
Doctor's Warning To People Whose Fingers And Toes Change Color And Feel Numb In The Cold
Dr. O'Donovan, UK Physician and YouTuber, Explains the Real Meaning Behind Cold, Numb Extremities
A UK-based doctor and popular YouTuber, Dr. O'Donovan, has issued a health alert that may concern more people than you might think. If your hands and feet change color and go numb in cold weather—not just feeling a bit chilly—this could be a sign of a specific circulatory condition that deserves medical attention.
In a recent video posted on his YouTube channel, Dr. O'Donovan, a licensed and practicing physician, shared insights into a condition that doesn't just appear in cold temperatures, but can also be triggered by emotional stress or anxiety. While many of us are familiar with the uncomfortable feeling of cold fingers or toes, this is something different—and more serious.
What is Raynaud’s Disease?
According to Dr. O'Donovan, what you're experiencing might be Raynaud’s disease (or Raynaud’s phenomenon), a condition in which small blood vessels—usually in the fingers and toes—suddenly narrow, reducing blood flow. This reaction can be triggered by cold temperatures or stress and often causes the affected areas to change color: first turning white due to lack of blood flow, then blue as the area becomes oxygen-deprived. Once circulation returns, the skin may appear red and start to tingle, throb, or swell.
These episodes can last anywhere from a few minutes to several hours, depending on the individual and the severity of the case. In some people, symptoms are mild and manageable, while others may find them debilitating.
Interestingly, Raynaud’s doesn’t just affect the fingers and toes. In rarer cases, the nose, ears, lips, or even nipples may be involved. The severity and range of symptoms can vary widely from person to person.
Two Types of Raynaud’s: Primary vs. Secondary
Dr. O'Donovan emphasized that there are two distinct types of Raynaud’s:
-
Primary Raynaud’s: The more common form, not linked to any other underlying health problem. It’s usually less severe and often appears between the ages of 15 and 30.
-
Secondary Raynaud’s: Less common but more serious, this form is associated with other underlying medical conditions like autoimmune diseases (e.g., lupus or scleroderma), artery diseases, or high blood pressure. It can also result from repetitive hand movements or exposure to certain chemicals.
Secondary Raynaud’s typically shows up later in life, usually after the age of 40, and requires more intensive medical evaluation and care.
Who is Most at Risk?
Raynaud’s is more common in women than in men, and people living in colder climates are also at greater risk. Genetics may also play a role—if a family member has Raynaud’s, your chances of developing it may be higher.
Certain occupational risks can contribute to developing the condition, especially for people whose jobs involve repetitive hand use, like typing, or those who use vibrating tools such as jackhammers or power drills. Smoking is another significant risk factor, as it narrows blood vessels and worsens circulation.
Additionally, some medications, including beta-blockers and certain migraine drugs, may trigger or worsen Raynaud’s symptoms.
Preventing and Managing Raynaud’s Symptoms
To avoid triggering Raynaud’s attacks, Dr. O'Donovan advises dressing warmly in cold weather, especially protecting your extremities. Wearing thermal gloves, thick socks, scarves, and layered clothing helps maintain core and peripheral warmth. Portable hand warmers can also be a useful tool.
Lifestyle changes can also make a difference. Quitting smoking, managing stress through techniques like mindfulness or yoga, and avoiding known triggers can significantly reduce symptoms.
If lifestyle adjustments aren’t enough, Dr. O'Donovan suggests that medical treatments may be necessary. These can include calcium channel blockers to relax and open small blood vessels, or even surgical options in extreme cases.
He recommends seeing a healthcare professional if your symptoms are getting worse, becoming more frequent, or starting to interfere with your daily life. Early diagnosis and treatment can prevent complications and improve quality of life.
News in the same category


Vaping vs. Smoking: New Study Says Vapes May Be More Harmful

Study Explains How the First Born Child Is Often the Most Intelligent

What 20 Seconds of Hugging Can Do for You
New Study Found Microplastics In Every Single Human Semen Sample

Unlock the Health Benefits of the Castor Bean Plant: A Natural Remedy for Wellness
10 Vegetables That Are Good for Your Heart

I-motif DNA structures are formed in the nuclei of human cells
Hyperacute rejection-engineered oncolytic virus for interventional clinical trial in refractory cancer patients

