Scientists reverse tissue calcification with just one supplement (not vitamin K2!)
What if a simple, everyday mineral could help dissolve harmful calcium deposits in your arteries, joints, and organs?
It sounds almost unbelievable—but emerging research suggests that magnesium may play a powerful role in preventing and even reversing one of the most dangerous processes of aging: soft tissue calcification.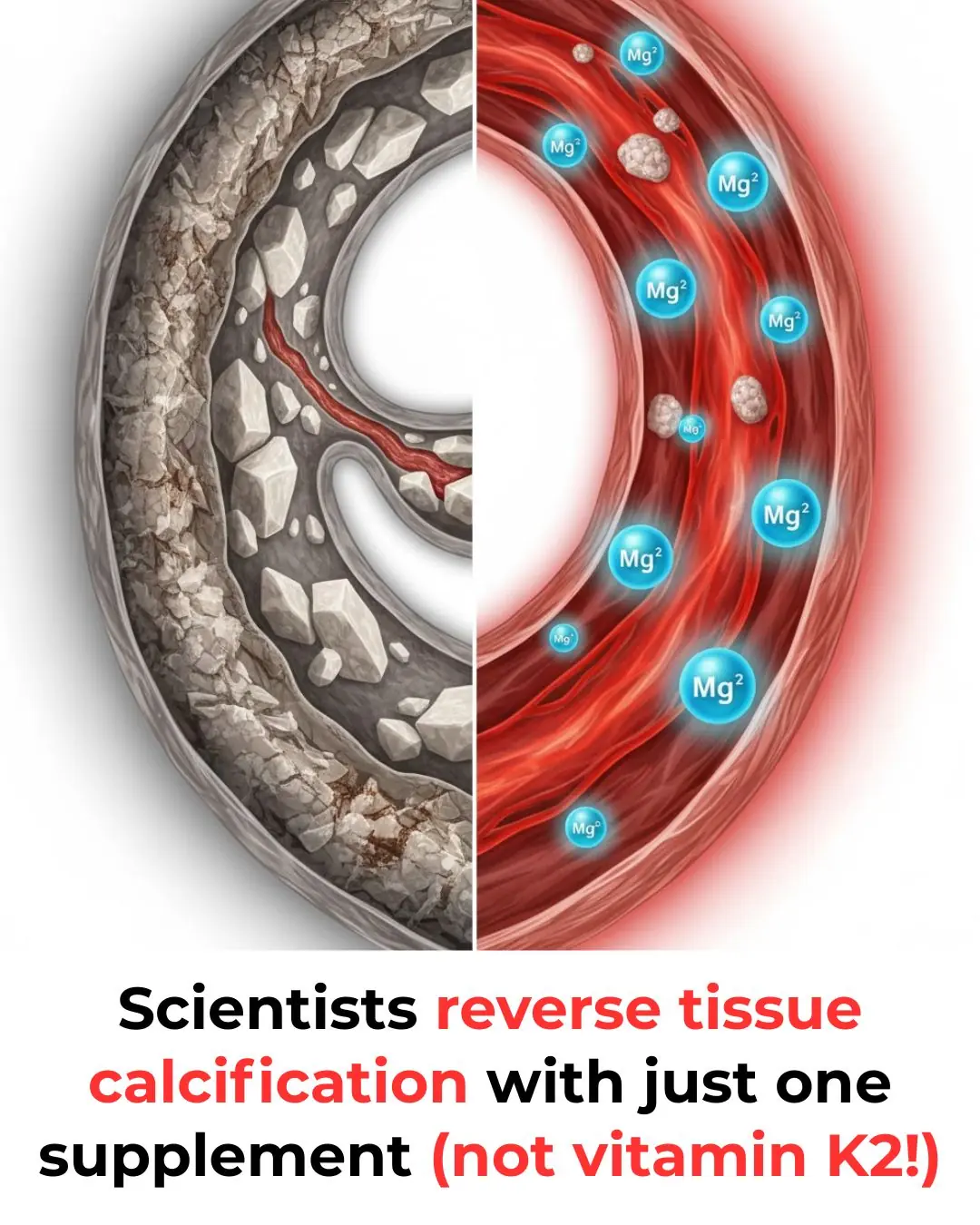
We’re often told that once calcium is deposited in the wrong place—like artery walls or shoulder tendons—it’s there for good. But a growing body of evidence suggests that’s not entirely true.
By understanding how your body manages calcium, and how magnesium fits into that system, you may be able to:
-
Prevent harmful calcium buildup
-
Support the breakdown of existing deposits
-
Keep calcium where it belongs—in your bones, not your soft tissues
(Based on the insights of Felix Harder.)
Key Takeaways
-
Magnesium is a powerful “decalcifier”: It can help block calcium crystal formation in soft tissue and may assist in dissolving existing deposits.
-
It protects your arteries: Magnesium helps prevent blood vessel cells from turning into bone-like cells—a key step in artery calcification.
-
Low magnesium is a major risk factor: People with higher magnesium intake tend to have less arterial calcification and lower rates of heart disease.
-
It’s a system, not a single supplement: Magnesium works best as part of a complete calcium metabolism network—including vitamins K2, D, A, boron, and balanced electrolytes.
-
You’re not powerless: By optimizing your diet, supplements, and lifestyle, you can help direct calcium into your bones and away from your arteries.
1. The Study That Changed Everything
An older but fascinating study looked at 80 patients with painful calcium deposits in areas like the shoulders, elbows, and hips.
Doctors used a two-part strategy:
-
Injected magnesium sulfate (Epsom salt) directly into the calcified areas
-
Gave the patients oral magnesium lactate for several months
The results were striking:
-
Around 75% of patients experienced major improvement
-
Many saw their calcium deposits shrink significantly or disappear
-
Joint mobility improved
-
No major side effects were reported
⚠️ Important: This is not something to try at home. Injecting any substance without medical supervision is extremely dangerous.
What matters here is the principle:
Magnesium showed a remarkable ability to counteract tissue calcification.
The oral form used—magnesium lactate—is known to bind calcium, which may explain its effectiveness. While the study didn’t specify dosage, it strongly suggests magnesium has therapeutic potential for a condition long thought to be irreversible.
2. Magnesium’s First Superpower: Blocking Crystal Formation
Soft tissue calcification doesn’t happen as a flat, smooth layer. It forms as sharp, rigid crystals called hydroxyapatite—the same mineral found in your bones and teeth.
This process accelerates when:
-
Blood phosphate levels are high (often from processed foods or poor kidney function)
-
Calcium and phosphate meet in the wrong environment
They begin to clump together, forming tiny crystals that:
-
Stiffen arteries
-
Damage tissues
-
Trigger inflammation
Here’s where magnesium steps in like a chemical bodyguard:
-
Magnesium binds to phosphate, slowing down calcium-phosphate crystal growth
-
It disrupts crystal formation, preventing them from hardening
-
It can help convert hard crystals into amorphous (softer, more soluble) calcium phosphate, which your body can clear more easily
In simple terms:
Magnesium makes it harder for calcium and phosphate to “team up” and cause damage in your soft tissues.
3. Magnesium’s Second Superpower: Reprogramming ‘Bone-Like’ Arteries
The second mechanism is even more intriguing.
Your arteries are meant to be flexible tubes lined with smooth muscle cells. But under chronic stress—like:
-
Inflammation
-
Oxidative damage
-
High calcium and phosphate levels
These smooth muscle cells can undergo a disturbing transformation:
They begin to behave like bone-forming cells (osteoblasts).
When that switch is flipped, they:
-
Produce bone proteins such as osteocalcin
-
Start laying down mineral deposits
-
Turn soft, elastic arteries into stiff, “bone-like” tubes
This is the core of vascular calcification.
Magnesium appears to act at the cellular level by:
-
Sending signals that discourage artery cells from acting like bone cells
-
Helping them maintain or return to their normal, smooth-muscle identity
