
This Ends Insulin Resistance (in Days, Not Years)
This Ends Insulin Resistance (in Days, Not Years)
Have you noticed that post-meal crash that leaves you desperate for a nap? Or that stubborn “spongy” fat collecting around your midsection that just won’t budge, no matter how hard you try? Maybe you’re constantly craving sugar or carbs, yet somehow still feel drained.
Here’s the truth: it’s not a lack of willpower — it’s a communication breakdown inside your cells. A microscopic traffic jam that leaves your body unable to properly use the fuel it already has. That’s insulin resistance, and it’s not just a precursor to diabetes — it’s a metabolic malfunction driving many of today’s chronic diseases, from heart problems to premature aging.
Today, we’ll break down what insulin resistance really is, how it develops, and why even lean, healthy-looking people can have it. Most importantly, we’ll show you how to reverse it — in days, not years — by resetting the cellular switches that control your metabolism.
(Based on the insights of metabolic health expert Thomas DeLauer)
Key Takeaways
-
Insulin resistance and diabetes are not the same thing. The former is reversible; the latter is its end-stage consequence.
-
Lean people can be insulin-resistant too. “Thin on the outside, fat on the inside” is more common than you think.
-
Inflammation and fat-derived molecules (DAGs) clog your cells’ ability to respond to insulin.
-
Simple daily actions — strategic nutrition, movement, fasting, and targeted supplements — can unjam your metabolism fast.
Insulin Resistance vs. Diabetes: The Fire Before the Inferno
Think of insulin resistance as a smoldering ember, and type 2 diabetes as the full-blown blaze. Both involve disrupted sugar metabolism, but insulin resistance is the stage where you can still extinguish the fire — and often, quite rapidly.
Here’s how it works: after you eat, your blood sugar rises. Your pancreas releases insulin, a hormone that acts like a key, unlocking your muscle cells so glucose (sugar) can enter for energy.
But when your cells become insulin-resistant, they stop “listening” to that key. The lock gets rusty. Your pancreas compensates by releasing more and more insulin to force the sugar in. On a standard blood test, your glucose might look fine — but only because your insulin is sky-high, frantically working overtime.
This is why many people feel fatigued, foggy, hungry, and inflamed long before they ever get diagnosed. Their doctor might say, “Your blood sugar’s normal,” missing the fact that their insulin levels are screaming for help.
Who Really Has Insulin Resistance?
We’ve been taught to picture insulin resistance as a problem for middle-aged, overweight people. But research paints a much broader — and more alarming — picture.
A 2024 study published in The Journal of Clinical Endocrinology & Metabolism found that a surprising number of young adults (ages 18–44) already have measurable insulin resistance. Even more shocking: about half of them are not obese.
