
Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors
Emerging research suggests that Alzheimer’s disease may be linked to an unexpected culprit — gum disease.
A study discovered the presence of Porphyromonas gingivalis, a bacteria responsible for chronic periodontitis, in the brains of deceased Alzheimer’s patients.
Researchers found that when mice were infected with the bacteria, it colonized their brains and triggered the production of amyloid beta, a protein commonly associated with Alzheimer’s. This evidence strengthens the hypothesis that the disease could have infectious origins rather than being solely a neurodegenerative disorder.
The study also revealed that toxic enzymes from the bacteria were present in individuals who had Alzheimer's-related brain changes but had not yet been diagnosed with dementia, suggesting the infection may begin years before symptoms appear.
This discovery opens the door to new potential treatments. A pharmaceutical company, Cortexyme, developed a compound called COR388, which showed promise in reducing both bacterial infection and amyloid beta accumulation in animal trials. While human trials are needed to confirm its effectiveness, the study underscores the importance of oral hygiene in brain health. Scientists remain cautiously optimistic, emphasizing that with no new dementia treatments in over 15 years, investigating all possible causes is crucial. While more research is needed, the link between gum disease and Alzheimer’s highlights a simple yet vital message: taking care of your teeth might help protect your brain in the long run.
Porphyromonas gingivalis, the keystone pathogen in chronic periodontitis, was identified in the brain of Alzheimer’s disease patients. Toxic proteases from the bacterium called gingipains were also identified in the brain of Alzheimer’s patients, and levels correlated with tau and ubiquitin pathology. Oral P. gingivalis infection in mice resulted in brain colonization and increased production of Aβ1–42, a component of amyloid plaques. Further, gingipains were neurotoxic in vivo and in vitro, exerting detrimental effects on tau, a protein needed for normal neuronal function. To block this neurotoxicity, we designed and synthesized small-molecule inhibitors targeting gingipains. Gingipain inhibition reduced the bacterial load of an established P. gingivalis brain infection, blocked Aβ1–42 production, reduced neuroinflammation, and rescued neurons in the hippocampus. These data suggest that gingipain inhibitors could be valuable for treating P. gingivalis brain colonization and neurodegeneration in Alzheimer’s disease.
News in the same category

Human Stomach Can Dissolve Stainless steel.
Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors
New blood test identifies hard-to-detect pancreatic cancer with 85% accuracy
5 Overlooked Signs You Might Have ADHD Without Realizing It

Higher consumption of sugary beverages linked with increased risk of mortality
Highly Intelligent People Are Less Satisfied By Having Friends, And There’s A Fascinating Reason Why

6 Effective and Safe Ways to Naturally Whiten Your Teeth
Clean Arteries: 10 Foods to Eat Daily
Struggling With Mucus? 5 Foods To Help and 4 That Make It Worse

Don’t Ever Use Turmeric If You’re On Any of the Following Medications
Is Drinking Water First Thing in the Morning Beneficial?
New Study Reveals Concerning Cause Behind Certain Kidney Damage

Check for 6 diseases

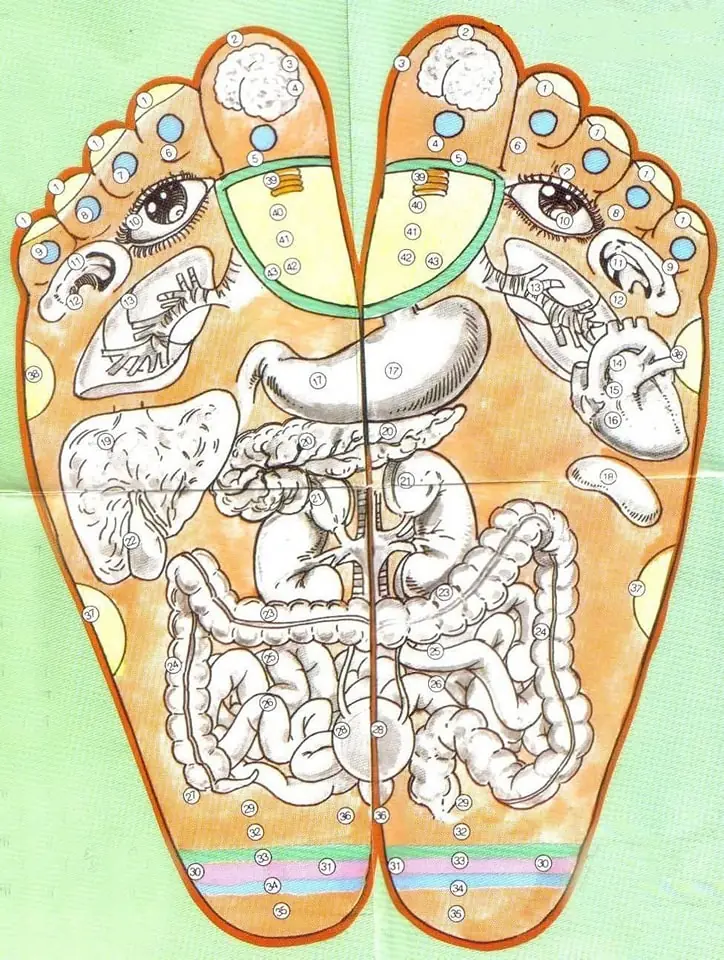
Are Feet an "Early Warning Sign" of Cervical Cancer? Don’t Ignore These 4 Situations

