Another US doctors’ group breaks with federal policy, recommends COVID-19 vaccines for all adults

A New Rift in COVID-19 Vaccine Guidance: Family Doctors vs. Federal Policy
For nearly five years, the COVID-19 pandemic has reshaped how the world thinks about public health, risk, and personal responsibility. Vaccines—once celebrated as a miraculous turning point in 2021—have since become the subject of shifting policies, waning urgency, and deeply divided public opinion. Today, the debate has entered yet another phase: the American Academy of Family Physicians (AAFP) has formally recommended that all adults aged 18 and older receive a COVID-19 vaccine. Their guidance also explicitly includes pregnant women and very young children, putting them in clear contrast to the U.S. federal government’s narrower approach.
On paper, the divergence may look subtle. In practice, it carries weighty consequences, shaping how families decide in clinics, living rooms, and workplaces across the country. While the federal government currently focuses updated vaccine eligibility primarily on seniors and those with serious health risks, the AAFP’s call for broader coverage raises a deeper question: should vaccination be a targeted intervention for the most vulnerable, or a universal tool for prevention across the population?
What the AAFP Is Saying
The AAFP’s recommendation reflects a proactive philosophy rooted in everyday clinical encounters. Family doctors are often the first point of contact for patients trying to navigate health choices, and their guidance carries significant trust. By urging all adults to get vaccinated, the AAFP aims to simplify messaging, reduce public confusion, and provide broader layers of protection—not only against the virus as it exists today but also against variants that could emerge in the future.
This approach reflects what public health experts call the precautionary principle: when the risks of illness remain and prevention is relatively safe and low-cost, the wiser path is to act broadly rather than narrowly.
For children, the guidance is carefully differentiated. The AAFP explicitly recommends vaccination for infants and toddlers aged six to twenty-three months—a group often more vulnerable to respiratory illnesses in general, even if COVID-19 itself tends to be less severe in young kids. For children between two and eighteen, however, the AAFP stops short of universal recommendation, instead encouraging parents and physicians to weigh risks on a case-by-case basis. This attempt at balance recognizes both medical nuance and parental concern.
Pregnant women are another key group. Research across the pandemic has shown that pregnancy increases vulnerability to severe outcomes from COVID-19, including higher rates of hospitalization, ICU admission, and complications. The AAFP highlights maternal vaccination as a protective double strategy: reducing risks for the mother while potentially passing protective antibodies to the newborn. This echoes long-standing practices with other vaccines, such as influenza and pertussis, where vaccinating during pregnancy has been shown to safeguard both mother and infant.
Taken together, these recommendations reflect not a blanket expansion but a layered approach—protecting groups with special vulnerabilities while still promoting broad coverage for adults.
Federal Policy Today
By contrast, federal policy under the U.S. Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) has narrowed considerably since the early days of the pandemic. At present, routine vaccination is primarily advised for those aged 65 and older and individuals with underlying conditions that heighten the risk of severe illness.
This “targeted protection” strategy rests on several points. First, hospitalization and death rates have plummeted compared to the crisis years of 2020–2022. A large share of the U.S. population now has at least partial immunity, whether from prior vaccines, past infections, or both. For younger, healthy adults, the likelihood of severe outcomes is statistically low. Regulators therefore question whether vaccinating millions of lower-risk individuals provides enough collective benefit to justify the costs and logistics.
Second, the federal government faces real resource pressures. Vaccination campaigns require funding, manufacturing capacity, supply chain coordination, and staffing—all of which compete with other pressing health priorities. Narrowing eligibility allows policymakers to concentrate resources on the most at-risk populations.
Finally, officials remain wary of vaccine fatigue. After years of shifting booster schedules and changing eligibility rules, public trust has frayed. Federal leaders fear that urging repeated doses for those at minimal risk could undermine confidence, fueling skepticism not only toward COVID vaccines but toward public health recommendations more broadly.
Why the Two Sides Differ
At the core of this divide lies a philosophical tension about risk and responsibility.
-
AAFP’s perspective: Prevention should cast a wide net. Even if severe cases in younger adults are rare, they are not nonexistent—and family physicians witness the unpredictability of illness firsthand. Their focus is less on statistics and more on avoiding preventable harm in individual lives.
-
Federal perspective: Policies must be efficient, sustainable, and data-driven at a population scale. With limited resources and declining risk, targeted protection for the most vulnerable is seen as both pragmatic and scientifically justified.
Both groups are interpreting the same evolving evidence base, yet their takeaways differ. For the AAFP, uncertainty about future variants strengthens the case for broad vaccination. For federal regulators, uncertainty justifies restraint until stronger data emerge. This isn’t a battle over science but a clash over how science should guide policy.
Real-World Impacts
For families, these differing recommendations are more than abstract debates. They directly shape decisions made in clinics and at kitchen tables.
-
Parents of toddlers: Under federal policy, parents might assume vaccination isn’t necessary, especially if their pediatrician follows the narrower government line. But under AAFP guidance, another doctor might strongly recommend it, leaving families to navigate contradictory advice.
-
Pregnant women: With federal agencies silent, some women may conclude vaccination isn’t important during pregnancy. The AAFP’s explicit recommendation could shift those choices, preventing complications but also raising confusion when federal and professional advice diverge.
-
Healthy younger adults: A 30-year-old might dismiss vaccination if relying only on federal messaging. But if their physician cites the AAFP’s stance, they may rethink—especially if they live with older relatives or work in high-exposure environments.
These scenarios illustrate how policy fractures translate into human dilemmas. It’s one thing to read about conflicting recommendations in headlines; it’s another to sit in a doctor’s office faced with a decision about your own child, your own pregnancy, or your own health.
The Bigger Picture
The disagreement between the AAFP and federal agencies reflects a broader challenge that has haunted pandemic response since 2020: the struggle to deliver clear, consistent, and trusted health communication in a rapidly shifting landscape. When respected authorities diverge, patients are left to wonder whom to believe, while physicians must shoulder the burden of explaining not just the medicine but the politics behind the medicine.
The lesson is sobering: science alone cannot sustain public trust. Without alignment, transparency, and empathy in communication, even sound evidence risks getting lost in the noise.
As the U.S. continues to transition from pandemic crisis to long-term management, these debates will likely resurface with every new variant, every booster campaign, and every shift in public health priorities. Whether the future leans toward targeted protection or universal precaution, the underlying challenge remains the same—balancing individual choice with collective safety in a society still learning how to live with the aftershocks of COVID-19.
News in the same category
Think Bottled Water Is Safer Think Again

