
Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]
Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]
What if the “perfect” blood pressure number you’ve been told to strive for — 120 over 80 — isn’t quite as perfect as it seems? What if, for some people, that golden standard might actually cause more harm than good? It sounds almost heretical, considering how deeply ingrained this number has become in modern health advice. But medicine, when practiced wisely, recognizes individuality — and your ideal blood pressure should depend on you, not on a rigid formula designed for the masses.
We’ve been conditioned to believe that 120/80 is the universal symbol of cardiovascular wellness. Yet, human bodies are far from identical. Age, genetics, stress levels, and lifestyle all shape what “healthy” looks like. The relentless pursuit of a single, universal number can lead to unnecessary medication, fatigue, and even serious harm. It’s time to rethink what your blood pressure should be — based on science, context, and common sense.
This isn’t about denying the dangers of truly high blood pressure. Instead, it’s about questioning the culture of over-treatment and blind number-chasing that has infiltrated modern healthcare. With insights from Dr. Suneel Dhand, we’ll explore why your personal ideal might differ from the textbook standard, the hidden risks of driving your pressure too low, and how to regain control of your health through personalized care and informed decision-making.
Key Takeaways
-
The “120/80” Target Isn’t Universal: This benchmark doesn’t suit everyone, particularly older adults or those with specific health conditions.
-
Over-Treatment Can Be Risky: Excessive medication can push your blood pressure too low, causing dizziness, confusion, or even organ damage.
-
Your Ideal Blood Pressure Evolves with Age: As your arteries stiffen naturally, slightly higher numbers can be a sign of healthy adaptation, not disease.
-
Accurate Home Monitoring Empowers You: Measuring your own blood pressure correctly gives you data that truly reflects your body’s reality.
-
Lifestyle Is the Real Medicine: Diet, stress, sleep, and physical activity are far more powerful than most realize.
-
Be Your Own Advocate: Don’t be afraid to question your treatment plan. Your body’s signals matter more than a chart on a wall.
1. What Do Those Blood Pressure Numbers Really Mean?
To understand why the “ideal” may not be universal, we need to revisit the basics. When you get a reading — say, 120/80 mmHg — you’re seeing two measurements:
-
Systolic (Top Number): The pressure in your arteries when your heart contracts and pumps blood.
-
Diastolic (Bottom Number): The pressure when your heart relaxes between beats.
Doctors often emphasize the systolic number because it tends to rise with age. But obsessing over lowering it at all costs can backfire. Your blood pressure isn’t static; it naturally fluctuates depending on your emotions, activity, temperature, and even hydration levels. That variability is part of being human — not necessarily a sign of illness.
2. The Trap of “Guideline Rigidity”: Treating Numbers, Not People
Medical guidelines are designed to simplify treatment, but they can unintentionally oversimplify patients. When we apply a single standard — 120/80 — to every adult, regardless of context, we stop practicing medicine and start managing statistics.
Consider the difference between a 30-year-old marathon runner and an 80-year-old woman with arthritis. Should both aim for the exact same blood pressure? Of course not. Yet many are prescribed medications until their numbers match this arbitrary “ideal.” This approach ignores symptoms like fatigue, dizziness, and brain fog — all signs that your body may be telling you something’s off.
Health isn’t a race to hit perfect numbers. It’s about balance, function, and how you feel day to day.
3. The Hidden Dangers of Blood Pressure That’s Too Low
We constantly hear warnings about hypertension — and rightly so. But what about hypotension, or blood pressure that drops too low? This under-discussed issue affects millions, especially older adults on multiple medications. When blood pressure falls below what your organs need, oxygen and nutrients can’t reach vital tissues — a condition known as under-perfusion.
Symptoms include:
-
Dizziness or lightheadedness
-
Confusion and poor concentration (“brain fog”)
-
Fatigue and weakness
-
Fainting or falling — often leading to injuries in seniors