This “TOFI” phenomenon — Thin Outside, Fat Inside — means that people who appear lean can still have internal fat accumulation around their organs (visceral fat), which silently disrupts their metabolic function.
And the consequences go far beyond weight gain. Insulin resistance:
-
Accelerates atherosclerosis (hardening of the arteries)
-
Fuels inflammation and oxidative stress
-
Increases risk of Alzheimer’s (sometimes called “type 3 diabetes”)
-
Triggers hormonal imbalances, especially in women (PCOS)
Even mild insulin resistance can kick off glycation, where excess sugar “caramelizes” proteins and collagen — aging your skin, stiffening your joints, and damaging blood vessels. In many ways, it’s the root cause of modern metabolic decline.
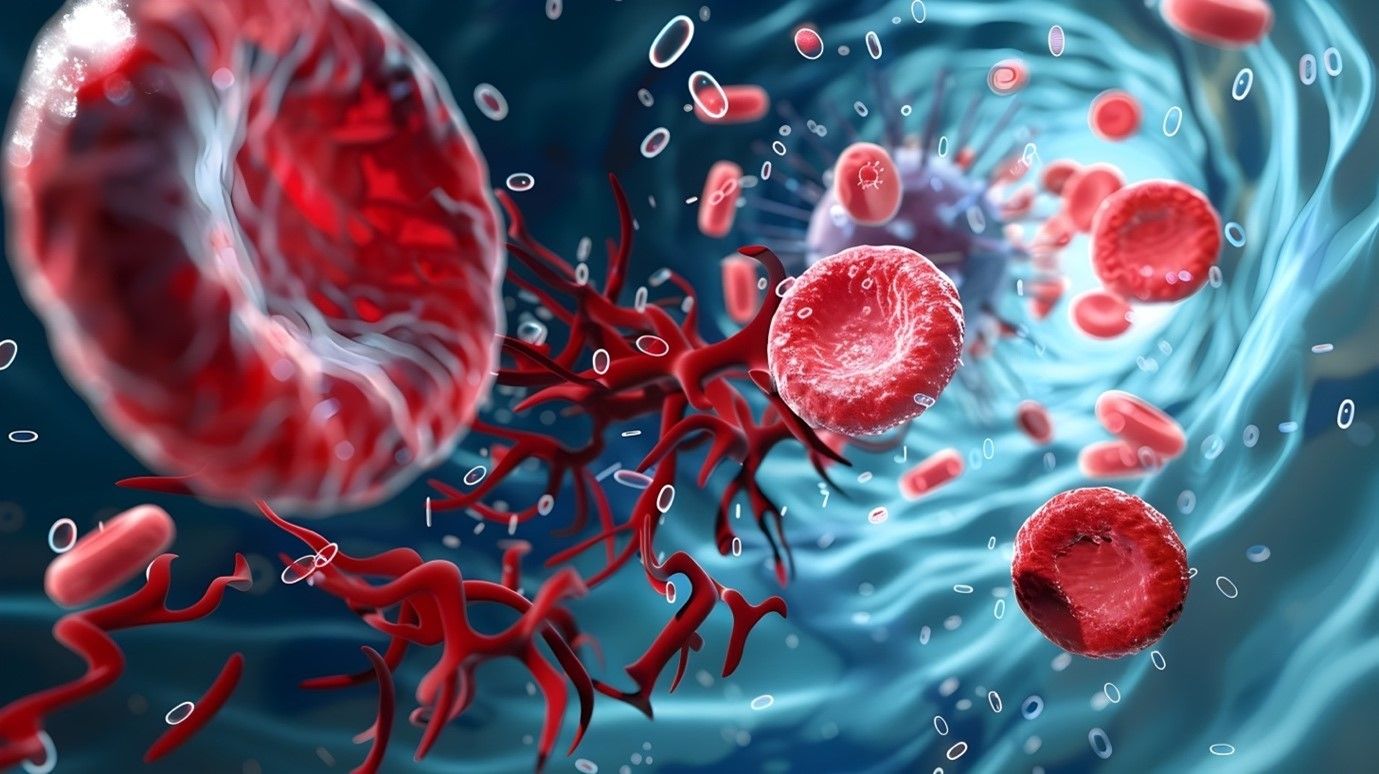
What’s Really Happening Inside Your Cells
Let’s zoom in on the cellular level.
Your muscle cells have special doorways for glucose called GLUT4 transporters. Insulin is supposed to send the signal that opens those doors. But when the system is overloaded — too much glucose, too much fat, too much stress — the signal gets jammed.
Why? Because of sticky fat molecules called diacylglycerols (DAGs). When your fat cells reach capacity, they start leaking fatty acids into your bloodstream. Those fatty acids infiltrate your muscles and liver, where they’re turned into DAGs — a sludge-like substance that literally blocks the insulin signal.
Picture this: insulin is pressing the remote to open your garage door, but inside the mechanism is gummed up with grease. The door doesn’t open. Glucose piles up outside (in your bloodstream), and your body goes into panic mode.
The result? Fatigue, hunger, and eventually, damage to your organs from chronically elevated insulin.
Your Insulin Resistance Reset Toolkit
Here’s the best part: this is reversible — and often quickly. You can restore insulin sensitivity in days to weeks, not years. The key is to unjam those cellular doorways, lower inflammation, and retrain your body to burn stored fat efficiently.
Step 1: Take a Post-Meal Walk
If your “remote” isn’t working, open the door manually.
A 15–20 minute walk after eating activates a separate energy pathway (AMPK) that bypasses insulin entirely, forcing glucose into your muscles. It’s one of the simplest, fastest ways to lower blood sugar and improve sensitivity — even after a single meal.
Bonus: If you can’t walk right away, even light movement (like cleaning up or stretching) helps. Your muscles are natural glucose sponges.
Step 2: Time Your Carbs Smartly
Exercise temporarily opens the GLUT4 doors without needing insulin. That’s why carbs consumed around workouts behave differently than carbs eaten while sedentary.
Having a small serving of fruit or simple carbs before or during resistance training can help shuttle glucose directly into working muscles — not into fat storage. You’re effectively teaching your body to use carbs as fuel again.
Step 3: Slow Down the Fuel Pump
Your metabolism can only handle so much incoming energy at once. When the “fuel pump” runs too fast — from overeating or combining too many energy sources (fats + sugars) — overflow occurs.
