Scientists Found IV Bags Could Send Microplastics Directly Into Your Bloodstream During Infusions
Invisible Plastics in IV Bags: What’s Really Flowing Into Patients’ Veins
Hospital patients trust intravenous infusions to deliver lifesaving fluids and medications. Doctors depend on IV bags to rehydrate the dehydrated, nourish the malnourished, and deliver drugs that can mean the difference between life and death. Every year, millions of people around the world receive IV treatments without a second thought—trusting that what flows through those clear tubes is clean, sterile, and safe.
But a startling discovery has challenged that trust. Scientists have now found that standard hospital IV saline bags contain thousands of microscopic plastic particles—tiny fragments invisible to the naked eye, suspended in the clear fluids that doctors inject directly into patients’ bloodstreams.
These aren’t contaminants introduced during handling or shipping. They’re not random dust or industrial pollution. The microplastics come from the IV bags themselves—tiny shards shed from the very plastic meant to hold lifesaving fluids.
Each 250-milliliter bag carries an estimated 7,500 polypropylene microplastics. These particles, ranging from 1 to 62 micrometers, are so small that they can travel freely through the bloodstream. They move from veins to arteries, to the heart, and onward to organs like the liver, lungs, and kidneys. Once inside, they may accumulate or trigger inflammation.
For years, scientists have warned about the dangers of microplastics in the environment—through food, water, and even the air we breathe. Yet until recently, almost no one had considered the possibility that these plastics could be pumped directly into human veins in the course of medical treatment.
What Researchers Found Inside Standard Hospital IV Bags

This revelation comes from a 2025 study by Liwu Zhang and Ventsislav Kolev Valev, published in Environment & Health. The researchers analyzed two widely used commercial brands of hospital saline solution to see whether the packaging itself could be releasing microplastics into the liquid.
To mimic real clinical conditions, the team transferred saline from IV bags into glass containers at typical hospital infusion rates—40 to 60 drops per minute. Afterward, they filtered the fluid through ultra-fine membranes and used advanced microscopy and spectroscopy techniques to identify and count plastic fragments.
The results were consistent across both brands. Every sample contained polypropylene particles, the same material used to manufacture the IV bags. On average, each liter of saline solution contained about 7,500 microplastic particles—and those particles varied in size, shape, and structure.
In Brand 1, about 52% of particles measured 1–10 micrometers, 35% were 10–20 micrometers, and 7% ranged from 20–30 micrometers. Brand 2 showed a similar trend, with nearly 68% smaller than 10 micrometers. Most particles fell within the size range that allows them to move easily through blood vessels and become lodged in tissues.
These findings highlight a sobering truth: the smaller the particle, the deeper it can travel into the body. Microplastics injected directly into the bloodstream bypass all natural filters—lungs, liver, kidneys—that normally trap or eliminate contaminants entering through food or air.
Polypropylene Shedding: How Plastic Bags Contaminate Their Own Contents
Polypropylene is used in IV bags because it’s transparent, lightweight, and chemically stable. It resists cracking and interacts safely with most medical solutions—or so it was thought. Hospitals worldwide rely on it precisely for these qualities.
But like all plastics, polypropylene degrades over time. Exposure to ultraviolet light can trigger photo-oxidation, making the material brittle. Fluctuations in temperature affect its flexibility and cause microscopic fractures. When the temperature rises from 23°C to 40°C, for instance, polypropylene loses about 20% of its stiffness.
During manufacturing, transport, and storage, physical stress further weakens the material. Each flex, bump, or vibration can release tiny fragments into the fluid. Even the saline itself—slightly ionic and reactive—can accelerate molecular degradation, encouraging small particles to detach and disperse.
The microplastics identified in the study perfectly matched the composition of the bags themselves. That means the contamination doesn’t come from the environment—it’s self-generated. The container sheds its own material into the sterile fluid long before it reaches a patient’s bloodstream.
Measuring the Invisible: How Scientists Detected Microscopic Particles

