Everything You Need To Know About Nail Pitting
Nail pitting refers to the appearance of small dents, depressions, or dimples on the surface of the nail plate. These indentations develop in the nail bed and are most commonly associated with autoimmune and inflammatory conditions, particularly psoriatic arthritis (PsA).
Treatment for nail pitting largely depends on identifying and managing the underlying condition. While it is not always possible to prevent nail changes entirely, controlling disease flares may significantly reduce their severity and progression.
Common Causes of Nail Pitting
The nail plate is produced in a specialized layer of tissue called the nail matrix. Inside the matrix are keratinocytes, which undergo a process known as keratinization. During this process, the cells flatten and harden to form the smooth, protective nail surface.
The matrix continuously produces new keratin that accumulates on the nail plate, pushing it forward and allowing the nail to grow. When inflammation, trauma, or immune dysfunction interferes with this process, abnormal keratin formation occurs, leading to visible pits or grooves in the nail.
Nail pitting is often a visible sign of an underlying medical condition, with some causes being more common than others.
Psoriasis
Psoriasis is a chronic autoimmune disease that causes rapid turnover of skin cells, leading to thickened, scaly patches on the skin.
In nail psoriasis, the immune system attacks cells in the nail matrix, disrupting normal keratin production. As a result, immature keratinocytes form and fail to function properly. When the nail grows with these damaged cells, pits and surface irregularities develop.
Nail pitting is particularly common in people with psoriatic arthritis, a condition that affects both the skin and joints. Studies suggest that a significant proportion of individuals with psoriasis will eventually develop nail involvement during their lifetime.
Alopecia Areata
Alopecia areata is an autoimmune disorder in which the immune system targets hair follicles, leading to patchy hair loss, most commonly on the scalp and face.
Although hair follicles are the primary target, the immune response may also affect the nail matrix. This can result in nail pitting, thinning, ridging, or brittleness. Nail involvement may signal more extensive immune activity and should be evaluated by a healthcare professional.
Dyshidrotic Eczema
Dyshidrotic eczema is characterized by small, itchy blisters that appear on the palms of the hands and soles of the feet. Triggers may include emotional stress, exposure to certain soaps or shampoos, and contact with irritating chemicals.
When dyshidrotic eczema becomes chronic or recurrent, persistent inflammation can extend to the nail matrix. Over time, this may interfere with nail formation and result in pitting, ridging, or discoloration of the nails.
Reactive Arthritis
Reactive arthritis is an autoimmune condition that typically develops days or weeks after an infection of the gastrointestinal or genitourinary tract.
Bacterial antigens in the bloodstream provoke an abnormal immune response, leading immune cells to attack joint tissues. In addition to joint pain and swelling, symptoms may occur outside the joints, including changes to the eyes, skin, and nails. Nail pitting in reactive arthritis reflects immune-mediated damage to the nail matrix.
Sarcoidosis
Sarcoidosis is an inflammatory disease in which clusters of immune cells called granulomas form in various organs, most commonly the lungs and lymph nodes.
Nail involvement in sarcoidosis is uncommon. When it does occur, it usually indicates systemic disease affecting multiple organs. Nail abnormalities may include pitting, ridging, or thickening and often accompany other serious clinical signs.
How to Recognize Nail Pitting
Nail pitting appears as small, round depressions or linear grooves that sink into the nail surface. It can affect both fingernails and toenails.