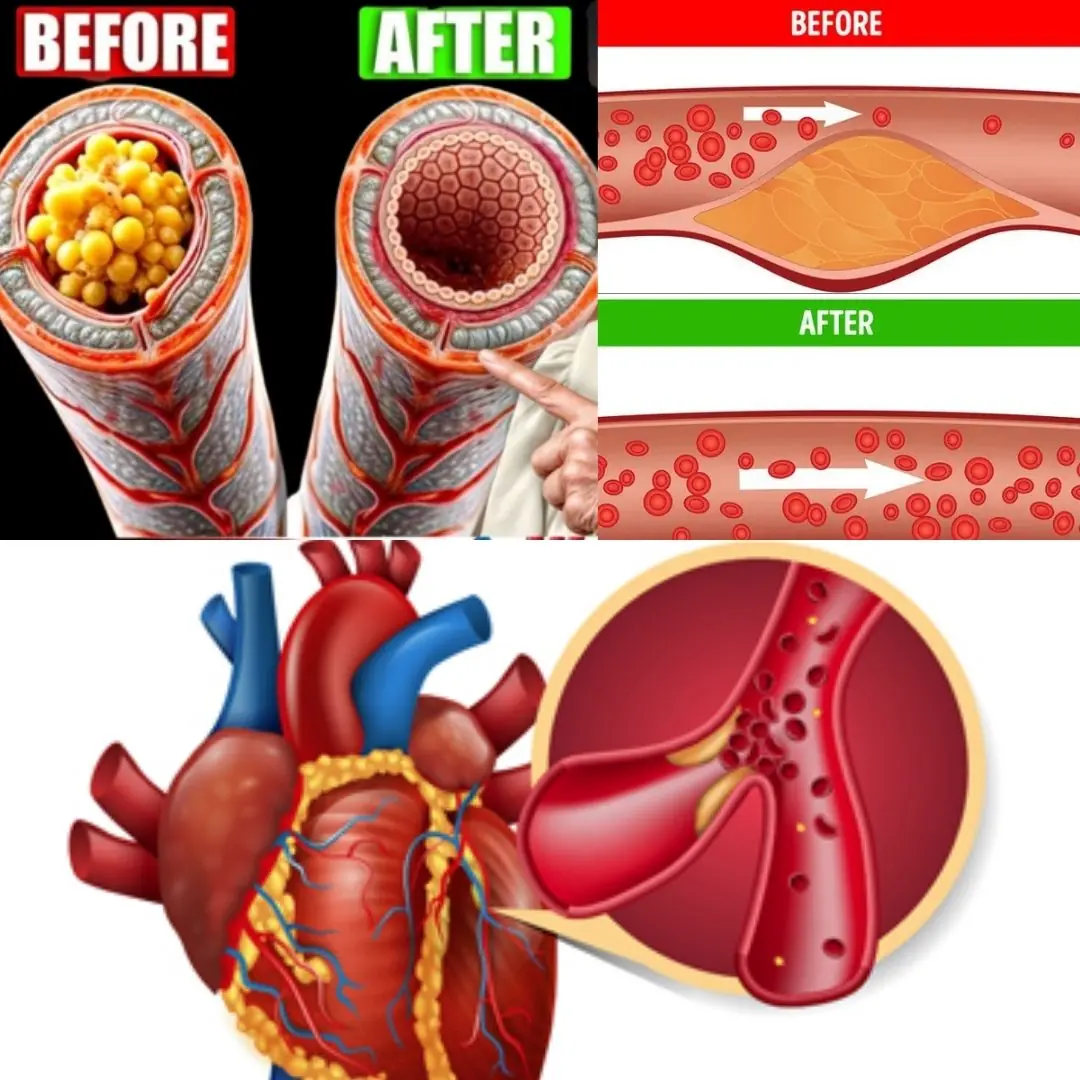
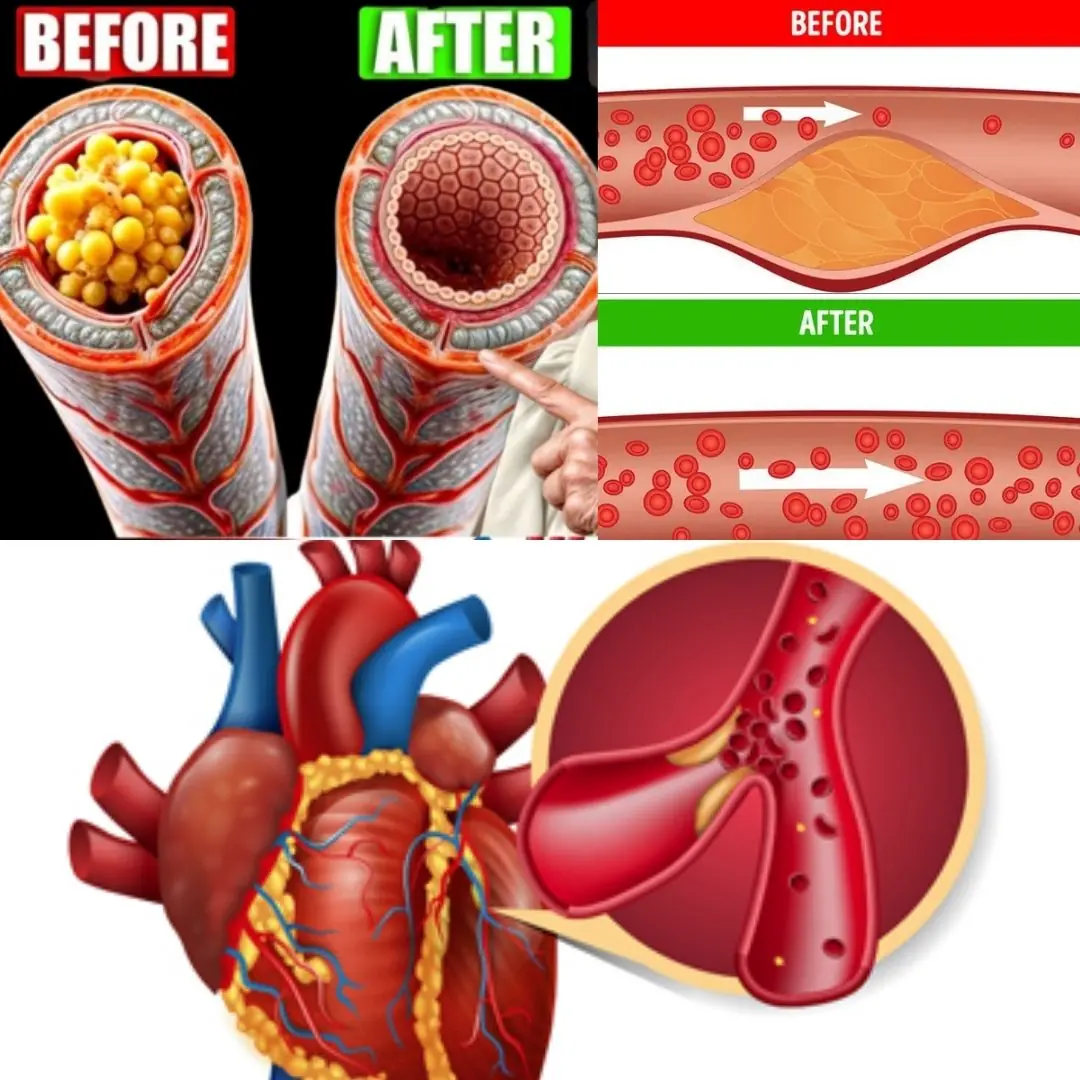
Your Feet Could Be Signaling That Your Arteries Are Clogged