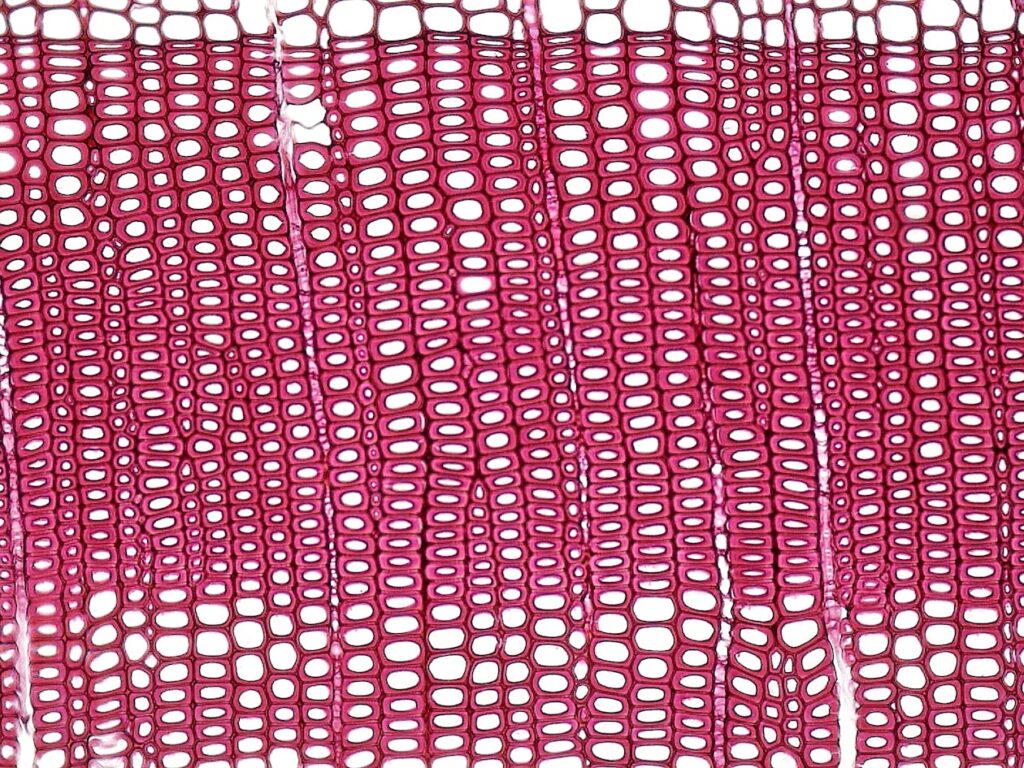
Finding something so small requires extraordinary precision. To detect and confirm the presence of microplastics, the researchers used Surface-Enhanced Raman Spectroscopy (SERS)—a method that amplifies molecular vibrations so scientists can identify materials based on their unique light signatures.
The team created custom gold-coated silicon substrates with microscopic pyramid structures that enhance Raman signals by focusing light into narrow electromagnetic “hot spots.” This allowed them to detect even the faintest traces of plastic.
After filtering the IV solutions, scientists concentrated the remaining particles and placed them onto these SERS surfaces. Using scanning electron microscopy (SEM) combined with energy-dispersive spectroscopy (EDS), they examined the shape, size, and chemical composition of each fragment. The carbon signatures perfectly matched polypropylene’s known profile.
To ensure accuracy, the team maintained an ultra-clean environment: they wore plastic-free fiber coats and latex gloves, used glassware washed multiple times with ultrapure water, and covered all containers to prevent airborne contamination. Blank control tests confirmed the results were genuine and not artifacts of the laboratory.
Size Matters: Particles Small Enough to Travel Anywhere in the Body
Microplastic particles between 1 and 62 micrometers can reach virtually any part of the human body. Blood carries them through arteries and veins, and depending on their size, they may lodge in capillaries, accumulate in organs, or pass into surrounding tissues.
Pulmonary capillaries—the smallest blood vessels in the lungs—range from 2 to 15 micrometers wide. In this study, the average particle size was 9.2 micrometers for one brand and 7.7 micrometers for the other—almost perfectly sized to become trapped in lung tissue.
About 60% of the particles found measured between 1 and 10 micrometers, meaning they can pass through tiny vessels and reach organs such as the liver, spleen, or even the brain. The smallest particles may cross biological barriers that normally protect these organs from foreign substances.
Electron microscopy showed a variety of shapes: threadlike filaments about 15 micrometers long, blocky fragments, and irregular granules roughly 5 micrometers in diameter. These shapes interact differently with blood vessels and tissue surfaces, potentially influencing how they move and where they accumulate.
From One Bag to Thousands of Particles: Calculating Exposure During Treatment