So magnesium is not just passively changing chemistry—it’s actively influencing how your artery cells behave.
4. Real-World Evidence: More Magnesium, Healthier Hearts
This isn’t just theory—we have strong real-world data.
Large population studies consistently show:
-
People with low magnesium levels are more likely to have:
-
Calcified arteries
-
Heart disease
-
Higher cardiovascular mortality
-
-
Those with higher magnesium intake have:
-
Less vascular calcification
-
Fewer heart attacks and strokes
-
Better long-term heart health
-
In dialysis patients, who are at extremely high risk for rapid arterial calcification:
-
Higher blood magnesium levels are linked to fewer cardiovascular events and lower death rates
-
Researchers are now exploring magnesium supplementation as a standard therapy to protect their arteries
The pattern is clear:
Adequate magnesium is one of the most important nutritional factors for avoiding calcified arteries and heart disease.
5. Why Magnesium Alone Isn’t a Magic Bullet
At this point, it’s tempting to think:
“Great, I’ll just take magnesium and fix everything.”
But severe calcification usually doesn’t come from a single missing nutrient. It’s a sign of a system-wide failure in calcium metabolism.
Your body’s ability to handle calcium depends on many pieces working together:
-
Absorption
-
Transport
-
Utilization
-
Excretion
If you have:
-
Low stomach acid
-
Vitamin D deficiency
-
Low vitamin K2
-
Poor diet or kidney issues
…then calcium can become “bio-unavailable”:
It’s floating around causing damage, but it can’t get into your bones where it belongs.
This is why people can have:
-
Osteoporosis (weak bones)
-
And calcified arteries at the same time
It’s not too little calcium—it’s calcium in all the wrong places.
6. How Calcium Metabolism Really Works: The Key Players
Let’s follow a bit of calcium from a food like cheese through your body:
1. Digestion
To free calcium from food, you need:
-
Strong stomach acid
-
Adequate zinc
-
B vitamins (especially B6)
-
Sufficient protein
Without these, absorption drops.
2. Absorption
Your gut uses vitamin D to activate receptors that allow calcium to cross into the bloodstream.
Low vitamin D = low absorption.
3. Transport & Targeting
Once in your blood, calcium must be managed:
-
It’s carried by proteins like albumin
-
It must be balanced with other minerals like magnesium, sodium, and potassium
-
Vitamin K2 activates proteins (like matrix Gla protein and osteocalcin) that:
-
Push calcium into bones and teeth
-
Keep it out of arteries and soft tissues
-
If vitamin K2 is low, that calcium can end up in your vessel walls instead of your skeleton.
7. Your Action Plan: Rebuilding the Calcium System
Reversing (or at least slowing) calcification isn’t about “piling on magnesium.”
It’s about rebuilding the whole calcium-handling system.
Here are the key players to focus on:
🧂 The Four Core Electrolytes
-
Calcium
-
Magnesium
-
Sodium
-
Potassium
They must be in balance. Together, they regulate:
-
Nerve function
-
Muscle contraction
-
Heart rhythm
🧬 Vitamin K2 (Non-Negotiable)
K2 is your calcium traffic controller:
-
Activates proteins that lock calcium into bones and teeth
-
Helps stop calcium from lodging in arteries and organs
You’ll find it in:
-
Natto (fermented soy)
-
Aged cheeses
-
Pasture-raised egg yolks
-
Grass-fed dairy
☀️ Vitamin D
Crucial for:
-
Calcium absorption
-
Immune function
Get it from:
-
Sunlight
-
Fatty fish
-
Egg yolks
-
Quality supplements (as needed)
🧡 Vitamin A & Boron
Support:
-
Bone remodeling
-
Mineral metabolism
-
Hormone balance
🏃 Mechanical Stress (Exercise)
No supplement can replace the signal sent by movement.
Weight-bearing activities like:
-
Walking
-
Strength training
-
Light jumping
tell your body:
“These bones are important—put calcium here.”
Conclusion: Think System, Not Shortcut
Soft tissue calcification is not just random bad luck—it’s a warning sign that your calcium regulation system is breaking down.
The empowering part?
You can work on that system.
-
Magnesium is a powerful tool—
-
It blocks crystal formation
-
Supports healthier arteries
-
May even help dissolve existing deposits
-
But it works best as part of a bigger picture that includes:
-
Vitamin K2
-
Vitamin D
-
Vitamin A
-
Boron
-
Balanced electrolytes
-
Regular movement
By gradually addressing each piece, you’re not just fighting plaque—you’re rebuilding the foundation of your cardiovascular and bone health.
Take your time.
Strengthen the system.
Let magnesium and its teammates do what they’re designed to do:
News in the same category

