New Research Shows Beta Blockers May Raise Heart Failure Risk in Women With Hypertension
Beta blockers are among the most commonly prescribed medications for controlling high blood pressure—a major risk factor for heart disease. But new evidence suggests that they may not affect men and women equally. According to a study published in Hypertension and led by researchers at the University of Bologna, women taking beta blockers for hypertension may face a nearly 5% higher risk of heart failure than men when they arrive at the hospital with acute coronary syndrome.
This finding raises important questions about whether current blood pressure treatments adequately account for biological differences between men and women—especially since women remain historically underrepresented in clinical trials.
Key Study Insights
Researchers evaluated 13,764 adults across 12 European countries. All participants had:
-
Hypertension
-
No prior cardiovascular disease
-
An acute coronary syndrome event
They were separated into two groups:
1️⃣ Those taking beta blockers
2️⃣ Those not taking beta blockers
The results revealed a striking gender difference in outcomes.
Beta Blockers Affected Women and Men Differently
Among participants using beta blockers:
-
Women had a 4.6% higher rate of heart failure compared to men at hospital presentation.
-
Both men and women who developed heart failure had 7x higher mortality compared to patients who had a heart attack without heart failure.
-
Women experiencing a ST-segment elevation myocardial infarction (STEMI)—a severe type of heart attack—were 6.1% more likely than men with STEMI to develop heart failure.
Among participants NOT taking beta blockers:
-
Men and women had nearly identical rates of heart failure.
This strongly suggests that beta blockers may contribute to worse outcomes in women under certain conditions.
Why the Difference?
Lead author Dr. Raffaele Bugiardini explained that prior beta-blocker research has heavily skewed toward male participants, which may have masked meaningful differences in how women respond to the medication.
The team proposed several possible explanations:
-
Biological differences in how women metabolize medications
-
Interaction between hormone replacement therapy and beta blockers
-
Variations in vascular response tied to female sex hormones
However, hormone therapy data was not included, so these remain hypotheses.
What Does This Mean for Women With Hypertension?
For women without prior cardiovascular disease who are taking beta blockers only to control blood pressure, the study’s authors emphasize the need for careful re-evaluation.
Dr. Bugiardini suggests:
-
Prioritizing diet and exercise as first-line approaches
-
Understanding that beta blockers may not offer equal safety across genders
-
Encouraging more research that includes balanced male–female participation
Because the study was observational, randomized trials would be needed to confirm causality—yet such trials may be ethically challenging since they would deliberately test for potential harm.
What Women Should Discuss With Their Doctor
If you are a woman taking beta blockers for high blood pressure, consider asking your healthcare provider:
-
Are there alternative medications better suited for women?
-
Could lifestyle changes reduce the need for medication?
-
Do I have additional risk factors for heart failure?
-
Should I be monitored more closely?
Conclusion
This emerging evidence highlights a critical gap in cardiovascular care: women are still underrepresented in key clinical research, and as a result, their risks may be underestimated. Beta blockers remain important and effective medications, but they may not be the best first-line treatment for all women with hypertension.
Understanding gender-specific responses can guide safer, more personalized treatment plans—and ultimately reduce the risk of heart failure in women.
Closing Lines (CKD Health Standard)
At CKD Health, we believe that heart care must be personalized—especially for women, whose bodies respond differently to medications and cardiovascular stress. By staying informed, advocating for equitable research, and working closely with your healthcare provider, you can make the safest decisions for your heart and long-term wellbeing.
News in the same category
13 Science-Backed Benefits of Drinking Lemon Water Daily

Spray This 3-Ingredient Oil On Your Feet 10 Minutes Before Bed And You’ll Be Dozing Off In No Time!
Sniffing Rosemary Can Increase Memory by 75%

The 60-second trick to reset your nervous system
Cleanse Your Kidneys of Toxins With 2 Effective 1-Ingredient Drinks

The unexpected connection between morning blood flow and a stronger heart

7 gentle balance moves seniors are using to feel steadier on their feet
How to Improve Your Vision with Garlic and Lemon – Effective Home Remedies

