Tragic Medical Error: 5-Year-Old Girl Dies After Doctors Miss This Common Childhood Illness
Doctors claimed it was a simple viral infection, but a tiny girl lost her voice mere days after her illness started. They advised her parents to wait things out. Later on, they would learn that a simple test may have prevented her death and changed everything.
When Cassie started exhibiting symptoms of what doctors characterised as a common seasonal illness, she was five years old, active, and in her first year of school. The specialists who evaluated her were not alarmed by the symptoms, which were initially modest. However, something wasn’t quite right for her parents.
They were forced to rely on medical advice that would soon turn out to be gravely incorrect as Cassie’s condition continued to deteriorate. Her body was battling a bacterial infection that affects hundreds of millions of people globally and is frequently cured with a single course of antibiotics, but no one knew this. Cassie was never given that opportunity.
Early Symptoms and a Dismissive Diagnosis
It started with a scratchy voice and painful throat, which are so typical of young children that they hardly ever induce fear. However, Cassie lost her voice entirely after three days. Justin Sutton, her stepfather, and Jasmine, her mother, became worried. There was a strange feeling. Cassie was behaving strangely.
The family took her to a nearby physician in search of explanations. The evaluation was quick and simple. They were advised to wait for Cassie’s viral infection, which was diagnosed as a cold. Her problems were not investigated further.
Keeping her comfortable at home was the recommendation. Cassie’s condition did not improve even after she followed the doctor’s directions. Her voice hadn’t come back, and she was losing her vitality. Her parents continued to hope that time and rest would be sufficient, despite professional assurances.
Escalating Trouble and an Emergency Room Visit
Cassie’s respiration started to alter as the days went by. What began as silent exhaustion became obvious discomfort. Her stepfather later compared it like the laboured breathing of an emphysema sufferer or an asthma episode. Something more than a cold was obviously taking hold.
Cassie’s parents hurried her to the emergency hospital in alarm. There, medical professionals conducted COVID-19 and respiratory syncytial virus (RSV) testing, both of which yielded negative results. The family was informed once more that she most likely had a viral infection.
They were told to take Cassie home and keep an eye on her despite her increasing discomfort and respiratory problems. Antibiotics were not taken into consideration, and no bacterial testing were requested. Her parents were still looking for answers that the system was failing to provide when Cassie was sent home for the second time.
What Is Strep A?
Nobody thought of group A streptococcus, or strep A, one of the most prevalent but potentially harmful diseases among kids her age. Siblings, carers, teachers, and anyone in close contact situations can all easily contract the ailment, which mainly affects school-aged youngsters between the ages of five and fifteen.
Because of how easily the virus can spread from person to person, high-risk settings include homes, nursery schools, schools, colleges and even military camps. The most common symptom of strep throat, which is caused by Strep A, is inflammation of the tonsils, which are lymph nodes at the back of the mouth, and the throat.
In contrast to common colds, strep throat frequently manifests as fever, enlarged lymph nodes, and an abrupt, intense sore throat. Pharyngitis, or sore throat, is usually the result of the inflammation spreading to the surrounding area.
The diagnosis is easy. Antibiotics, usually amoxicillin or penicillin, are used in treatment. The presence of the bacterium can be verified with a simple throat swab. Alternative antibiotics can be provided to people who are allergic to penicillin. Medication can be administered by injection, liquid, or tablet.
To guarantee that the bacteria are completely eradicated, the entire course of treatment, which typically lasts 10 days, must be finished, even if symptoms start to improve sooner. Early cessation raises the possibility of problems or recurrence.
When strep throat is properly diagnosed and treated, it usually goes away in seven to 10 days. However, the delay may have irreparable effects if the diagnosis is incorrect, as it was in Cassie’s case.
Collapse at Home and Medical Response
Cassie’s condition did not stabilise even after she was released with orders to wait it out. Her symptoms at home rapidly progressed from worrisome to life-threatening. Breathing difficulties turned into an emergency.
In her mother’s arms, her lips became blue, and she began to slip in and out of awareness. Justin started CPR while they waited for aid to arrive after Jasmine promptly dialled triple-0. Before paramedics arrived and took over, he continued for 10 to fifteen minutes.