To prevent that, add fiber and protein to every meal.
Soluble fibers like psyllium husk, acacia fiber, flaxseed, or chia slow digestion and help stabilize blood sugar by turning your food into a slow, steady release of fuel instead of a flood.
This isn’t just about digestion — it’s metabolic regulation.
Step 4: Burn the Sludge with Targeted Support
Once DAGs are formed, your body needs help breaking them down. Exercise is the best detox — it signals your mitochondria to burn fat for energy — but certain nutrients enhance that process.
Trimethylglycine (TMG) supports liver function and boosts AMPK, helping your cells clean out those fatty metabolites. Paired with regular activity, it helps your body rewire itself for efficient fat metabolism.
Step 5: Spice Up Your Metabolism with Cinnamon
Cinnamon isn’t just a flavor — it’s a natural insulin sensitizer. Certain compounds in cinnamon mimic insulin’s action and help receptors respond better to the real thing.
A simple ¼ teaspoon per day (added to coffee, oatmeal, or smoothies) can significantly improve your insulin response over time. It’s a small, delicious metabolic upgrade.
Step 6: Hit the Master Reset — Fasting
When your system is overloaded, sometimes you need to unplug it. Fasting gives your body a break from constant fuel input and triggers powerful repair mechanisms.
Even a 16-hour fast (intermittent fasting) can:
-
Lower insulin levels dramatically
-
Activate AMPK, the “fat-burning” enzyme
-
Boost autophagy — your body’s cellular cleanup process
-
Help clear out old, damaged proteins and DAGs
Think of fasting as pressing the reset button on your metabolism. It restores metabolic flexibility — your body’s ability to switch between burning sugar and burning fat efficiently.
Bonus: The Protective Power of Carnosine
Carnosine acts like a shield for your cells. It intercepts sugar molecules before they can latch onto and damage proteins — effectively blocking the glycation process.
Adding 3–6 grams per day, especially if you consume more carbs, can reduce oxidative stress, protect your arteries, and slow the visible signs of aging.
Recap: Reclaim Your Metabolic Power
Insulin resistance doesn’t have to be a life sentence. You can restore your metabolic health — often within days — by sending the right signals to your body.
-
Move after meals to bypass insulin.
-
Add fiber and protein to slow energy release.
-
Use cinnamon and TMG to enhance sensitivity.
-
Implement fasting to reset your system.
-
Protect your cells with carnosine.
Remember, your body isn’t broken. It’s just overloaded and confused by the modern diet and lifestyle. Once you give it clarity — fewer mixed signals, cleaner fuel, and proper rest — it responds quickly.
This isn’t about deprivation; it’s about retraining your metabolism to do what it was designed to do: burn energy efficiently and keep you vibrant, lean, and focused.
Your insulin resistance doesn’t need years of struggle to end — it just needs a few consistent days of sending the right signals.
News in the same category