Top 3 vitamins to repair painful joints that actually work!
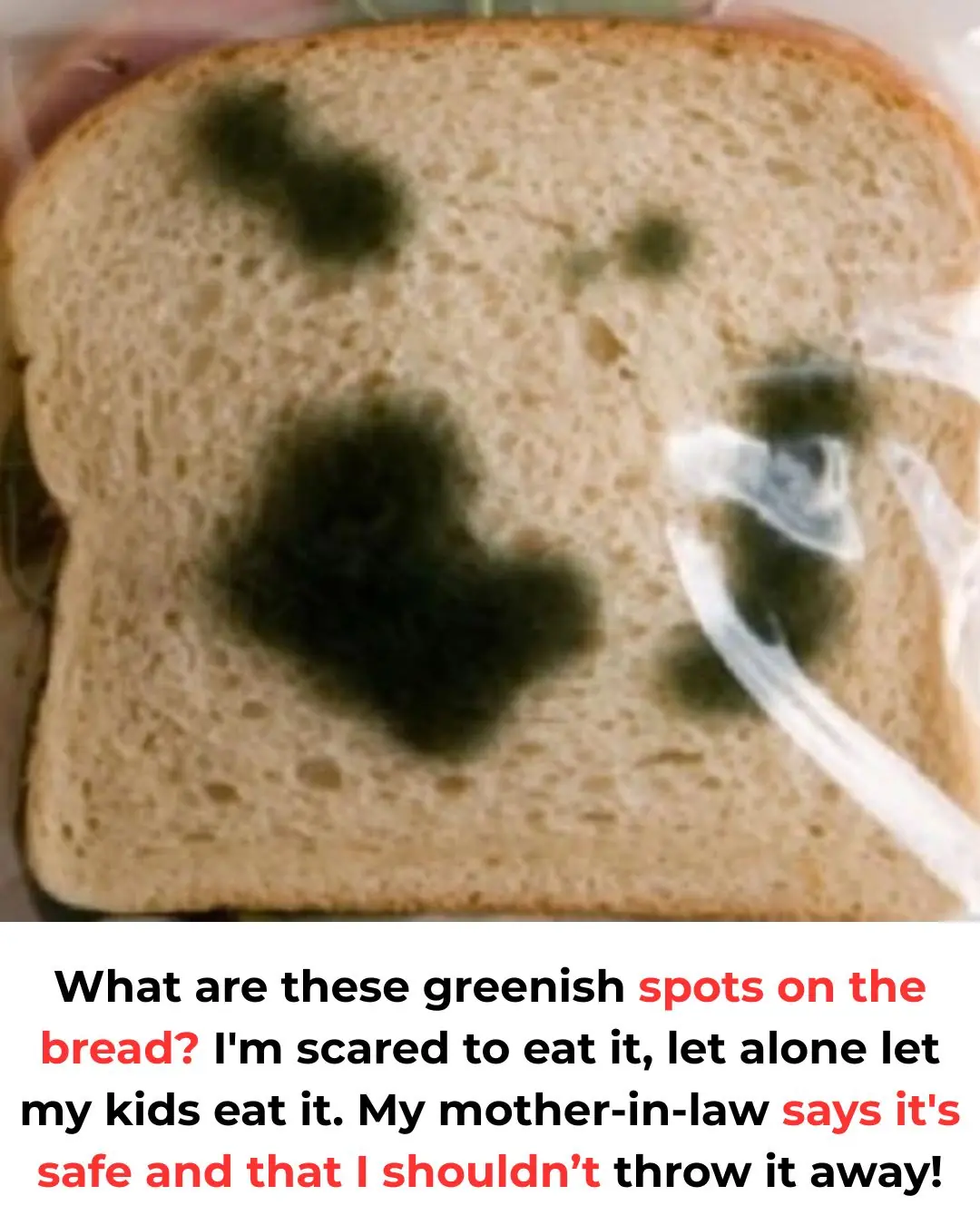
Should or should not eat and why
If you feel itching in these 3 areas, here’s what your body might be trying to tell you
1 cup that instantly wakes your kidneys up and strengthens them naturally
What Clearing the Table Says About You

The effortless joint pain relief trick you will wish you tried sooner

The trick to finally ending stomach pain that refuses to go away
6 Foods That Can Drain Your Calcium and Weaken Bones
If You Carry Bl.ood Type O, You Must Know This to Protect Your Life