To understand the scale of exposure, researchers calculated how many microplastics a patient might receive under typical medical conditions.
-
Severe dehydration: Treatment often requires 4–5.5 liters of fluid, translating to roughly 30,000–40,000 particles entering the bloodstream.
-
Routine hospital hydration: Patients may receive 13–16 bottles of saline daily, equaling 24,000–30,000 microplastics per day.
-
Abdominal surgery: A patient might receive about 7 liters of fluid on the day of surgery—equivalent to over 50,000 particles in one procedure.
-
Labor and delivery: Mothers receive around 240 milliliters per hour for about 4 hours, resulting in 7,000–8,000 particles.
-
Emergency care: A half-liter rapid infusion in 15 minutes could inject nearly 4,000 microplastics, while larger resuscitation doses double that amount.
These numbers reveal a disturbing reality: modern medicine may be unintentionally introducing billions of plastic particles into patients every year—not through pollution or lifestyle, but through routine hospital care.
Where These Particles End Up Once Inside Your Blood
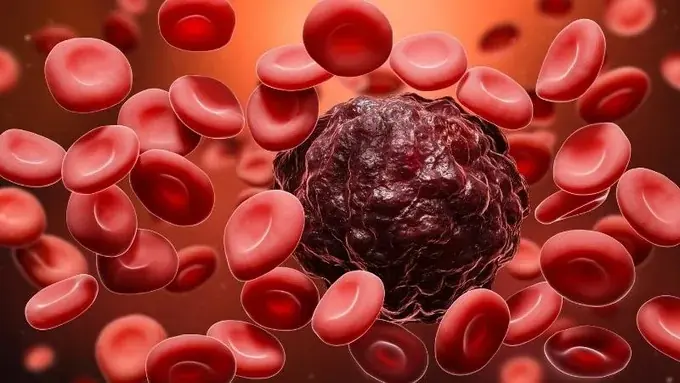
Once injected, microplastics don’t vanish. Studies have confirmed their presence in multiple human organs and tissues.
One investigation of 304 people found polyethylene in plaque removed from carotid arteries—detected in nearly 60% of patients. Those with polymer traces faced over four times greater risk of fatal cardiovascular events during the following three years.
Another study examined human blood clots and found plastic fragments in 16 of 26 samples, most smaller than 10 micrometers. Animal research shows a similar pattern: when microplastics enter the bloodstream, smaller ones concentrate in the liver and spleen, while larger ones tend to accumulate in the lungs.
In human liver tissue, scientists have detected multiple polymer types—ranging from 3 to nearly 30 micrometers in size—in patients with cirrhosis, but not in healthy controls. Even more concerning, polypropylene particles can cross the placenta, meaning fetuses may be exposed during pregnancy.
Why Particle Size Matches Capillary Diameter Perfectly
The lungs appear particularly vulnerable. Pulmonary capillaries—averaging 2–15 micrometers—are almost exactly the size range of the microplastics detected in IV fluids. As blood flows from the heart into the lungs, these particles can get trapped, blocking small vessels and reducing oxygen exchange.
Doctors have already documented at least one case that may reflect this danger. A 26-year-old woman receiving total parenteral nutrition developed high fever and shortness of breath. Tests showed blood oxygen levels falling below 90%. A lung biopsy revealed widespread small-vessel thrombosis and inflammation caused by particulate matter between 0.5 and 650 micrometers. Once the IV nutrition was stopped, her symptoms disappeared—strong evidence that the infused particles were to blame.
Physical Damage: Inflammation, Blood Clots, and Organ Dysfunction

Microplastics can harm the body in several ways beyond physical blockage. They can trigger inflammatory responses, cell death, genetic damage, and fibrosis.
When the immune system recognizes these particles as foreign, white blood cells rush to attack them, releasing inflammatory chemicals that can injure surrounding tissue. Over time, chronic inflammation causes scarring, thickening, and loss of function in affected organs.
Microplastics can also activate blood-clotting pathways, forming dangerous thrombi that obstruct vessels. During heart surgery, researchers have linked particle contamination to post-operative organ dysfunction. In some cases, immune cells form granulomas—clusters of cells that wall off foreign material—further disrupting normal tissue structure.
Why Current Systems Can’t Stop These Particles
Hospital filtration systems are designed to block bacteria and other large contaminants, but they fail to stop microplastics. Even after passing through 0.2-micrometer filters, researchers still detected thousands of particles in the saline.
The reason lies in the irregular shape and flexibility of polypropylene. Many fragments can deform under pressure, squeezing through filter pores that should theoretically trap them. Moreover, current medical standards don’t test for plastic contamination—meaning hospitals have no established way to measure or prevent it.
As a result, IV therapy today remains an unintentional delivery route for microplastics, bypassing every natural defense the human body has.
Solutions on the Table: Better Filters and Smarter Storage