In nail psoriasis, pitting often shows the following features:
• Uniform size and depth
• One or multiple pits per nail
• Small pits with sharply defined edges
• Occasional red or discolored spots
Some individuals may also experience onycholysis, a condition in which the nail plate separates partially or completely from the nail bed. The presence of ten or more pits in a single nail, or more than fifty pits across all nails, is highly suggestive of psoriasis.
Important note: The appearance of nail pitting varies depending on the underlying cause. Additional symptoms may include nail brittleness, cracking, rough texture, discoloration, and abnormal thickening.
Getting a Diagnosis
Nail pitting is usually diagnosed through a physical examination of the nail beds by a healthcare provider. A detailed review of symptoms, medical history, and family history helps determine the most likely cause.
Because multiple conditions can produce similar nail changes, additional testing may be necessary, including:
• Blood tests to detect inflammation and genetic risk factors
• Imaging studies to identify lung inflammation or scarring if sarcoidosis is suspected
• Nail biopsy to examine the nail matrix at the cellular level
• Nail clippings analyzed under a microscope to distinguish psoriasis from fungal nail infections
Accurate diagnosis is essential, as treatment varies significantly depending on the underlying disease.
What Treatment Looks Like
Treatment aims to improve nail appearance, reduce pain, and slow further nail damage.
Note: Nail growth is slow, typically requiring several months for visible improvement. In many cases, patients must try more than one treatment before achieving satisfactory results.
Topical Medications
Medications applied directly to the nail or surrounding skin may reduce inflammation and improve nail texture. Corticosteroids are commonly prescribed.
Vitamin D–based treatments such as calcipotriol can reduce abnormal keratin buildup beneath the nail. Vitamin A derivatives such as tazarotene may help correct nail pitting and surface irregularities when used consistently.
Intralesional Steroid Injections
Steroid injections can be administered directly into or near affected nail areas. These are typically given every four to six weeks and are used for moderate to severe nail disease that does not respond to topical therapy.
Systemic Medications
In severe or widespread cases, systemic therapies may be required. These include biologic drugs and disease-modifying antirheumatic drugs (DMARDs) such as methotrexate. These medications suppress abnormal immune activity and can improve both skin and nail symptoms.
Tips for Preventing Nail Pitting
Although it is not always possible to prevent the conditions that cause nail pitting, certain habits may reduce flare-ups and minimize nail damage:
• Avoid artificial nails and harsh nail treatments
• Use mild nail polish and gentle buffing only
• Do not push back cuticles or scrape beneath the nails
• Keep hands moisturized and nails trimmed short
• Wear protective gloves when working with chemicals or performing manual tasks
Maintaining good nail hygiene can reduce trauma to the nail matrix and lower the risk of worsening symptoms.
Complications to Watch For
Beyond cosmetic concerns, nail pitting can negatively affect quality of life. Progressive nail changes may cause pain and interfere with daily activities such as grasping objects, buttoning clothing, or typing.
In some cases, nail disease reflects more severe systemic inflammation, signaling the need for closer medical monitoring and long-term management.
Disclaimer: This article is for educational purposes only and is not intended as medical advice. Always consult a qualified healthcare provider for diagnosis and appropriate treatment of nail disorders.
News in the same category