Westmead Children’s Hospital received Cassie via medical helicopter. Doctors there worked desperately to bring her back to life. However, her body had already suffered too much by the time she got there.
A Diagnosis That Came Too Late
Physicians at Westmead Children’s Hospital made every effort to bring Cassie back to life. They did continuous CPR for 78 minutes, but irreparable harm had already been done due to the lack of oxygen. Her parents were summoned for a meeting on August 28, 2023.
They learnt that Cassie had been declared brain dead there. The hospital only performed a throat swab after this. What none of the other tests had checked for was confirmed by the results. It was strep A that Cassie had.
If the bacterial infection had been discovered sooner, it may have been treated. In addition to dealing with the loss, her family had to deal with the fact that the illness was completely avoidable. The disease has been lurking in the shadows.
Global Prevalence and Risks
Cassie’s situation is by no means unique. Over 616 million new cases of Group A Streptococcus are diagnosed by medical professionals worldwide each year, making it one of the most prevalent bacterial illnesses. Approximately 500,000 of the instances end in death.
It is one of the most frequent reasons children visit a doctor in the United States, accounting for between 15 to 35 percent of children’s sore throat cases and 5 to 15 percent of adults’.
Even though it is common, it is usually missed in the first examination, particularly if the symptoms are similar to those of a viral cold. Testing should be done right away if there is fever, sore throat, and exhaustion without respiratory congestion, as cough is usually absent in strep A infections.
The group A streptococcus (GAS) bacteria that causes strep throat is the source of its name. This bacterium has over 120 strains, and although the majority of cases are benign, some strains can cause serious problems.
Rheumatic fever, a dangerous condition that can permanently harm the heart and its valves, can develop from strep throat if left untreated. The following symptoms can occur suddenly:
- A severe sore throat
- Fever that spikes quickly, often on the second day
- Chills
- Headache
- Loss of appetite
- Abdominal pain
- Nausea or vomiting
Notably, strep throat rarely manifests as a cough. This distinction is important since a patient’s cough and cold-like symptoms are more likely to be caused by a virus than by bacteria. But other strep A carriers may not exhibit any symptoms at all, rendering them unaware of their infection.
It is quite easy to spread strep throat. People with active symptoms are more contagious, but even those without symptoms can spread it. Respiratory droplets from coughing, sneezing, or even sharing cutlery can spread it.
When strep throat is properly diagnosed and treated, it usually goes away in seven to ten days. However, the delay may have irreparable effects if it is undiagnosed. However, such testing is rarely carried out unless expressly asked, as was the case with Cassie.
Children’s immune systems are still developing, thus the illness can worsen very quickly. The best preventative measures continue to be awareness and prompt action.
Cassie’s Final Gift on Jersey Day
Cassie’s family had to make decisions in the days after her death that no parent ever wants to make. They decided to honour her life by assisting others in the midst of their sorrow. The donation of Cassie’s organs took place on September 1, 2023. In Australia, the day fell on Jersey Day, a nationwide initiative to encourage organ and tissue donation.
View this post on InstagramA post shared by Jazz Worobez (@jazzyworo92)
That choice led to the life-saving transplantation of three youngsters. It was anticipated that all three recipients would fully recover. Knowing that Cassie could assist others gave her family a sense of purpose in an otherwise meaningless loss.
Her stepfather referred to her as a “real-life superhero,” a young girl who was able to alter the lives of three other families despite unthinkable circumstances.
View this post on InstagramA post shared by Jazz Worobez (@jazzyworo92)
Grief, Reflection, and a Plea for Awareness
Cassie’s family spoke of feeling numb while they got ready for her funeral, a condition that enabled them to carry on with their daily lives. The weight of what had transpired weighed heavily in the silence between preparations and farewells.
Nothing could bring Cassie back, but her parents kept thinking the same thing: things may have turned out differently. An antibiotic course could have saved her life. The warning symptoms had been present, and the infection was curable.
But blame was not their main concern. Making others aware was their top priority for the time being. They advised families to believe their gut feelings, seek for testing even when medical professionals reassure them, and speak up when something doesn’t feel right.
“But what I’ve said to everyone is we’re going to worry about those doctors later because that’s a fight for a different day,” Justin replied. Now, they wanted to keep other families from suffering the same grief. The story of Jasmine and Justin is not unique.