5 Early Warning Signs of Cervical Cancer That 90% of Women Overlook
Cervical cancer is not a silent killer—it sends out warnings. The challenge is whether women notice and act on them in time.

8 Shocking Toilet Clues That Could Signal Cancer: Don’t Ignore These Early Warnings
Many people dismiss subtle changes in bathroom habits as minor or temporary issues. However, certain unusual signs when you go to the toilet could be early red flags of serious health problems. Recognizing them in time can make the difference between earl

Study Reveals How Earth’s Orbit Triggers Ice Ages, And There’s One in The Next 11,000 Years

This 3,200-Year-Old Tree Is So Big, It’s Never Been Captured In A Single Photograph…
Travel Coast-to-Coast by Train and See America’s Greatest Sites For Just Over $200
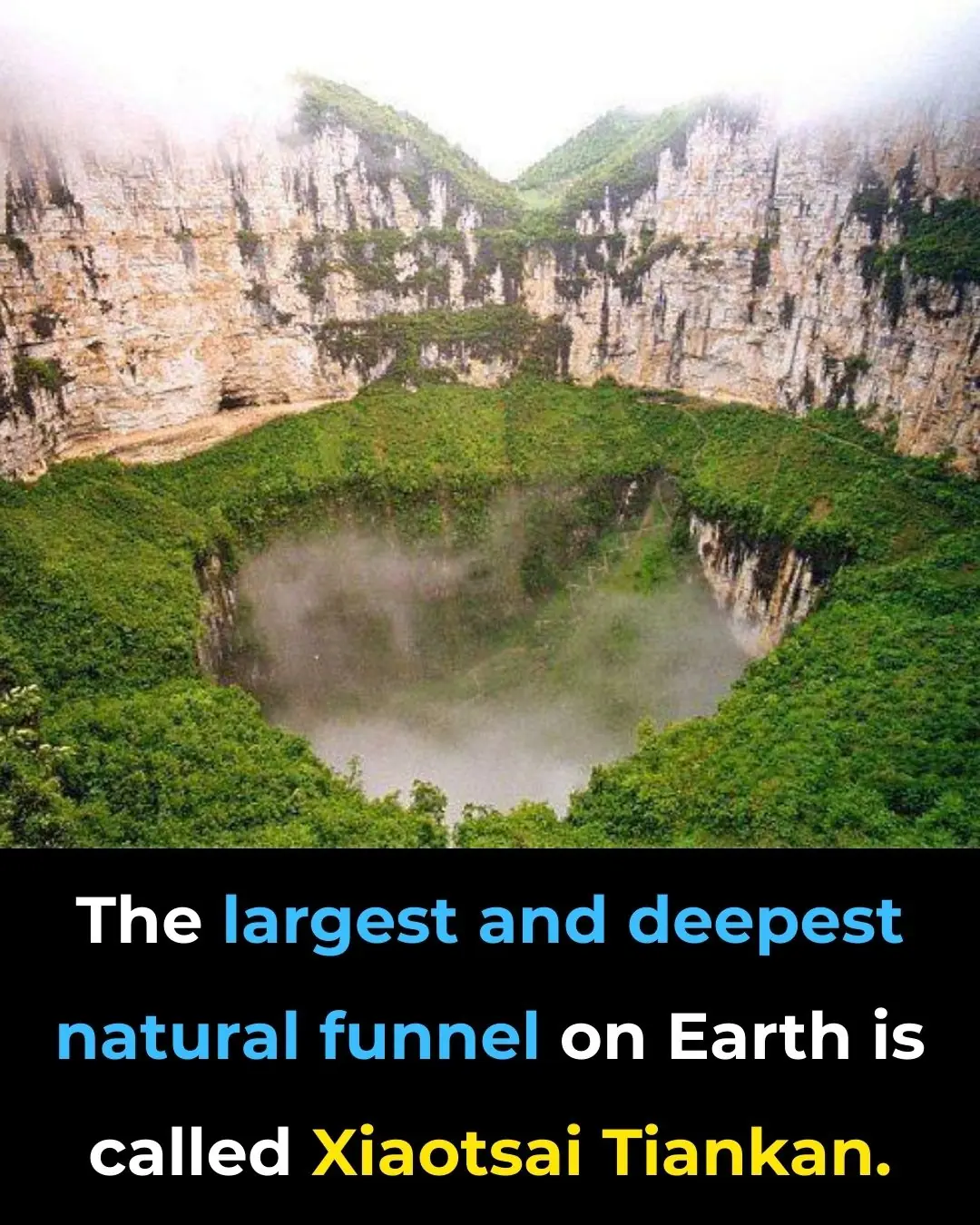
Descend Into the Heavenly Pit: Exploring Xiaozhai Tiankeng, the World’s Deepest Sinkhole