36-Year-Old Teacher Dies From Diabetes Doctors Say Was Triggered By Everyday Foods
Cancer Rates Rising in Gen X and Millenials Compared to Older Generations, Study Finds
Lungs Full of Mucus? 1 SINGLE Drop Clears Airways & Restores Lung Health! | Barbara O’Neill
Rejuvenate Your Prostate Naturally: The Incredible Power of Tomato and Garlic Juice

Experts reveal the five foods that seriously affect your eyesight including one many of us eat every day
Early signs of diabetes many fail to notice
Bizarre permanent effect being stressed for just 5 days can have on your body

Everything to know about US measles outbreak as 2025 cases so far surpass numbers for whole of 2024
News Post
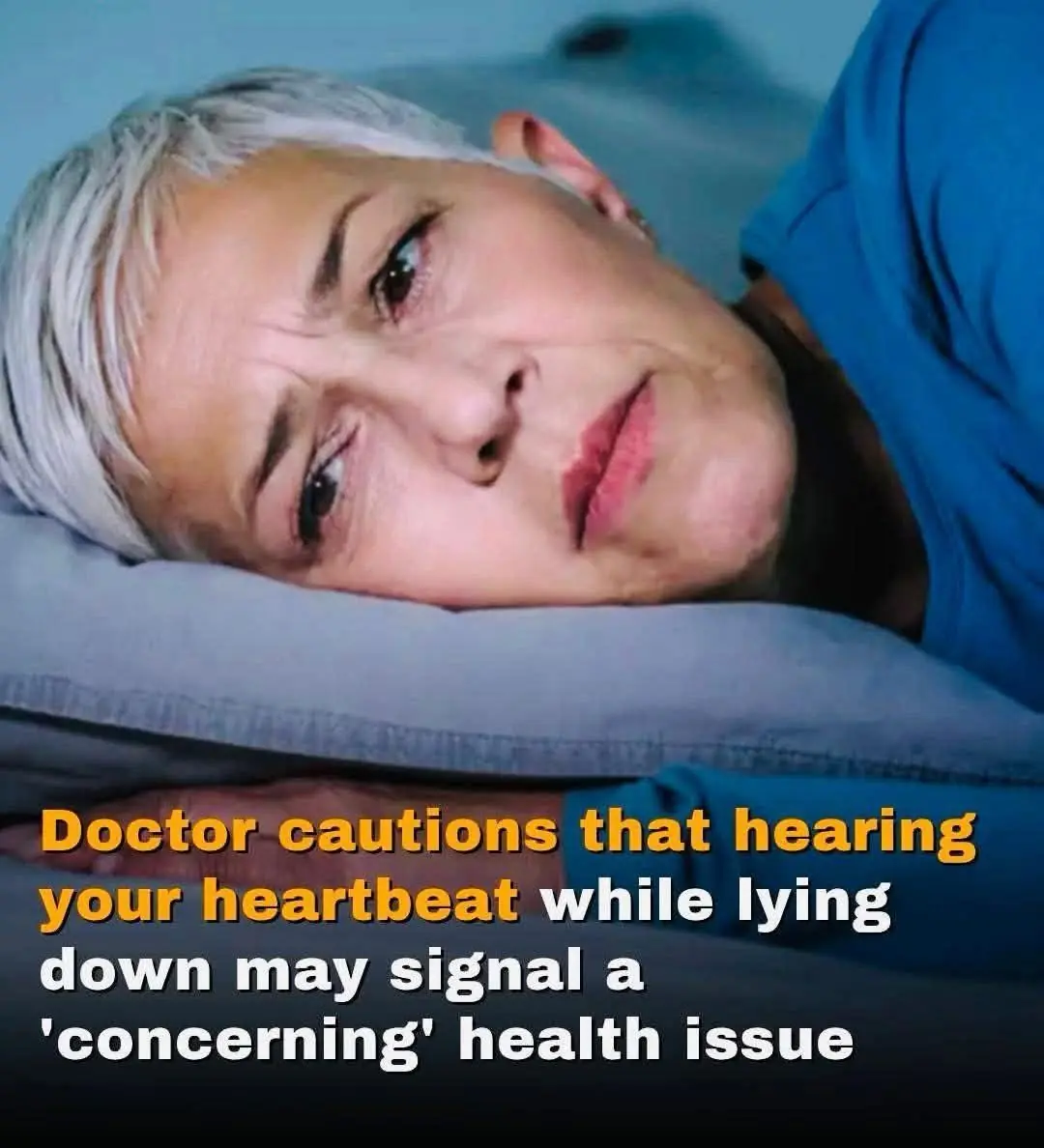
Pulsatile Tinnitus: Why You Hear Your Heartbeat While Lying Down

Red Spots on Skin: 13 Common Causes

Vaping vs. Smoking: New Study Says Vapes May Be More Harmful

Businessman Loses All Hope After His Diagnosis, but One Hospital Encounter Changes Everything

My Husband's 'Business Partner' Showed Up at Our Door and Mistook Me for the Cleaning Lady — I Decided to Play Along

My Husband Asked for a Divorce Right After Learning About His Rich Father's Inheritance

Entitled Mom Claimed My Seat at the Cafe — Her Face Turned Red after I Taught Her a Lesson

My Fiancé Told Me His Grandma Wanted to Meet Me Before the Wedding – As I Arrived, a Nurse Pulled Me Aside and Said, 'Don't Believe a Word'
The Healthy Benefits Behind Grapeseed Extract: A Comprehensive Guide

I Built My Dream Home With My Husband of 22 Years — Then He Put It in His Mistress's Name!

