
The 32-year-old teacher who almost lost her life to diabetes
A 32-year-old teacher, widely considered to be at a normal weight and following what many would describe as clean and healthy eating habits, was recently diagnosed with type 2 diabetes. Her diagnosis came as a shock — not just to her, but to many around her — and unfortunately, she is far from alone.
Contrary to popular belief, type 2 diabetes is not limited to individuals who are overweight, obese, or who consume large amounts of sugar. New research is shedding light on how a complex mix of modern dietary patterns, genetics, fat distribution, and metabolic function can lead to diabetes, even in people who appear outwardly healthy.
A comprehensive review published in Diabetologia revealed that a significant number of type 2 diabetes cases occur in people with normal or even below-normal Body Mass Index (BMI). In certain Asian and African populations, as much as 24% to 66% of diabetes cases are found in individuals who are not overweight. Although the overall risk of diabetes is higher among overweight or obese people, the incidence among normal-weight adults is steadily increasing — a trend that highlights the changing face of the disease.
Why Weight Isn't the Whole Story
These findings challenge the traditional view that excess body weight is the primary trigger for type 2 diabetes. While being overweight is a major risk factor, it is by no means the only one. In reality, several lesser-known factors can independently contribute to diabetes risk, even in people who are not visibly unhealthy.
Visceral Fat: The Hidden Danger
One of the most important, yet overlooked, factors is where fat is stored in the body. Even if someone has a normal BMI, they may still carry visceral fat — fat stored deep in the abdomen around organs like the liver and pancreas. This type of fat is especially harmful because it can:
-
Interfere with insulin signaling
-
Promote insulin resistance
-
Increase inflammation throughout the body
Imaging studies such as CT scans have shown that many “lean” individuals diagnosed with type 2 diabetes have abdominal fat distribution patterns similar to those seen in obese individuals, including increased visceral fat, fatty liver, and pancreatic fat deposits. These internal fat patterns can significantly impair how the body manages blood sugar.
Metabolic Health vs. Physical Appearance
Another key concept is the idea of being “metabolically unhealthy at a normal weight” (MUNW). People in this category may look fit and maintain a healthy BMI, but under the surface, they experience metabolic disturbances such as:
-
Elevated fasting blood glucose
-
Insulin resistance
-
Abnormal cholesterol or triglyceride levels
-
Chronic low-grade inflammation
These risk markers often go undetected because the individual doesn't meet the visual stereotype of someone at risk for diabetes. Unfortunately, many doctors and patients alike overlook these red flags, delaying diagnosis and intervention.
Modern Diets: Not Just About Sugar
In today’s food environment, diet quality matters just as much — if not more — than sugar intake alone. Many people who think they’re eating healthily unknowingly consume high levels of ultra-processed foods. These products, while sometimes low in added sugar, are often rich in:
-
Refined carbohydrates
-
Industrial seed oils
-
Chemical additives
-
Preservatives and flavor enhancers
According to a study in The Journal of the Academy of Nutrition and Dietetics, higher consumption of ultra-processed foods is directly linked to poorer blood sugar control (higher HbA1c levels) — even among people who don’t eat many sweets or sugary beverages.
Some commonly consumed foods that increase diabetes risk include:
-
White bread and pasta
-
Pastries and baked goods
-
Packaged frozen meals
-
Sugary drinks such as fruit juice, flavored milk, and energy drinks
-
Fast food and heavily processed takeaways
A Cautionary Tale
In the case of the 32-year-old teacher, although she regularly cooked at home and avoided junk food, she often consumed pastries and refined carbs without realizing how much they affected her blood sugar levels. Her eating habits, while seemingly harmless, were contributing to unseen spikes in blood glucose that gradually led to insulin resistance.
Her diagnosis serves as a wake-up call: health cannot be judged by appearance alone. The human body is complex, and how it processes food and stores fat varies widely from person to person.
The Takeaway: Rethinking Risk
Type 2 diabetes is increasingly being recognized as a multifactorial condition, not simply a consequence of poor lifestyle choices or excess body weight. Factors like:
-
Fat distribution
-
Genetic predisposition
-
Chronic inflammation
-
Diet quality
-
Metabolic response to stress
can all converge in subtle, hidden ways.
As cases of type 2 diabetes rise globally — especially among younger adults and normal-weight individuals — it’s critical for both the medical community and the public to shift away from outdated assumptions. Prevention and screening efforts must evolve to consider metabolic health as a whole, rather than focusing narrowly on weight or sugar consumption.
Ultimately, this teacher’s story is a powerful reminder: you can’t always see diabetes coming, but with the right knowledge, you can reduce your risk — no matter your size.
News in the same category