The Walking Trees of Ecuador: They Reportedly Move Up to 20 Meters Per Year

How to See Halos, Sun Dogs and Other Delights of the Daytime Sky
When someone in the family passes away, you should know that you should not keep these 4 relics for your children and grandchildren.
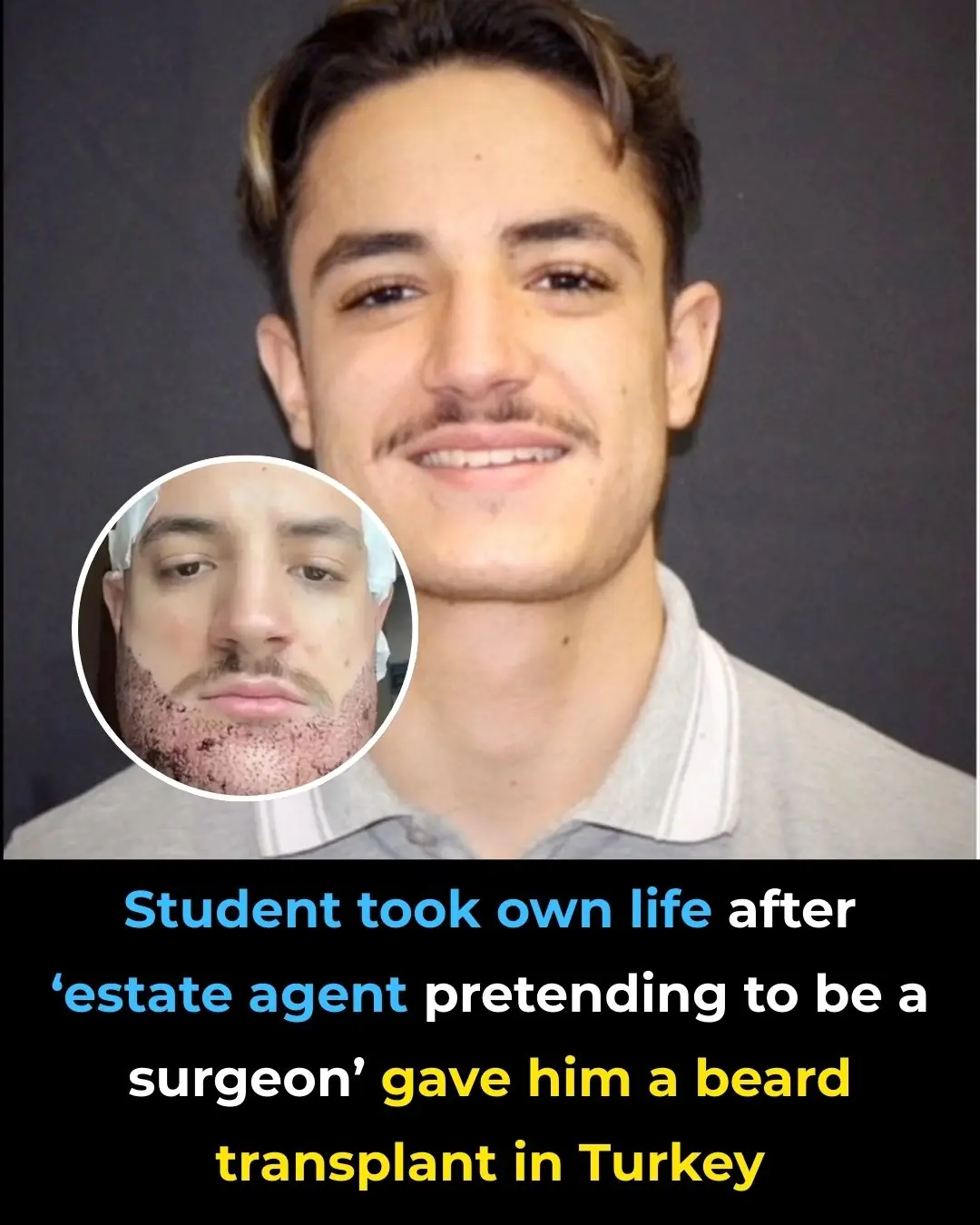
Student dies by suicide after undergoing a beard transplant in Turkey from an ‘estate agent posing as a surgeon’