Just hours before their five-year-old daughter passed away next to her mother while she slept, another family in the UK went through a similar grief when physicians rejected her concerns.
News in the same category


If Your Body Suddenly Jerks While Falling Asleep, This Is What It Means

If You Eat Eggs Every Day
Vegetables To Clean Your Arteries And Prevent Heart Attack
Pain in This Part of the Body Could Indicate Cancer Cells are 'Awakening' – Both Men and Women Shouldn't Ignore It
10 Unconventional Signs of Liver Damage You Must Know About
14 Early Warning Signs You're Dangerously Low on Magnesium
How To Get Rid Of Phlegm and Mucus In Chest and Throat

Burnout: Tips for Coping When You Can’t Just Quit

Beautifully Unbroken: Living Fully and Imperfectly With Bipolar
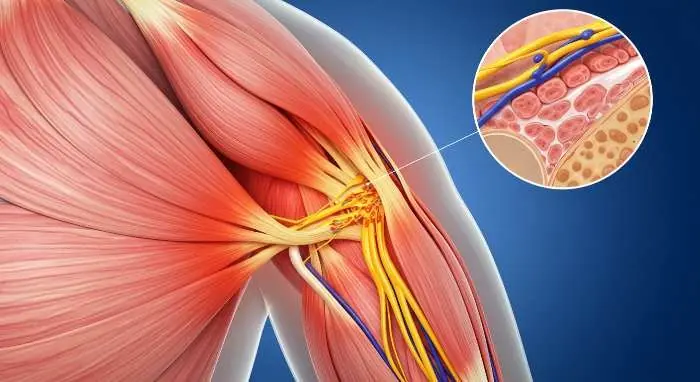
How to Get Rid of Muscle Soreness: Home Remedies That Really Work

15 Common Cancer Symptoms You Shouldn’t Ignore

New Blood Test Shows Over 90% Accuracy for Lyme Disease
Is AI Use Causing Endoscopists to Lose Their Skills?

Florida Man Struck by Lightning Wakes Up With Heart Beating 265 Times a Minute

1 cup before bed: end restless nights and repair your nerves

Top 10 Nutrients in Foods that Clean Your Arteries Fast

Scientists Uncover A Natural Way to Restore Vision

Remedy For Falling Asleep Quickly

Sleeping Enough But Still Tired
News Post

Arkansas woman accidentally discovers $27,000 dollars after kicking 'spiderweb' in park

Exactly how virus carried by 'Frankenstein' rabbits growing black 'tentacles' spreads following urgent warning from experts
The Elders' Teachings Are Not Wrong: "The Kitchen Should Not Face Three Directions, and the Bed Should Not Be Placed in Three Locations"

5 Types of Plants That Snakes Love: If You Plant Them in Front of Your House, Remove Them Immediately Before It’s Too Late

If Your Non-Stick Pan Has Lost Its Coating, Don’t Rush to Throw It Away. Follow This Trick to Turn Your Old Pan Into a Like-New One.

Cooking Oil Often Splashes When Frying? Add This Ingredient to the Pan, and You Won't Have to Worry About Oil Splattering or Sticking to the Pan
Is It Correct to Close the Door When Using the Air Conditioner? Here Are 5 Mistakes That Can Cause Your Electricity Meter to Increase 2-3 Times
Boiling Eggs with Just Water is Not Enough: Add This Ingredient, and the Eggs Will Cook Evenly, Have a Rich Flavor, and the Shells Will Peel Off Easily

Do Not Ignore These 10 Warning Signs That Your Kidneys May Be In Danger

Buying Meat and Just Placing It Directly in the Freezer for Storage is a Mistake: The Shop Owner Shares a Trick to Keep Meat 'Fresh for a Whole Year' Without Spoiling

Sprinkle a Little of This Powder into the Oil Before Frying, Everyone Will Be Amazed by Its Incredible Effectiveness

If Your Body Suddenly Jerks While Falling Asleep, This Is What It Means

What Is This Button In The Car For

How Long Cooked Food Can Stay In The Refrigerator

If You Eat Eggs Every Day
Vegetables To Clean Your Arteries And Prevent Heart Attack
Pain in This Part of the Body Could Indicate Cancer Cells are 'Awakening' – Both Men and Women Shouldn't Ignore It
10 Unconventional Signs of Liver Damage You Must Know About
14 Early Warning Signs You're Dangerously Low on Magnesium