How to lower blood pressure naturally (doctor explains)
News Post

The Hidden Power: How Green Papaya Sap Soothes Cracked Heels and Boosts Digestion
Anise Seeds: 8 Remarkable Benefits for Women – When Science Meets Ancient Tradition
Two Tablespoons in the Morning: The Power of Magnesium Chloride
Warning Signs of an Overworked Liver—and the Top Herbs to Help Restore Its Function
Drink Just 1 Glass Before Bed to Cleanse Your Entire Colon in 10 Minutes
The Power of Clove Steam Inhalation (Respiratory Relief You Can Feel Immediately)
13 Science-Backed Benefits of Drinking Lemon Water Daily
Doctors Reveal What Eating Cauliflower Really Does to Your Body — And Why You Shouldn’t Ignore It

Spray This 3-Ingredient Oil On Your Feet 10 Minutes Before Bed And You’ll Be Dozing Off In No Time!
Sniffing Rosemary Can Increase Memory by 75%

The 60-second trick to reset your nervous system
Cleanse Your Kidneys of Toxins With 2 Effective 1-Ingredient Drinks

The unexpected connection between morning blood flow and a stronger heart
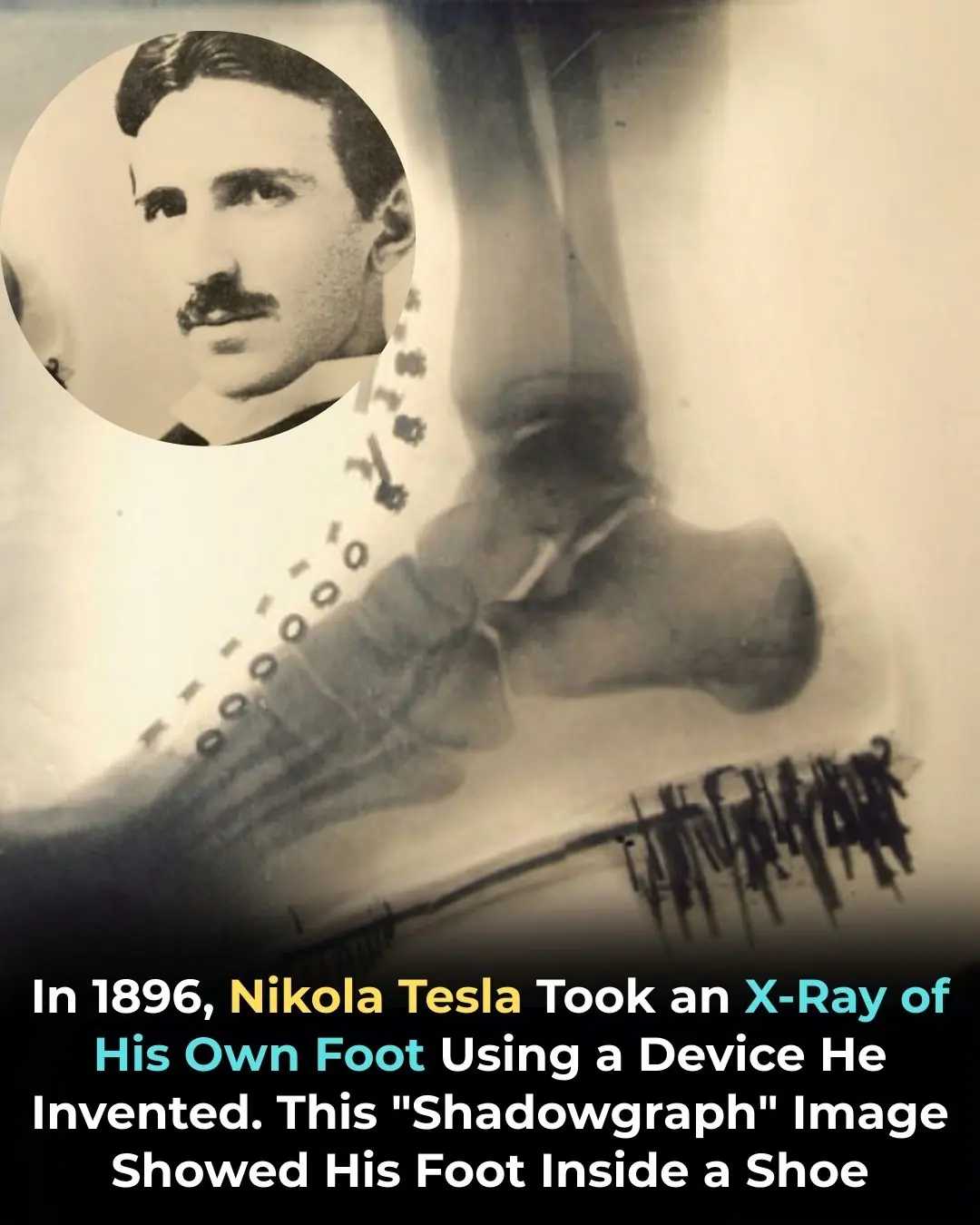
Nikola Tesla X-Rayed His Own Foot in 1896 — Pioneering the Future of Medical Imaging
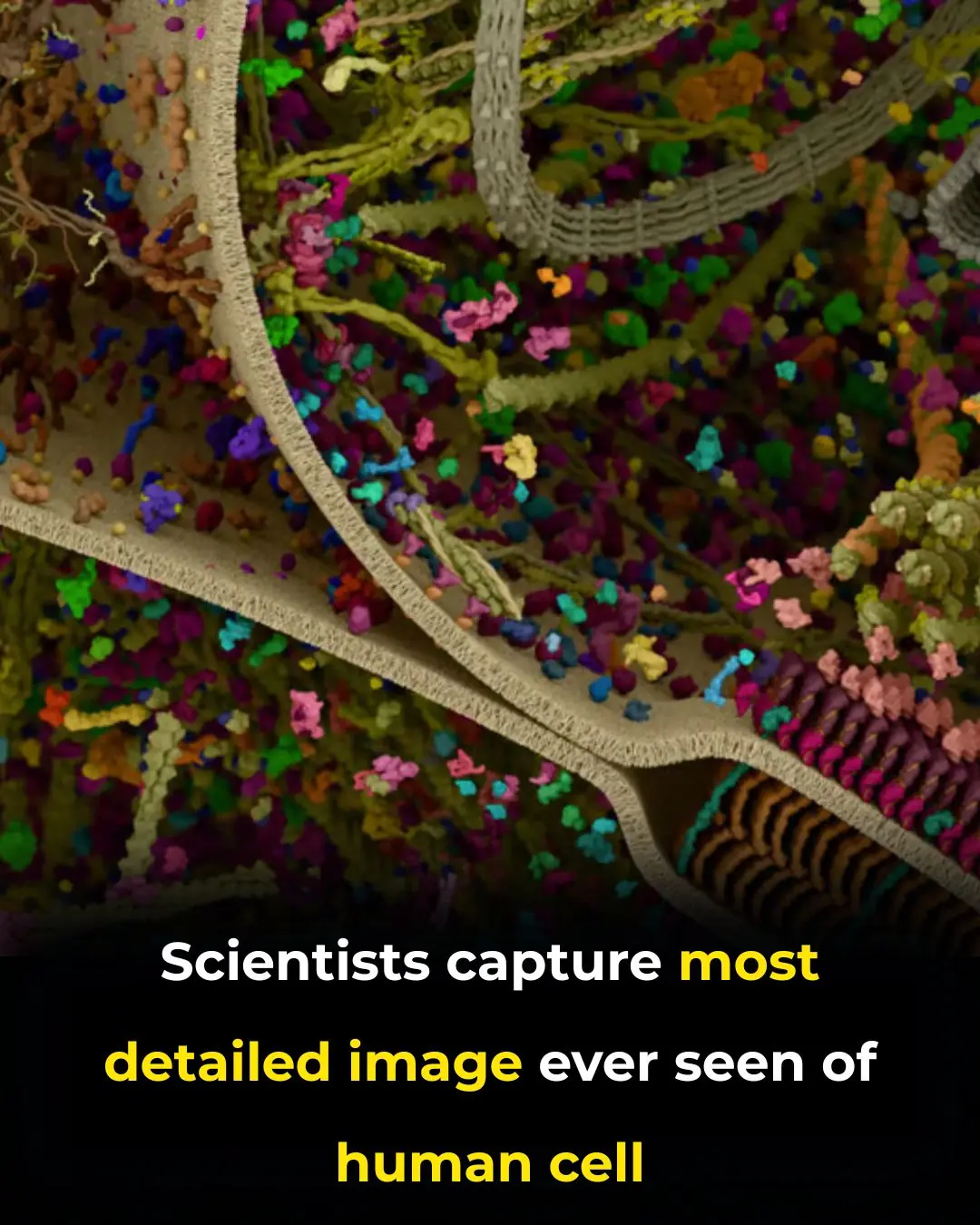
Revolutionary Breakthrough: Scientists Capture the Most Detailed 3D Image of a Human Cell