Right-Side Abdominal Pain in Women: Could It Be Gallstones?
🧠 8 Strange (But Real) Signs Your Body Is Begging for More Vitamin B12 – Don’t Ignore These Red Flags

Discovering Smart Protein Choices: 4 to Include and 5 to Limit for Kidney Health Support

How I Improved the Appearance of My Legs: Smoother, Brighter & Healthier-Looking Skin with Simple Habits

Discover 5 Everyday Foods That May Increase Cancer Risk and Simple Swaps for Better Health

Discover Everyday Herbal Habits That Can Help Support Your Kidney Health Naturally

Danger at home! 8 household items that could harm your health lp

Discover a Simple Homemade Recipe with Lemon, Ginger, and Honey to Naturally Support Your Eye Health

Doctors Reveal That Eating Broccoli Regularly Leads To pu
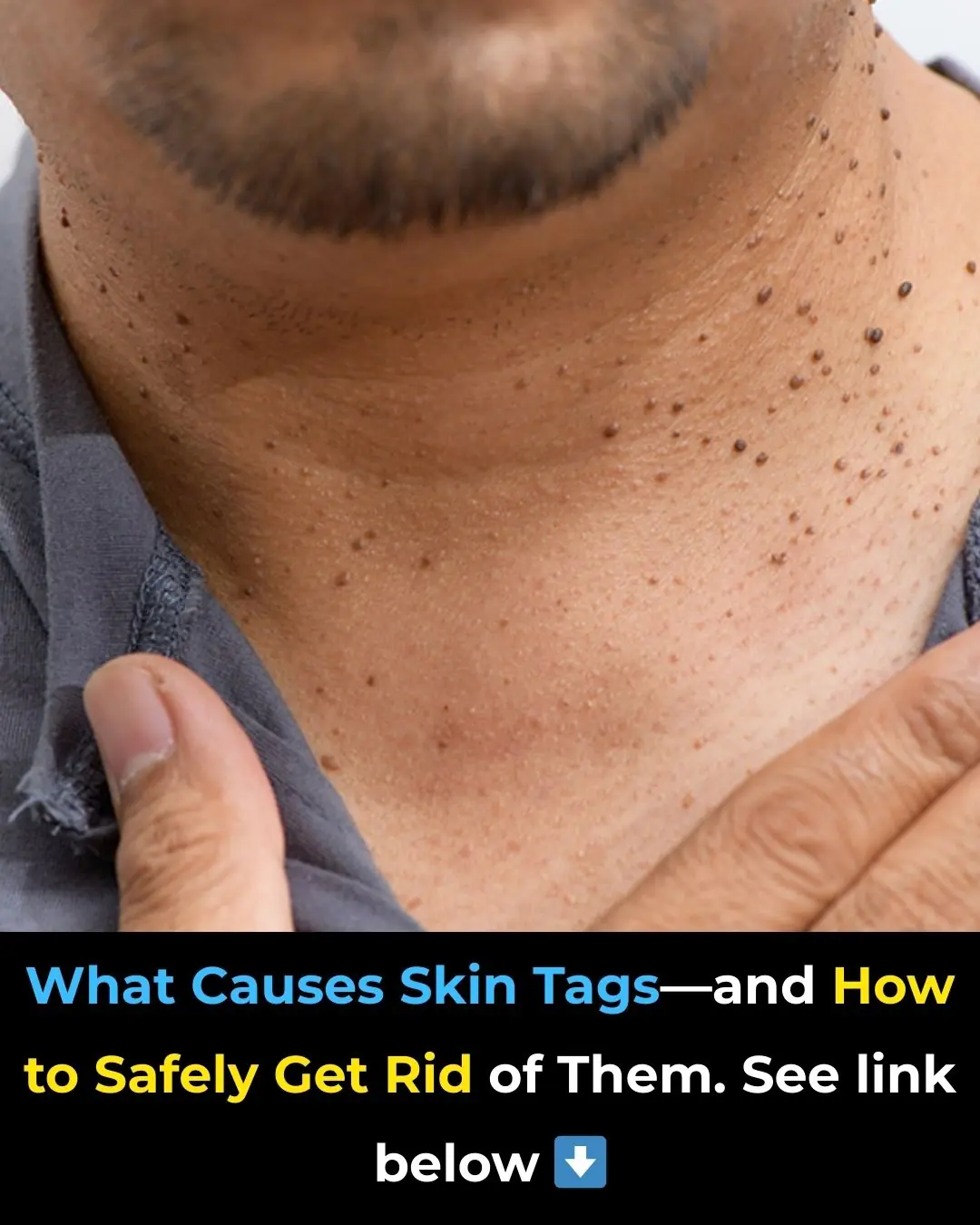
How To Identify Skin Tags and When To Remove Them