The good news is that the problem, while serious, may be solvable. Researchers propose several strategies to reduce microplastic contamination in IV fluids.
-
Protect IV bags from heat and UV light. Controlled storage conditions—cool, dark, and stable—can slow polypropylene degradation and reduce particle shedding.
-
Add finer, micrometer-level filters before infusion. Installing these filters at the point of use could trap particles after they leave the bag but before entering a patient’s bloodstream.
-
Develop alternative materials. Glass or advanced biopolymers could replace polypropylene, eliminating the source of plastic shedding. Though heavier and more expensive, such materials would offer long-term safety.
-
Improve manufacturing quality control. Tighter standards across production, transport, and hospital storage could ensure cleaner, more stable materials.
-
Design closed infusion systems. These systems minimize external contamination while reducing friction that causes microplastic release.
As the researchers wrote:
“Our findings highlight an aspect of plastic pollution that affects humans most directly—because microplastics are being injected into the bloodstream. Yet this pathway has received far less attention than any other.”
What This Discovery Means for Medical Safety
For decades, intravenous therapy has been one of medicine’s greatest life-saving tools. No one imagined that the very system designed to heal could also deliver a hidden pollutant into human veins.
Yet this discovery offers not only concern—but opportunity. Hospitals can begin protecting IV bags from light and heat immediately. Manufacturers can innovate safer materials and filtration systems. Regulators can set new contamination standards for medical plastics.
Unlike environmental pollution that spans oceans and continents, this problem exists within a controlled medical infrastructure—one that can change quickly if the will exists.
Identifying the presence of microplastics in IV solutions doesn’t diminish modern medicine’s achievements. Instead, it challenges the healthcare system to evolve once again—to recognize emerging risks and act before harm becomes widespread.
News in the same category
Choose a Nail to Discover What Kind of Woman You Are
Never Do These 15 Things for a Man (Even If You’re Madly in Love With Him)

Adam Sandler Sends Heartfelt Flowers to Jennifer Aniston EVERY Year On a Specific Day and Here’s Why
The Dawn of Genetic Healing: A New Hope for Huntington’s Disease

The Hidden Meanings Behind Men Wearing Earring

20 Subtle Signs He’s Not as Good as He Seems

Why Your Hard-Boiled Eggs Have That Weird Green Ring
Aluminum Foil Can Help You Boost Your Wi-Fi Signal