7 gentle balance moves seniors are using to feel steadier on their feet
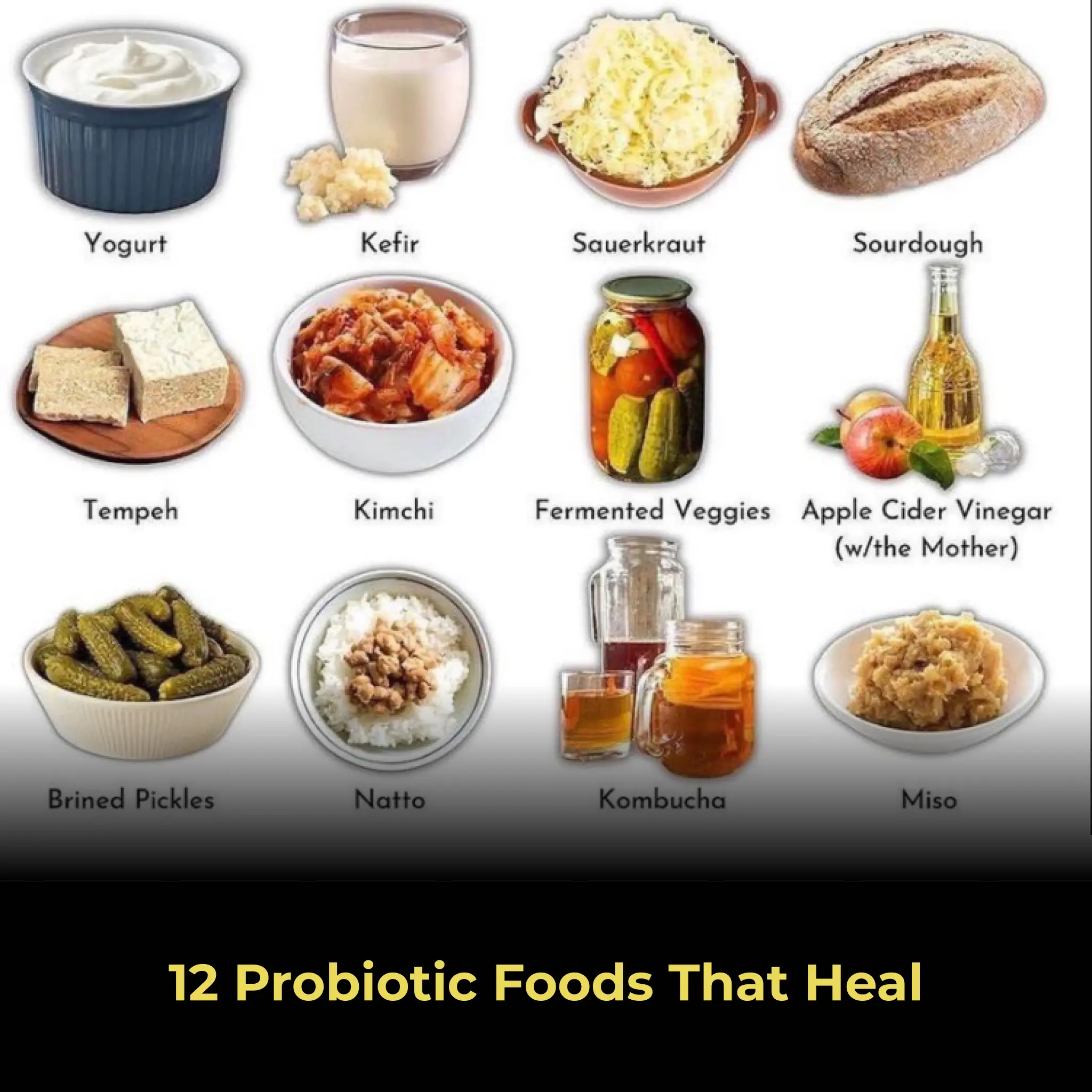
12 Probiotic Foods That Heal

Connecting Consumers to Farmers: The Trend of Personalized Food Packaging in Japan