Signs of kidney failure that if ignored may require lifelong dialysis!

The effortless daily trick people use to double their potassium

Aspirin saves lives— but here’s what most people still get wrong about it

The top 10 foods people use to keep their blood sugar steadier

7 powerful anti-cancer foods you should start including in your diet

If Your Kidneys Are in Danger, the Body Will Show these 10 Signs

Top 8 Foods for Stronger Legs (Seniors, Eat Daily!)

He thought it was just an allergy, until the diagnosis proved otherwise
One Miracle Oil to Remove Dark Spots “Overnight”!

The #1 seed flour people over 60 use for steady energy and strength

Stop adding butter — eat these 3 foods instead for faster weight loss

Doctors warn: before a heart attack your body will warn you of these 7 RED flags

Foods to Eat if You Need to Poop – The Best Natural Laxatives to Relieve Constipation
This is what happens to your body when you stop having intimate relationships

Remember The ‘3 Don’ts’ After Meals And ‘4 Don’ts’ Before Bed To Prevent Strokes At Any Age

The Power of Citrus Pith: The Hidden Layer Packed With Health Benefits

Powerful Health Benefits of Pineapple You Should Know

7 Powerful Bay Leaf Benefits for Heart Health and Smoother Blood Flow
News Post
The Best Ways to Lower Blood Sugar Fast: What Science Really Says

New HIV Antibody Discovery Offers Hope for Universal Treatment and Prevention

Signs of kidney failure that if ignored may require lifelong dialysis!
Eyes as a Window to Heart Health: New Study Reveals How Eye Exams Can Detect Early Cardiovascular Risks
Revolutionary ALS Discovery: Immune System’s Role in Disease Progression Opens New Treatment Possibilities
The Heart as a 'Little Brain': Exploring Its Impact on Emotions, Decision-Making, and Mental Health
Groundbreaking Study Maps Brain Regions Linked to Dyslexia, Uncovering Connections to ADHD and Pain

Harnessing Anger and Passion for Purposeful Action
How Two Children Created the Perfect Birthday With Creativity Instead of Cash

How to Make Your Stainless Steel Pots Shine Like New and Choose Sweet, Juicy Oranges

Just tried this and whoa

Beer on the Window Sill: A Simple Trick With Surprising “Magic” Benefits
How to Make Rose Water at Home Using Fresh Rose Petals

You are doing it all wrong. Here's the right time to eat tomatoes

Mexico City Ends 500 Years of Bullfighting in Landmark Animal-Welfare Vote

Try This Method: Clean Your Floors Just Once a Week—They Stay Shiny, Fresh, and Dust-Free

10 Foods That Help Beat Fatty Liver: Nutrition Experts Recommend Eating Them Daily

The effortless daily trick people use to double their potassium