The Sun Begins Killing off Elon Musk’s Starlink Satellites as Scientists Sound Alarm

Never Leave a Charger in Outlet Without Phone. Here Are the Top 6 Reasons Why

3 Coffee Types That Can Add Years to Your Life and Shield You from Heart Disease and Stroke
Enjoying two to three cups of ground, instant, or decaf coffee daily can be a powerful step toward a longer and healthier life.

Bananas Are Packed With Nutrients, But These 4 Groups Should Avoid Eating Too Many
Bananas are undeniably one of the most versatile and beneficial fruits. From boosting digestion to supporting heart health, they offer a wide range of nutrients. However, they are not suitable for everyone.
9 Early Warning Signs of Stomach Cancer You Should Never Ignore
. Paying attention to subtle but persistent warning signs, combined with regular health screenings, offers the best chance for timely intervention.
MAHA Chief Medical Advisor Dr. Aseem Malhotra Just Declared That No One Should Have Ever Taken the COVID mRNA Vaccines.

New mRNA Shot Turns Immune Cells Into Cancer-Killers Directly Inside the Body, Study Finds
News Post

Remove these 7 everyday foods from your fridge—they could raise cancer risk
The Anti-Cancer Diet: Cancer Fighting Foods to Help Prevent Cancer (Evidence Based)
Drinking guava leaf water, the body receives these 6 great benefits

With just one lemon: You can get rid of all the ants in your house in no time, never to return.

Used Coffee Grounds: Don’t Throw Away Money – Amazing Everyday Uses You Should Know
I Put 3 Ice Cubes in the Washing Machine Like My Neighbor Did—What Happened Surprised Me

5 Best Drinks for Kidney Health — Especially #1, Free and Longevity-Boosting

10 Best Potato Face Packs for Glowing, Clear, and Youthful Skin
From acne and pigmentation to dryness and aging, potatoes address nearly every skin issue without side effects or hefty price tags. With consistent use, these DIY packs can reveal skin that’s clearer, smoother, and radiant.

Reverse Premature Grey Naturally with This Easy Homemade Hair Oil
While it is natural for hair to turn grey as we age, there are many natural remedies, dietary changes, and cosmetic treatments available that can help slow down or reverse the process.
Donald Trump Says There Could Be People in Epstein Files Who ‘Don’t Deserve to Be’ There in Shocking Statement
Clean Your Kidneys and Urinary Tract Naturally: One Teaspoon a Day
Think Bottled Water Is Safer Think Again
A Surprising Drink That May Help Prevent Cancer – And It's Not Tea or Coffee
How To Get Rid of Phlegm And Mucus

5 Early Warning Signs of Cervical Cancer That 90% of Women Overlook
Cervical cancer is not a silent killer—it sends out warnings. The challenge is whether women notice and act on them in time.

8 Shocking Toilet Clues That Could Signal Cancer: Don’t Ignore These Early Warnings
Many people dismiss subtle changes in bathroom habits as minor or temporary issues. However, certain unusual signs when you go to the toilet could be early red flags of serious health problems. Recognizing them in time can make the difference between earl

3 Powerful Ways to Keep Snakes Out of Your Home and Protect Your Family
By combining natural repellents, careful use of traditional methods, and the protective instincts of pets, households can greatly reduce the likelihood of encountering these stealthy reptiles.

Study Reveals How Earth’s Orbit Triggers Ice Ages, And There’s One in The Next 11,000 Years