6 Benefits of Eating Garlic Before Bedtime

WARNING SIGNS OF POOR BLOOD CIRCULATION THAT MOST PEOPLE OVERLOOK AND HOW TO SPOT THEM EARLY
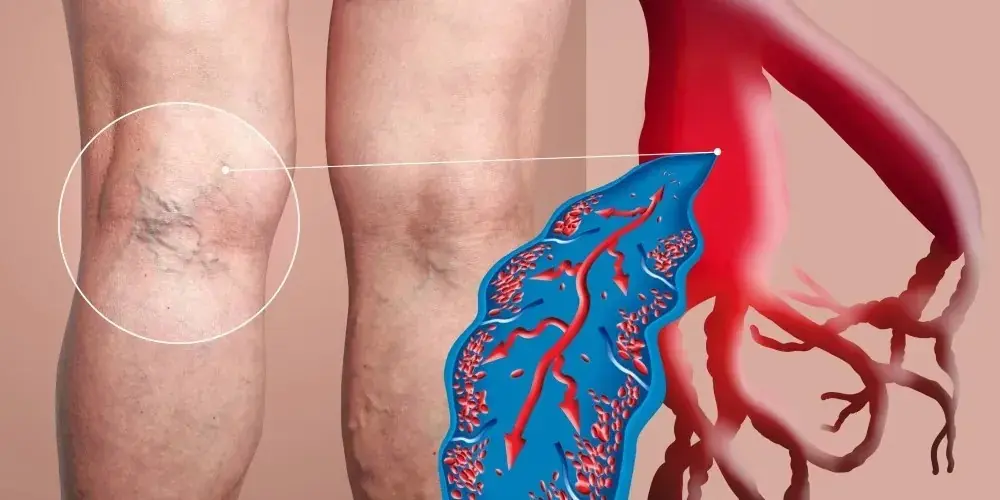
Thrombosis can strike suddenly — know the symptoms before it's too late

Secret that Dentists don't want you to know: Remove Tartar and Teeth Whitening in just 2 minutes
The #1 Enemy of Your Thyroid: Stop Eating This Food Immediately!
7 Warning Signs of a Heart Attack You Can Spot Up to a Month Before—And the One Deadly Sign You Must Never Ignore

This Food Helps Activate Your Body’s Stem Cells So It Can Repair Itself Naturally

These 4 Herbs Can Protect Your Brain From Alzheimer’s, Depression, Anxiety & Much More

Hidden Signs Constipation Is Affecting Your Whole Body

Doctor has message for anyone who takes collagen
Remove one item from your home to live longer, says a 92-year-old cardiologist

The Hidden Costs of Sleeping with the Wrong Person: What You Need to Know

Clean Your Blood Vessels Naturally

Cracked Heels Could Be a Warning Sign

SEVEN TYPES OF PAIN THAT SIGNAL MAJOR RED FLAGS FOR YOUR HEALTH

This Is What Happens to Your Body When You Add Turmeric to Your Daily Diet, According to Science
9 Signs of Diabetes That Appear at Night: What You Need to Know!
News Post

Lemon Seeds Can Save a Snakebite Victim Within Just One Minute If Used This Way

Why Keeping A Lemon In Your Bedroom Is A Great Idea

Put salt in your toilet. Here's why. This is something plumbers will never tell you

Guava Leaves for Blood Sugar Control: Nature’s Gift for Diabetics

Banana Blossom: Health Benefits, Recipes, and Uses

Common Mullein: Benefits and Uses of Nature’s Versatile Herb

Fig Leaves: Surprising Benefits and Uses

Inner Vitality Elixir: Benefits of Uda Seeds, Lemon, Aidan Fruit, and Ginger for Women’s Health

When Checking Out of a Hotel, Don’t Fold the Bedding—Not Knowing This Will Only Cause Trouble

Some of the Benefits of Castor Leaves and the Seed

The Versatile Uses of Stubborn Grass
Pour Beer into Table Salt to Solve Many Household Problems – Wish I Knew This Trick Sooner!
The Best Tea for Mornings and After Dinner: A Powerful Blend for Health

Mimosa Pudica Tea: How to Prepare and Health Benefits

If you have this plant in your garden, don’t cut it down – it’s incredibly valuable!