Your brain and kidneys are especially sensitive to low blood flow. In older patients, this can mimic dementia or accelerate kidney failure. Ironically, treatments meant to protect health sometimes end up creating new dangers.
4. Why Age Changes the Game
As you age, your arteries naturally lose flexibility — a process called arteriosclerosis. To push blood through these stiffer vessels, your body may need slightly more pressure. In this sense, a systolic reading of 140 or even 150 can be normal and necessary for older adults.
Research has revealed a U-shaped curve in mortality rates among seniors: both very high and very low blood pressures are linked to poorer outcomes, while moderate readings often fare best. This means that “lower” isn’t automatically “better.” Forcing a 90-year-old’s blood pressure down to 115 might cause fainting spells or cognitive decline, not improved longevity.
5. The Silent Epidemic of Over-Medication
Here’s a true story: a 78-year-old man who’d been on blood pressure medication since his forties kept feeling weak and dizzy. One morning, he nearly collapsed — his blood pressure was 78 systolic, dangerously low. Over time, doctors had simply added new medications without reassessing whether he still needed the old ones. Once his treatment was adjusted, he quickly felt better.
This is what’s known as polypharmacy — the stacking of multiple drugs without ongoing evaluation. It’s alarmingly common and often overlooked. Millions are over-medicated not because of negligence, but because our healthcare system rewards treatment volume more than treatment wisdom.
6. How to Take Back Control: Home Blood Pressure Mastery
Monitoring your blood pressure at home isn’t just helpful — it’s empowering. It allows you and your doctor to see the real picture instead of relying on a single, possibly stress-inflated clinic reading.
Here’s how to do it right:
-
Use an upper-arm cuff (brands like Omron are reliable). Wrist cuffs are convenient but often inaccurate.
-
Prepare correctly: Rest for at least 5 minutes, avoid caffeine, smoking, or exercise 30 minutes prior, and keep your arm level with your heart.
-
Be consistent: Measure twice daily — morning and evening — and take three readings each time.
-
Keep a log: Record your numbers for two weeks and bring them to your doctor. Consistent patterns tell a clearer story than one-off readings.
This simple routine turns you from a passive patient into an active participant in your own care.
7. “White Coat Hypertension”: When Stress Skews Your Results
Ever notice your blood pressure is higher at the doctor’s office? That’s white coat hypertension, and it’s surprisingly common. The stress of the visit — traffic, waiting, or anxiety — can raise your numbers temporarily. Home monitoring helps distinguish true hypertension from these fleeting spikes.
A smart tip: ask your doctor to check your blood pressure at the end of your appointment, after you’ve relaxed. You’ll likely see a more accurate result.
8. The Real Solution: Reverse High Blood Pressure Naturally
For many people, especially those under 60, high blood pressure stems from insulin resistance — the body’s impaired ability to process sugar efficiently. This leads to inflammation, stiff arteries, and sodium retention. Fortunately, lifestyle changes can reverse much of this damage.
Your natural medicine chest includes:
-
Nutrition: Prioritize whole, unprocessed foods rich in potassium, magnesium, and fiber.
-
Exercise: Move daily — walking, swimming, dancing — consistency matters more than intensity.
-
Stress Reduction: Meditation, nature time, and deep breathing calm the nervous system.
-
Sleep Quality: Poor rest raises stress hormones and directly increases blood pressure.
In many cases, consistent lifestyle improvements can help reduce or even eliminate the need for medication — under proper medical supervision.
Conclusion: Health Is Personal, Not Mathematical
It’s time to step away from industrialized medicine’s one-size-fits-all model and embrace a personalized, human-centered approach. If your numbers look “ideal” on paper but you feel drained, foggy, or unwell, that’s not true health. The goal isn’t perfection on a monitor — it’s vitality, clarity, and quality of life.
You are not just a chart. You are a complex, adaptive organism. Partner with a doctor who listens, tracks your progress holistically, and helps you find the right balance — not just the “right number.” Because real health is not about chasing 120/80; it’s about feeling strong, steady, and alive in your own body.
News in the same category