Study Explains How the First Born Child Is Often the Most Intelligent

What 20 Seconds of Hugging Can Do for You
New Study Found Microplastics In Every Single Human Semen Sample

Unlock the Health Benefits of the Castor Bean Plant: A Natural Remedy for Wellness

'I Told You a Hundred Times Not to Do That!' My Husband's Accidental Words to My Friend, Whom I Thought He Had Never Met Before

We Rented a House From an Elderly Woman—And Found Letters in the Walls from the Man She Lost
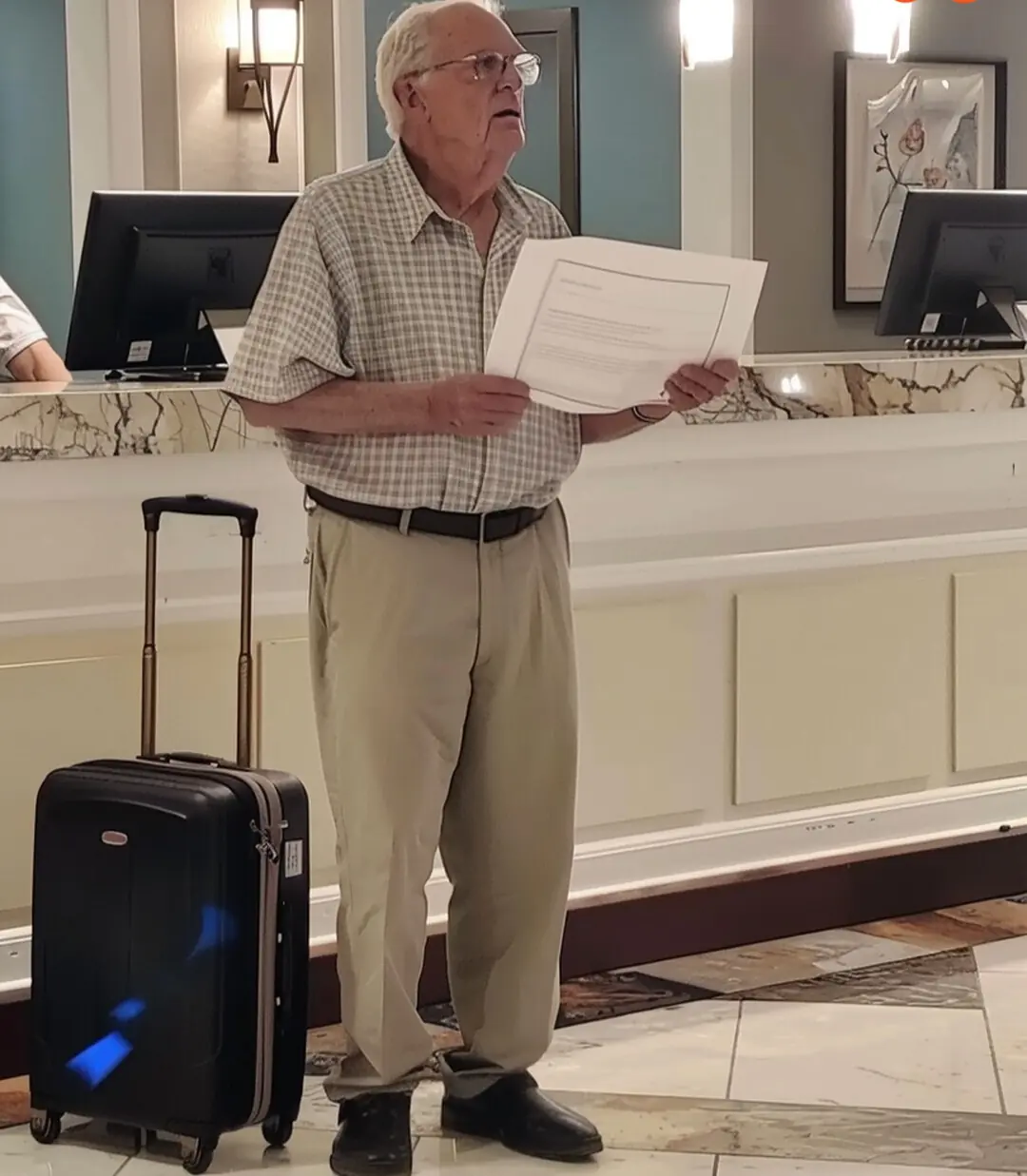
My Family Left Grandpa at the Hotel to Avoid Paying — They Didn't Realize I Was the Wrong Grandson to Mess With
10 Vegetables That Are Good for Your Heart