The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup

Forget Calcium — Doctors Say This Is the #1 Exercise for the Strongest Bones

7 Warning Signs of Diverticulitis Most Doctors Miss
![Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]](https://onplusnewscom.8cache.com/onplusnewscom/images/2025/10/25/1761400387Ii4TCVIhQj.webp)
Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]
Medicinal Health Benefits of Turmeric, Curcumin and Turmeric Tea Based on Science

The Best Foods to Cleanse and Prevent Clogged Arteries

Capsaicin Stops Heart Attacks And Destroys Cancer Cells
17 Signs Your Body Is Too Acidic And 9 Ways To Quickly Alkalize It
Adrenal fatigue: what it is and 17 all-natural ways to fix it fast

Colon Cleansing With Kefir and Flaxseed Meal
Apple extract kills colon cancer cells better than chemotherapy drug
12 surprising foods that help dissolve blood clots naturally
News Post

7 Common Health Issues That Keep Appearing Could Be Early Warning Signs of Cancer

Small Life Hacks That Can Be Life-Saving
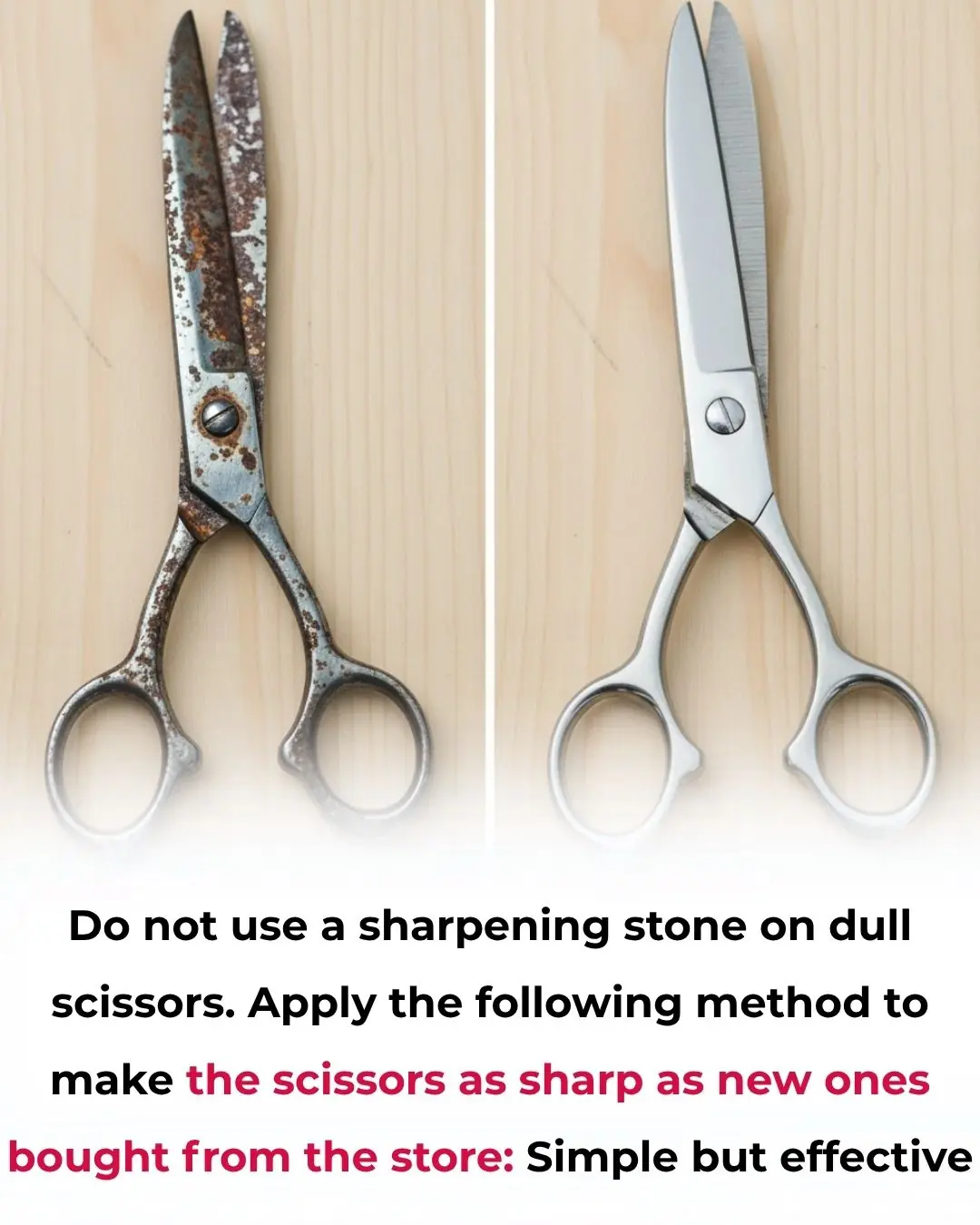
How to Sharpen Dull Scissors Without a Sharpening Stone: Simple and Effective Method