Cancer Dies When You Start Eating These 7 Foods. Time to Start Eating Them
YOUR BODY IS ASKING FOR HELP! 10 Warning Signs of Nutrient Deficiencies & How to Fix Them

Eliminate Cancer, Diabetes, and High Blood Pressure with Dr. Frank Suárez’s Home Remedy

Healthy Green Juices for Liver Health | Detoxify Your Body | Burn Fat and Improve Your Health
News Post

My Sister Gave Up Her Adopted Daughter After Having a Bio Son — but Karma Hit Back Immediately
Love isn't supposed to have conditions. But for my sister, it did. Without an ounce of guilt, she gave up her adopted daughter after having a biological son. As I tried to comprehend the cruelty, she simply shrugged and said, "She wasn't really mine anywa

Is It Normal to Hear Your Heartbeat While Lying On Your Pillow? What You Need to Know

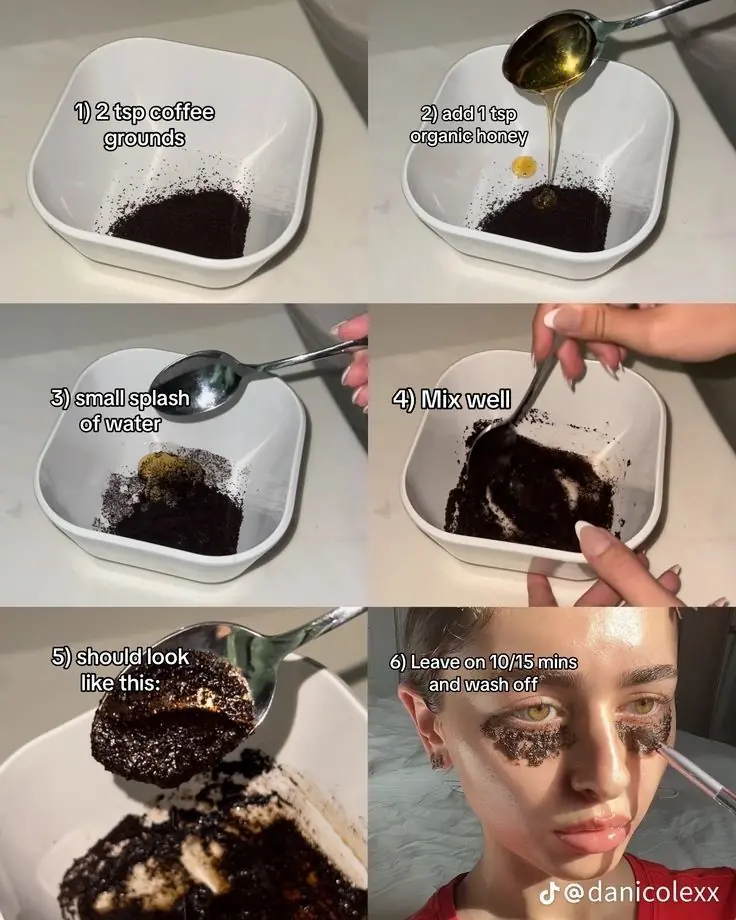
Dark Neck Home Remedies To Get Rid Of It