Euphorbia Hirta (Asthma-plant): Traditional Uses and Applications

Harnessing the Power of Goose Grass: A Guide to Its Preparation and Therapeutic Uses
The water pipe is clogged, do this way to solve it easily, no need to call a plumber
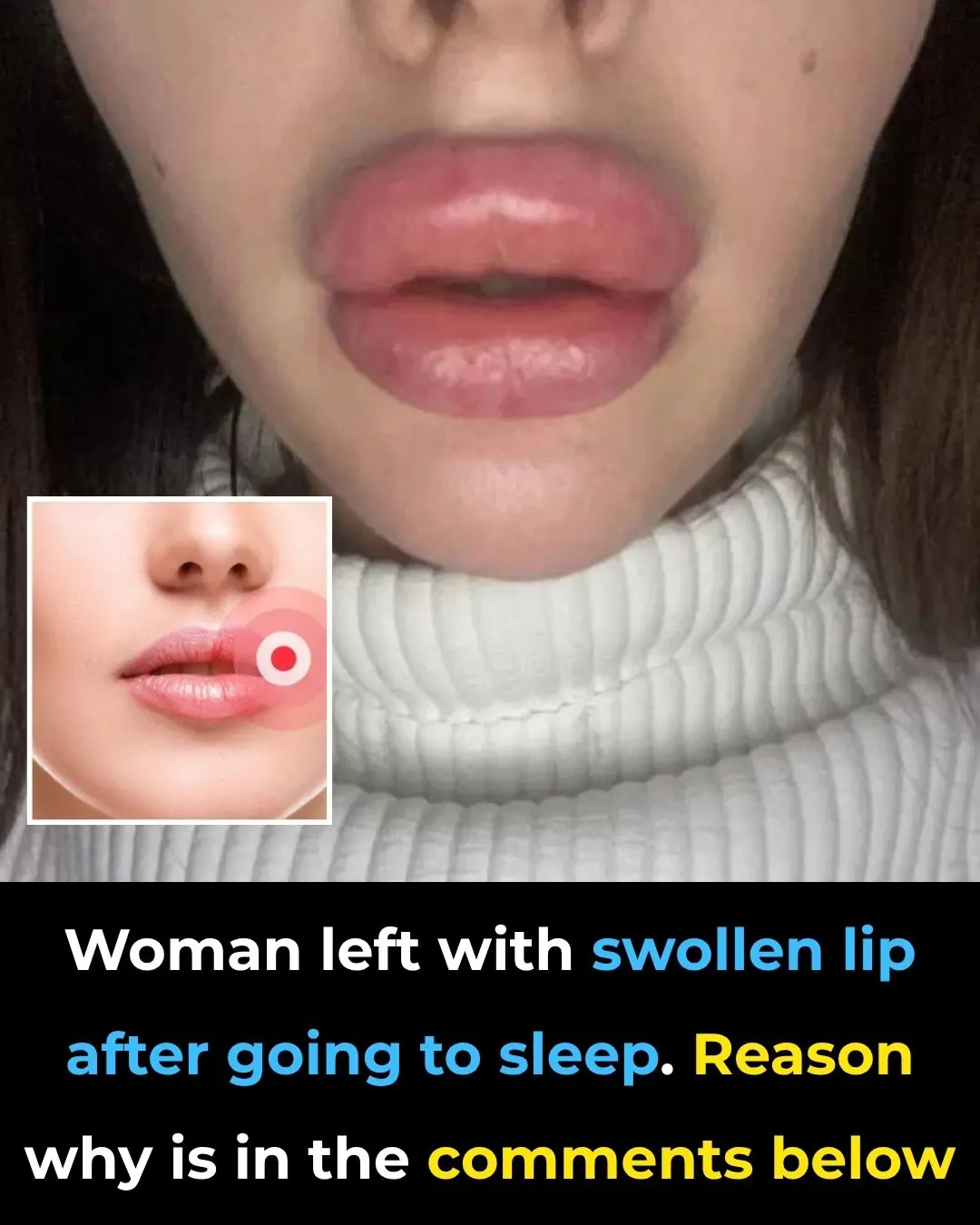
Woman Left with Swollen Lip After Centipede Bites Her in Sleep