Halo Brows: The Playful, Loopy New Beauty Trend Taking Over
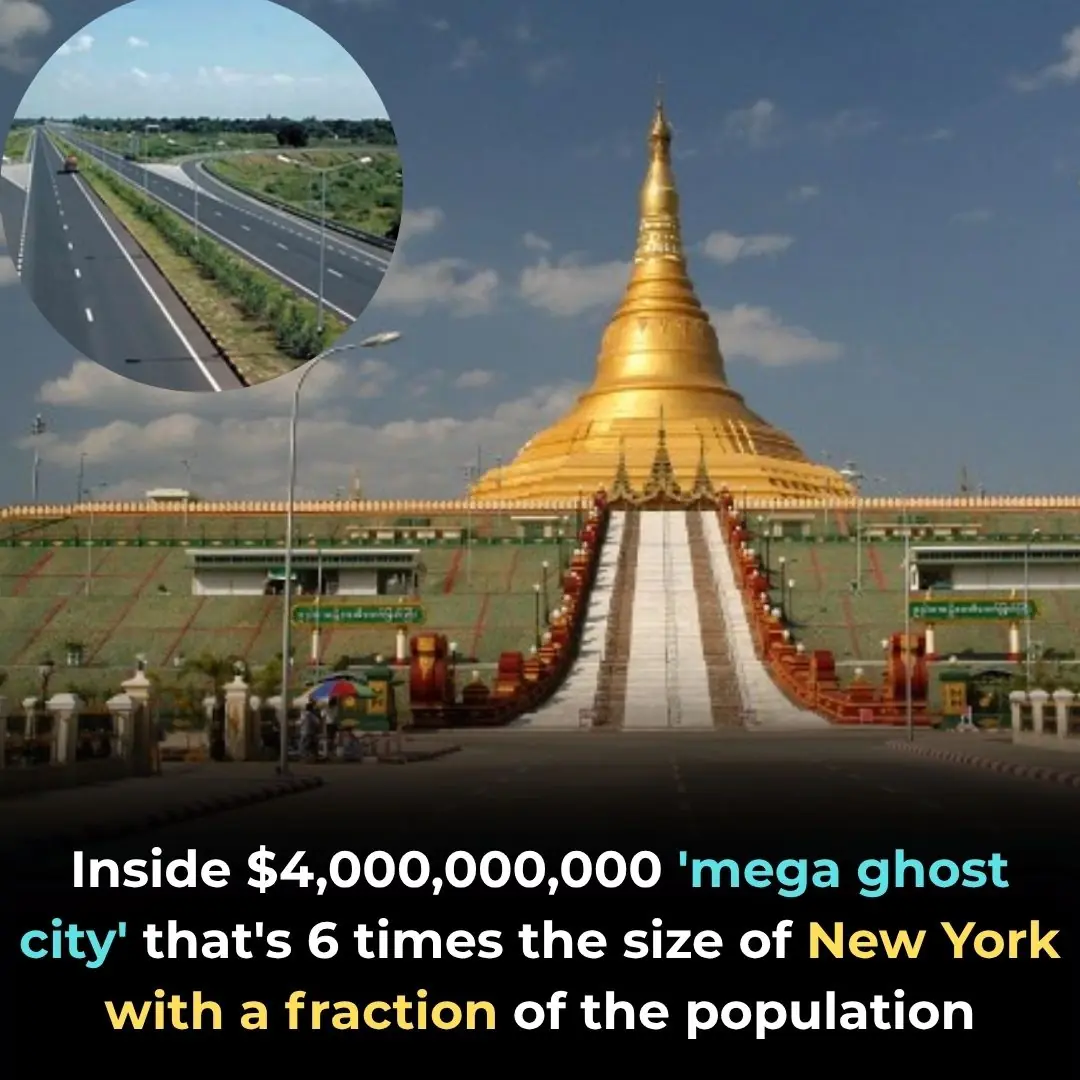
Inside $4,000,000,000 'mega ghost city' that's 6 times the size of New York with a fraction of the population

Why There's A Growing Trend Of Straight Men Dating Trans Women
What Really Happens When You Drink Coffee Every Morning

Joseph Gordon-Levitt Urges a Global Pause on AI Superintelligence Until Safety Measures Are in Place
The Three Nations Working Together to Protect the Mayan Jungle
The Spiritual Meaning of White Butterflies in Your Home

If You Find A Tick Inside Your Home, Here’s What You Need To Know

Magpie The Spiritual Meaning of an Unusual Encounter

When your dog looks at you for a long time, here's what it means according to experts...
News Post

Papaya Sap for Cracked Heels: A Simple Natural Remedy
Garlic for Ear Health: Natural Relief and Protection
Old Doctors’ Secret: Mix Olive Oil + Black Pepper to Fix 11 Problems After 60 — See Results in 1 Week

🌿 The Forgotten Healing Drink Making a Powerful Comeback
You’ll NEVER Shave the Same Again After Seeing This Onion Trick

HOW I GREW MY EYELASHES IN JUST 7 DAYS — Naturally with Castor Oil

7 Essential Leaves to Naturally Improve Your Eye Health

Don’t Drink Coconut Water Before You Know These 11 Secrets!

