No Reset: When a Clinical Mindset Takes Over Your Whole Life
Physicians are trained to expect the worst. From the earliest days of medical education, they learn to scan for danger, anticipate complications, and prepare for every possible negative outcome. In clinical settings, this mindset saves lives. Outside the hospital or clinic, however, it can quietly become a burden—one that follows physicians home and begins to shape how they experience the rest of their lives.
The Skill That Never Turns Off
Medicine rewards vigilance. A missed diagnosis, an overlooked symptom, or a delayed intervention can carry serious consequences. As a result, physicians develop a habit of constant mental scanning: What could go wrong? What am I missing?
Over time, this pattern becomes automatic. The same mental process used to evaluate a patient with chest pain may be applied to everyday situations—children running late, a partner’s headache, a strange noise in the car, or a minor personal health symptom. The mind remains in diagnostic mode, even when no diagnosis is needed.
When Preparedness Turns Into Anxiety
What begins as professional competence can slowly evolve into chronic anxiety. The physician’s brain, trained to prioritize rare but catastrophic outcomes, may struggle to accept uncertainty or benign explanations. Everyday life becomes filled with low-level alarm.
Many physicians describe:
-
Difficulty relaxing or being fully present at home
-
Persistent “what if” thinking
-
Trouble sleeping due to racing thoughts
-
Emotional exhaustion without a clear cause
This constant anticipatory stress can erode emotional well-being, even in doctors who love their work and feel fulfilled professionally.
The Emotional Cost of Hypervigilance
Hypervigilance does not come without consequences. Sustained activation of stress responses can contribute to burnout, depression, and feelings of detachment. Relationships may suffer as physicians unintentionally bring clinical detachment or worst-case thinking into family interactions.
Loved ones may sense emotional distance or a tendency to catastrophize. Meanwhile, physicians often feel guilty for struggling—after all, they are trained to manage stress and help others cope with illness and uncertainty.
Why Physicians Rarely Talk About It
The culture of medicine often normalizes self-sacrifice and emotional suppression. Many physicians assume that this way of thinking is simply “part of the job.” Others fear that acknowledging mental strain may be interpreted as weakness or incompetence.
As a result, the psychological toll of carrying a clinical mindset into personal life often goes unspoken, quietly accumulating over years of practice.
Learning to Create a Mental Boundary
The solution is not to abandon clinical thinking, but to contain it. Some physicians find relief by intentionally creating mental transitions between work and home—simple rituals that signal the brain that vigilance is no longer required.
Helpful strategies may include:
-
Reflective writing to “offload” clinical thoughts
-
Mindfulness practices that emphasize presence rather than prediction
-
Therapy or peer support to normalize these experiences
-
Consciously allowing uncertainty in non-clinical situations
These practices help retrain the nervous system to recognize when alertness is necessary—and when it is not.
Reclaiming Life Beyond the Diagnosis
Physicians dedicate their careers to protecting others from harm. Yet they, too, deserve a life not dominated by constant anticipation of disaster. Learning to step out of the clinical mindset—at least part of the time—is not a failure of professionalism. It is an act of self-preservation.
Medicine may teach physicians how to save lives. But learning when to turn off the internal alarm may be what allows them to truly live their own.
News in the same category
Frozen Meat Rock-Hard from the Freezer? Use These Two Simple Methods to Thaw It Quickly Without Waiting

5 Types of Eggs That Can Be Harmful If Consumed Too Often

Women Who Drink Perilla Leaf Water With Lemon at These 3 Times May Notice Brighter Skin and a Slimmer Waist
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)
How to Naturally Increase Estrogen Levels

Evidence-Based Health Benefits of Honey (Raw, Pure, Natural) + Turmeric Golden Honey Recipe
Foamy Urine: Here’s Why You Have Bubbles in Your Urine
Why Almonds Are So Good for You: Health Benefits of Almonds Backed by Science

Dermatology Data Reinforce the Relative Safety of JAK Inhibitors
Can Cuffless Blood Pressure Devices Transform Cardiovascular Disease Prevention and Treatment?
Early-stage stomach cancer is often accompanied by these 6 symptoms

6 Things People Who Live to 100 Do Every Week to Stay Healthy

Seven Foods That Rarely Spoil: Still Safe to Eat Even After the Expiration Date

Five Parts of Fish That Are Dirty and Potentially Toxic — The First One Is Often Mistaken as Healthy but Can Be Fatal

Health Benefits of Boiled Green Bananas

How to Drink Lemon Turmeric Water in the Morning to Support Liver and Kidney Detox Without Harming the Stomach

Can Relative Fat Mass Replace BMI in Assessing Obesity?
When Women Target Other Women: The Hidden Wounds of Bullying in Medicine
News Post

Jeezy Calls Out Industry for Exploiting Trauma in Young Rappers
Marlon Wayans warns 50 Cent