The Best Scientifically Proven Foods to Cleanse Your Liver
Flush the toxins silently damaging your kidneys — with these 13 powerful cleansing foods

The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

When Staying Alone in a Hotel: Place Two Cups on the Door Handle – A Small Action with Big Benefits

15 Things You Should Never Do to Protect Yourself from Lightning During Thunderstorms

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup
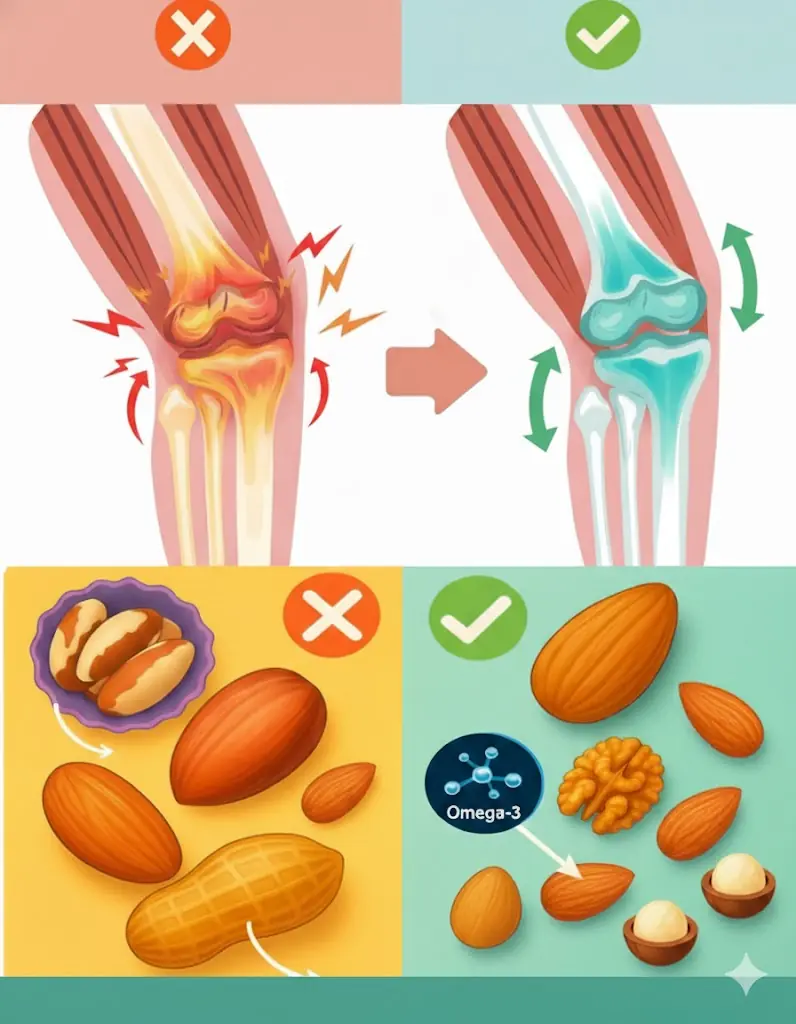
The Ultimate Nut Guide for Seniors: 4 Healthy Choices and 4 to Skip

The Man Who Walks for Dogs: Edgardo Perros’ 8,500-Mile Mission of Compassion

The Dog Who Went Out and Never Came Back the Same
To cook any kind of fish, just add a handful of these leaves: the fish will lose all its fishy smell and the meat will be rich and firm.

Great tips when growing pothos, in just 3 months the plant will form a beautiful green carpet