White Clover (Trifolium repens): 15 Benefits and Homemade Uses

7 Benefits and Uses of Ageratum conyzoides
How often should you shower
Expert, 95 Years Old with 60 Years of Cancer Research Reveals: You Must Avoid These 4 Things So Cancer Doesn’t Come Knocking

Sharp Pain in Ear: Causes, Treatments and When to See a Doctor
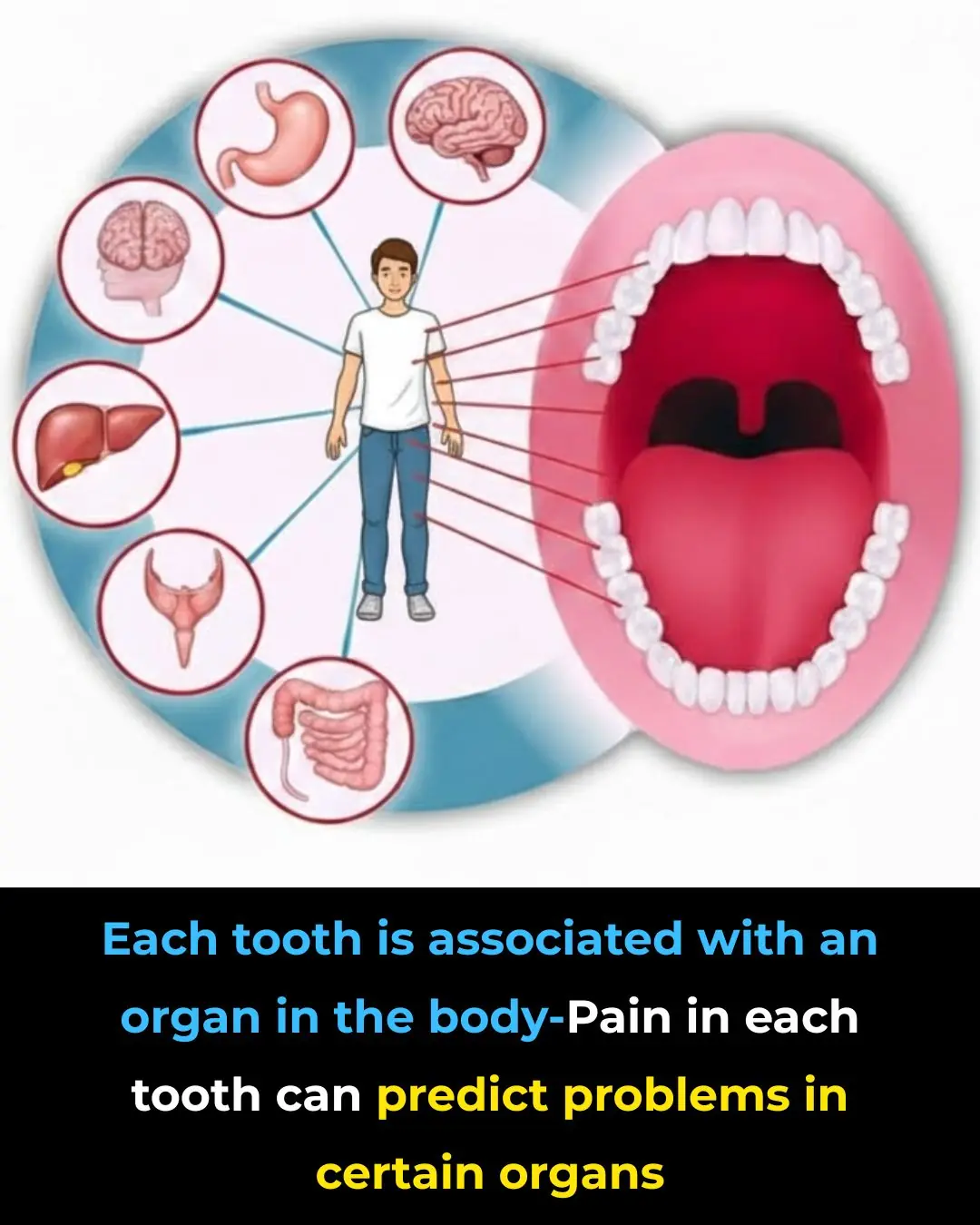
Each Tooth Is Associated With An Organ In The Body – Pain In Each Tooth Can Predict Problems In Certain Organs

Here’s the secret why everyone puts avocados on the fire!

Amazing vitamin can help stop cancer growth and this is how much you need

Euphorbia Hirta: 30 Benefits and How to Use It Safely
THE BEST HOME REMEDIES THAT END CONSTIPATION FAST AND NATURALLY

Lady places cup of vinegar into microwave. Here’s the genius reason why