Vaseline and Lemon for Clear, Glowing Skin: A Simple Guide

Get Rid Of Large Pores In 4 Steps, Naturally!
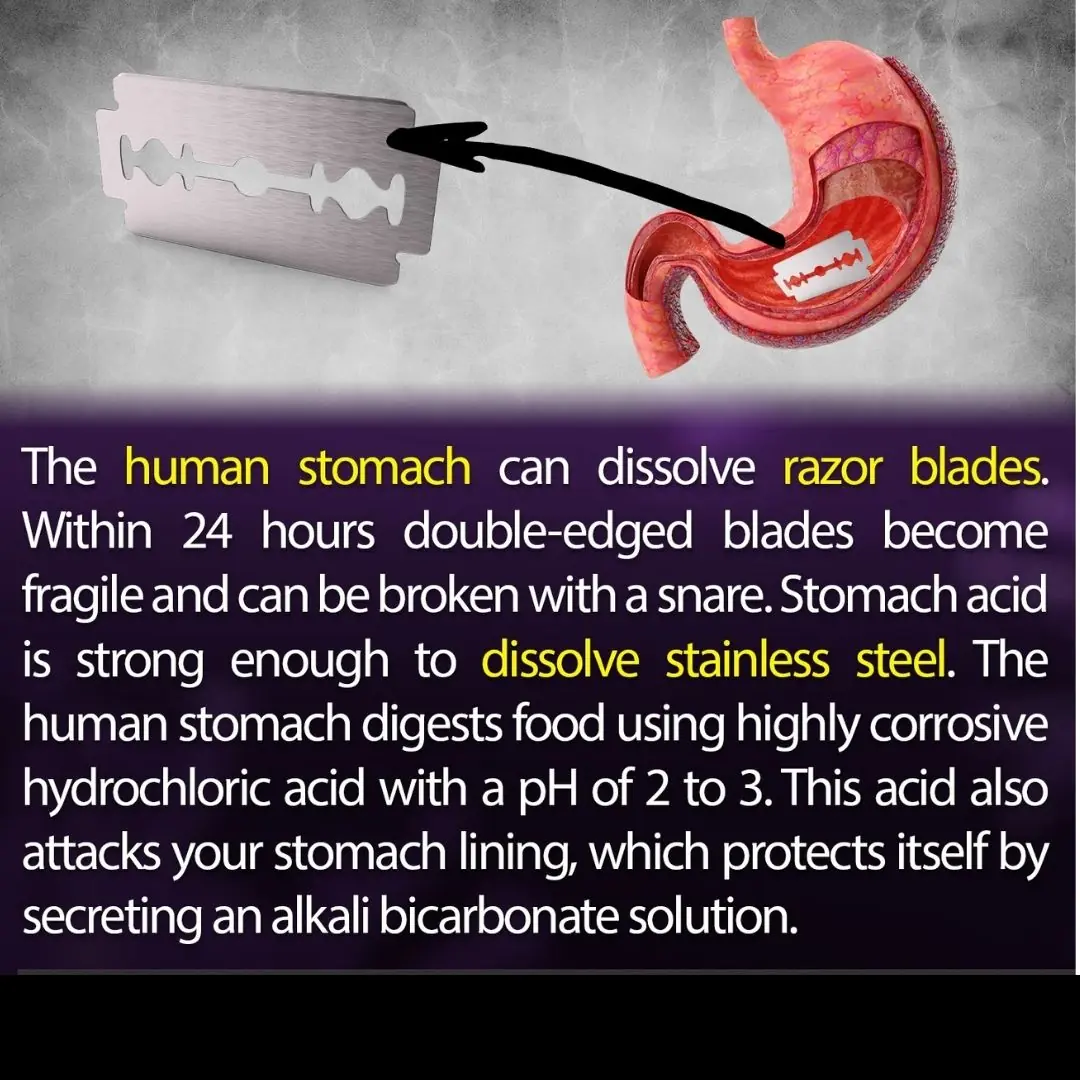
Human Stomach Can Dissolve Stainless steel.

Ever Heard Of Mix Cloves and Vaseline as A Moisture Boost For Hands?

DIY Miracle Shampoo to Stop Hair Loss & Regrow Hair – Even on Bald Spots!

Use this diy cream to look years younger

This Common Antidepressant Is Secretly Battling Infections & Sepsis—And Doctors Are Shocked
New blood test identifies hard-to-detect pancreatic cancer with 85% accuracy

3 Most Effective Essential Oils To Get Rid Of Dark Spots On Your Face

Mix Parsley with Apple! 🔥 A Secret No One Will Tell You – 100% Effective!

Explore Numerous Natural Skincare Recipe From Cucumber
5 Overlooked Signs You Might Have ADHD Without Realizing It

🌿✨ Facelift with Natural Collagen! At 65, Wrinkles Disappear in 3 Minutes with Rice Water! 💖

I Thought My Neighbor Was a Good Mom Until I Learned She Was Keeping Her Stepdaughter Only Because of Her Father's Will, So I Decided to Act — Story of the Day
When my neighbor died, I tried to help his grieving family. His daughter was left with her stepmother, who seemed kind at first. But as I spent more time with the little girl, I started to see things that didn’t feel right. I knew I couldn’t just stan
Erase Wrinkles in 3 Minutes? The Magic of Yeast and Coffee for Youthful Skin

My Ex-husband Ripped off the Wallpaper After Our Divorce Because 'He Paid for It' – Karma Had a Joke in Store for Him
My ex-husband once told me, "It's just harmless fun." That's what he called his infidelity. But when he ripped the wallpaper off my walls after our divorce, karma decided it was her turn to have some fun — with him.