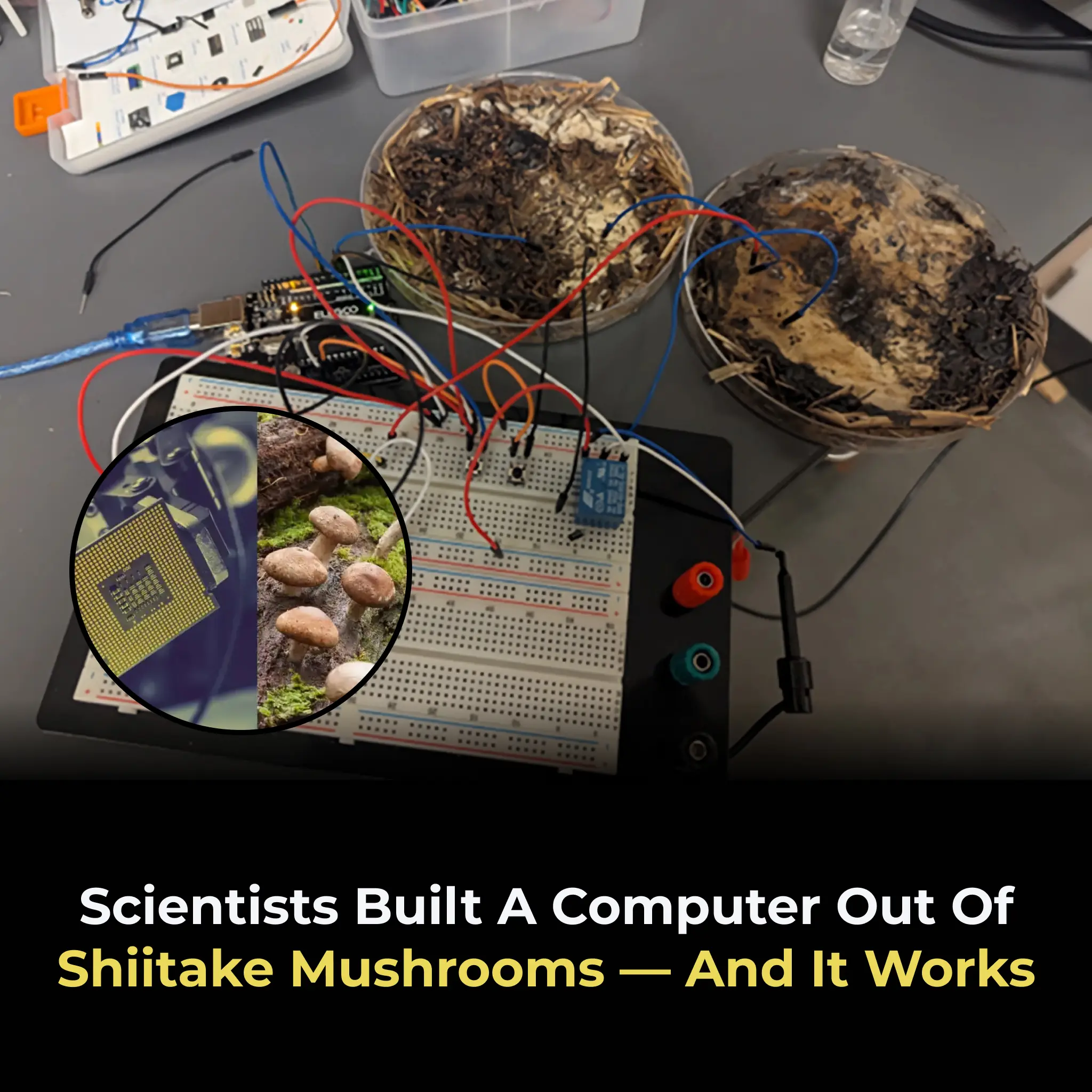
Scientists Built A Computer Out Of Shiitake Mushrooms — and It Works
12 Brilliant Ways to Reuse Silica Gel Packets at Home: Don’t Throw Them Away!

Female Dogs Can Accurately Detect Levels of Human Incompetence