The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup

Forget Calcium — Doctors Say This Is the #1 Exercise for the Strongest Bones

This Ends Insulin Resistance (in Days, Not Years)

7 Warning Signs of Diverticulitis Most Doctors Miss
Medicinal Health Benefits of Turmeric, Curcumin and Turmeric Tea Based on Science

The Best Foods to Cleanse and Prevent Clogged Arteries

Capsaicin Stops Heart Attacks And Destroys Cancer Cells
17 Signs Your Body Is Too Acidic And 9 Ways To Quickly Alkalize It
Adrenal fatigue: what it is and 17 all-natural ways to fix it fast

Colon Cleansing With Kefir and Flaxseed Meal
Apple extract kills colon cancer cells better than chemotherapy drug
12 surprising foods that help dissolve blood clots naturally
News Post

7 Common Health Issues That Keep Appearing Could Be Early Warning Signs of Cancer

Small Life Hacks That Can Be Life-Saving
How to Sharpen Dull Scissors Without a Sharpening Stone: Simple and Effective Method

The Best Scientifically Proven Foods to Cleanse Your Liver
Flush the toxins silently damaging your kidneys — with these 13 powerful cleansing foods

The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

When Staying Alone in a Hotel: Place Two Cups on the Door Handle – A Small Action with Big Benefits