Bun B Expands Trill Burgers with New Missouri City Location

Octavia Spencer celebrates 'iconic' Sinners' duo Ryan Coogler and Michael B. Jordan for EW's 2025 Entertainers of the Year
Lil Durk's Legal Team Alleges He's Spent 131 Days in Solitary Confinement Over Apple Watch
DMX Will Posthumously Become Ordained Minister at Historic Underground Railroad Church
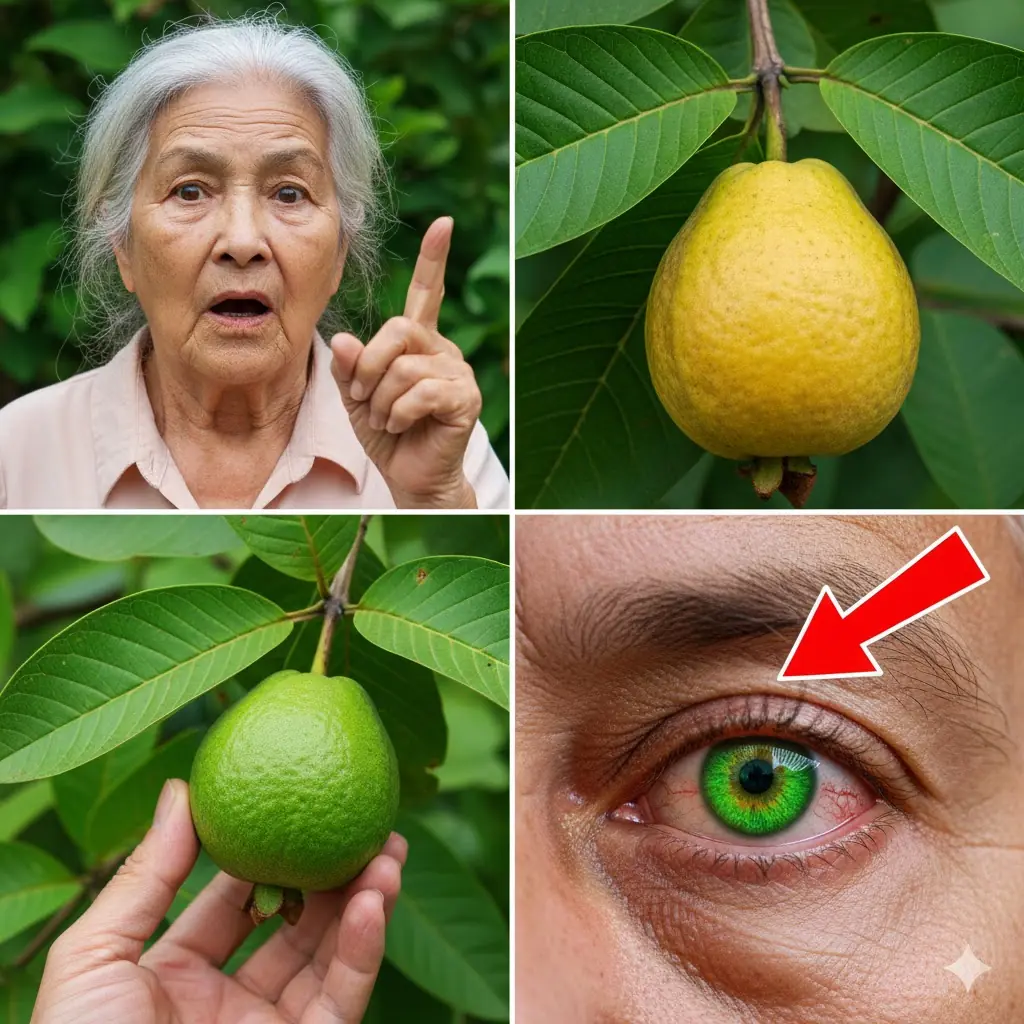
How Guava Can Naturally Support Your Eye Health: Surprising Benefits and Safe Remedies

Grape Hyacinth (Muscari): A Tiny Spring Wonder with Surprising Benefits and Uses

12 Surprising Benefits of Bull Thistle Root (And Safe Ways to Use It Naturally)
14 Little-Known Health Benefits of Moringa Leaves

Tips for preserving bean sprouts to keep them crispy and prevent them from turning black for 7 days.
Simple Tips to Store Ginger Without a Refrigerator: Keep It Fresh for a Year Without Sprouting or Spoiling
Frozen Meat Rock-Hard from the Freezer? Use These Two Simple Methods to Thaw It Quickly Without Waiting

5 Types of Eggs That Can Be Harmful If Consumed Too Often

Women Who Drink Perilla Leaf Water With Lemon at These 3 Times May Notice Brighter Skin and a Slimmer Waist

Tata Sierra vs Mahindra XUV 7XO: A Mid‑Size SUV Showdown 🚙🔥

This red, scaly patch won’t go away. It's all over my forehead and doctor isn't answering me. What is it?
I keep wondering why this happens to me
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)