14 Visible Signs of Cancer Most Women Ignore
When You Sleep Less Than Six Hours a Night

What Eating Oranges Can Really Do to Your Body
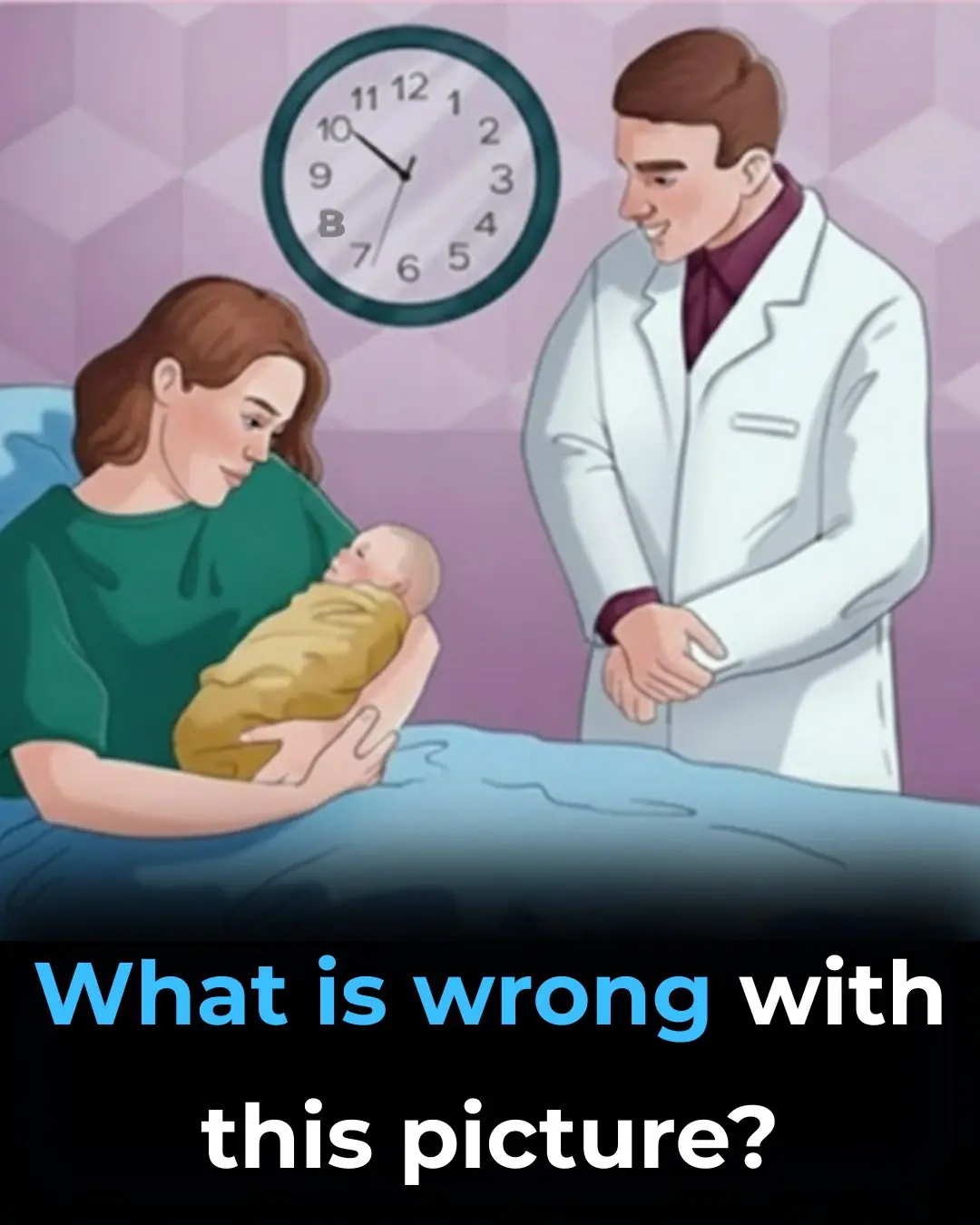
Can You Spot the Hidden Mistake in This Hospital Picture

Sida Acuta: Exploring the Healing Properties of this Herbal Remedy

Do you wake up several times a night to go to the bathroom? Discover the 5 mistakes that are ruining your sleep

Discover the Plant That Can Purify Your Blood, Renew Your Skin, and Cleanse Your Organs — But Only If You Use It This Way

Garlic and Clove Oil: A Natural Approach Many Are Trying for Varicose Veins and Better Circulation
News Post
The Wisest Japanese Secret! Even at 70, You Look Like 35
Whiten Dingy Grout
8 Foods You Should Eat Instead of Taking a Vitamin C Supplement

Right-Side Abdominal Pain in Women: Could It Be Gallstones?
🧠 8 Strange (But Real) Signs Your Body Is Begging for More Vitamin B12 – Don’t Ignore These Red Flags

Discovering Smart Protein Choices: 4 to Include and 5 to Limit for Kidney Health Support

How I Improved the Appearance of My Legs: Smoother, Brighter & Healthier-Looking Skin with Simple Habits

Discover 5 Everyday Foods That May Increase Cancer Risk and Simple Swaps for Better Health

Discover Everyday Herbal Habits That Can Help Support Your Kidney Health Naturally

A fire swallowed my entire farm in a single night, leaving nothing but ashes and smoke behind

Danger at home! 8 household items that could harm your health lp

Discover a Simple Homemade Recipe with Lemon, Ginger, and Honey to Naturally Support Your Eye Health

Doctors Reveal That Eating Broccoli Regularly Leads To pu

They Invited the ‘Class Loser’ to the 10-Year Reunion to Mock Her — She Arrived by Helicopter
How To Identify Skin Tags and When To Remove Them

14 Visible Signs of Cancer Most Women Ignore
When You Sleep Less Than Six Hours a Night

What Eating Oranges Can Really Do to Your Body