15 Things You Should Never Do to Protect Yourself from Lightning During Thunderstorms

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
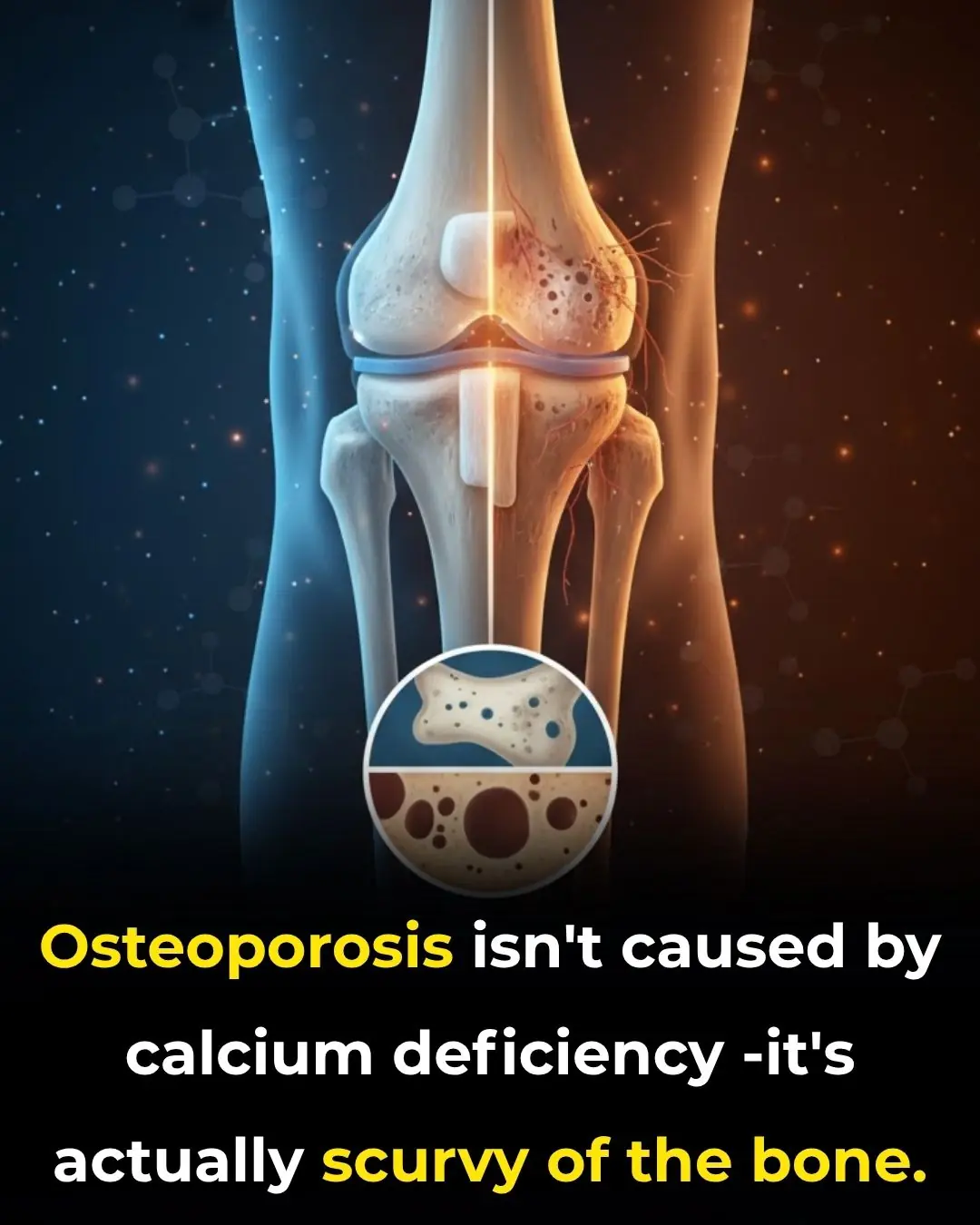
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup
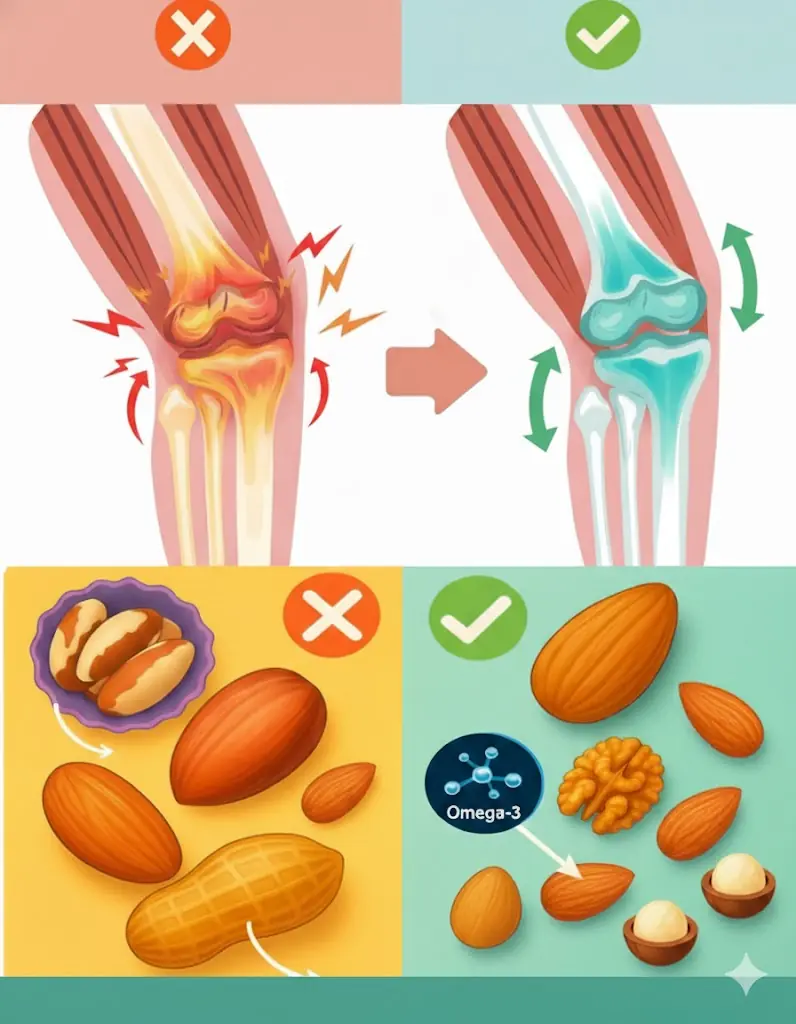
The Ultimate Nut Guide for Seniors: 4 Healthy Choices and 4 to Skip

The Man Who Walks for Dogs: Edgardo Perros’ 8,500-Mile Mission of Compassion

The Dog Who Went Out and Never Came Back the Same
To cook any kind of fish, just add a handful of these leaves: the fish will lose all its fishy smell and the meat will be rich and firm.

Great tips when growing pothos, in just 3 months the plant will form a beautiful green carpet
