
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
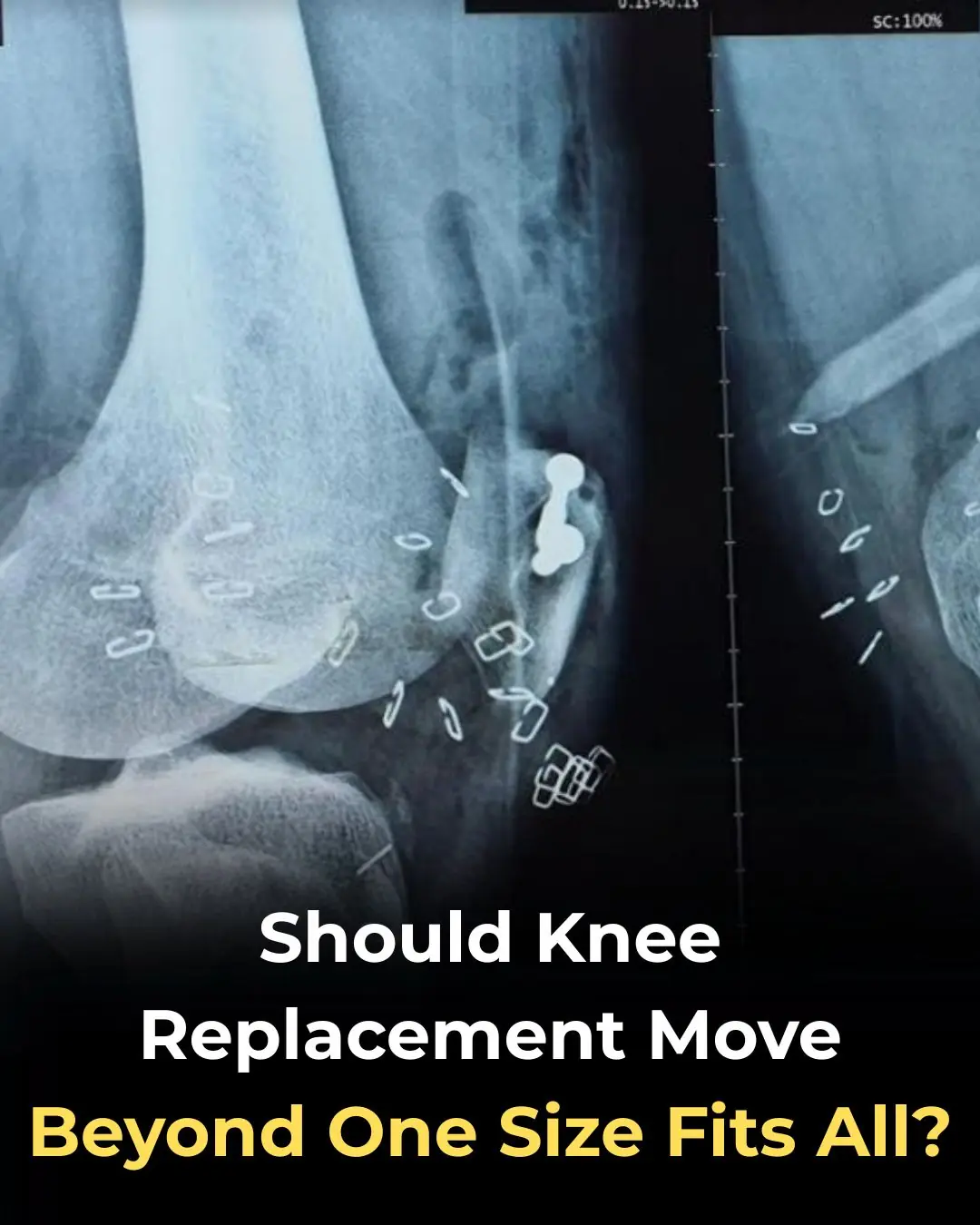
For decades, total knee replacement (TKR) surgery has been guided by a simple and seemingly logical principle: restore the leg to a perfectly straight, neutral mechanical alignment. This approach aimed to evenly distribute load across the artificial joint, reduce implant wear, and prolong prosthesis longevity. Standardized alignment became the gold standard taught in surgical training programs and embedded in implant design worldwide.
Yet despite remarkable advances in materials, implant technology, surgical navigation, and robotic assistance, a persistent and troubling reality remains: approximately 5%–20% of patients report ongoing discomfort, dissatisfaction, or a knee that never truly feels “forgotten” after surgery. This gap between technical success and patient satisfaction has prompted orthopedic surgeons to re-examine a long-standing assumption—is neutral alignment truly optimal for every patient?
The Forgotten Knee: A Measure of True Success
The concept of a “forgotten knee” refers to a joint replacement that feels so natural and pain-free that the patient is largely unaware of its presence during daily activities. While many patients experience significant pain relief and functional improvement after knee replacement, achieving a forgotten knee remains elusive for a substantial minority.
Importantly, dissatisfaction is not always linked to implant failure, infection, or obvious surgical complications. Instead, many patients describe vague but persistent symptoms: stiffness, unnatural movement, instability, or a sense that the knee “doesn’t belong” to their body. These experiences suggest that success in knee replacement may depend on more than implant durability and radiographic alignment alone.
The Problem With Universal Neutral Alignment
Neutral mechanical alignment assumes that a straight leg—where the hip, knee, and ankle fall into a single vertical line—is ideal for all individuals. However, growing evidence challenges this assumption. Large population studies have shown that many people naturally have a constitutional varus or valgus alignment, meaning their legs are slightly bowed inward or outward even before arthritis develops.
For these individuals, forcing the knee into perfect straightness during replacement surgery may unintentionally disrupt their native biomechanics. Muscles, ligaments, and soft tissues that have adapted over decades to a specific alignment are suddenly required to function in a new configuration. This mismatch can lead to altered joint kinematics, increased ligament tension, and abnormal loading patterns—factors that may contribute to residual pain or dissatisfaction.
Toward Personalized Alignment Strategies
In response, the field of knee arthroplasty is increasingly exploring personalized alignment approaches, such as kinematic alignment and functional alignment. Rather than imposing a universal standard, these strategies aim to restore the patient’s individual anatomy and pre-arthritic joint orientation as closely as possible.
Kinematic alignment, for example, seeks to position the implant in a way that replicates the knee’s natural motion and alignment, respecting the patient’s unique bone geometry and ligament balance. Early studies suggest that this approach may improve functional outcomes, patient satisfaction, and the likelihood of achieving a forgotten knee—without compromising implant survival in the short to mid term.
Technology Enabling Individualization
Advances in surgical technology are making personalization more feasible than ever. Robotic-assisted surgery, patient-specific instrumentation, and advanced imaging allow surgeons to plan and execute procedures with remarkable precision. These tools support nuanced alignment decisions tailored to each patient’s anatomy, lifestyle, and functional goals.
However, personalization also requires careful judgment. Not every patient is an ideal candidate for non-neutral alignment, and long-term data are still evolving. The challenge lies in balancing respect for individual anatomy with the proven principles of implant longevity and joint stability.
Rethinking Success in Knee Replacement
The ongoing debate over alignment reflects a broader shift in medicine—from standardized treatment protocols toward patient-centered care. Knee replacement surgery is no longer judged solely by X-rays and implant survival curves, but by how patients feel, move, and live with their new joint.
As evidence continues to accumulate, it is becoming increasingly clear that one-size-fits-all alignment may not serve every patient equally well. Embracing anatomical diversity and functional individuality may be the next crucial step in improving outcomes and closing the satisfaction gap in knee replacement surgery.
Conclusion
Total knee replacement has transformed millions of lives, yet the persistent absence of a forgotten knee in a notable percentage of patients highlights the limitations of a purely standardized approach. Recognizing that most people are not naturally “neutral” challenges decades of surgical convention—but it also opens the door to more personalized, biomechanically harmonious solutions.
Moving beyond one-size-fits-all alignment does not mean abandoning proven principles; rather, it means refining them. By integrating anatomical individuality, advanced technology, and patient-centered outcomes, knee replacement surgery may move closer to its ultimate goal: a joint that patients no longer have to think about at all.
News in the same category

Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail
How do people who take naps and those who don't? Experts reveal surprising truth
Of particular note, these four unusual pains occurring every morning may be a warning sign of a tumor in the body
10 Habits That Harm Your Heart That You Probably Didn’t Know About

How to Get Rid of Muscle Soreness: Home Remedies That Really Work

Crusty sore on my lip won’t go away. Appointment is impossible to get right now. What is this?

Coffee Consumption, Additives, and Mortality Risk: Evidence from a Large U.S. Cohort Study

Kimchi Consumption and Immune Balance: Evidence from a Controlled Human Trial

Repurposing Itraconazole as an Anticancer Agent: Mechanisms and Clinical Potential

Maternal Vitamin D Status during Pregnancy and Neurocognitive Development in Early Childhood

Overnight Olfactory Enrichment as a Novel Strategy to Enhance Memory in Older Adults
Vitamin D as a Regulator of Energy Partitioning: Insights from Preclinical Research
A 30-year-old man suffered a stroke while showering: Here are 5 things to remember when showering in cold weather to avoid accidents

Itchy Breasts? Here Are 6 Health Issues That Could Be Behind It
News Post
Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings

At thirty-seven, I walked into the Grand Westbrook Hotel in downtown Chicago wearing a simple black dress and a wool coat I’d owned for years.

I worked abroad for 5 years to buy a house for my mother – When I returned, meeting my mother was not like I imagined.

THE MORNING AFTER THE WEDDING, MY HUSBAND AND I WERE ALREADY PACKING FOR HONEYMOON WHEN I GOT A CALL FROM THE REGISTRY OFFICE: ‘SORRY, WE CHECKED YOUR DOCUMENTS AGAIN… YOU NEED TO COME IN & SEE THIS IN PERSON. COME ALONE — AND DON’T TELL YOUR HUSB

I quit my career because my husband said, “A real wife stays home.” I did—ten years of silence and sacrifice. Then he filed for divorce. His lawyer smirked, “She has no skills.

“Just the thought of sleeping with that fat pig makes me sick.” I heard my son-in-law say this about my daughter the night before their wedding. He and his friends laughed like it was nothing… But in the end, I was the one who had the last laugh.

I Was Seven Months Pregnant, Carrying Groceries Up Three Flights Of Stairs While My Husband Sat On The Couch Playing Video Games.
Boiling chicken without tap water
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail

Soaking bananas in vinegar: 4 amazing uses recognized by experts, everyone loves it
How do people who take naps and those who don't? Experts reveal surprising truth

Ants, cockroaches, mosquitoes… will gradually leave their homes thanks to these tips

Ripe bananas spoil quickly after being bought; preserve them this way so they stay bright yellow, fragrant, and firm for a whole week
Of particular note, these four unusual pains occurring every morning may be a warning sign of a tumor in the body

Don't do these 5 things in the morning if you don't want your cancer cells to grow rapidly.
Unbelievable: Adding a few drops of menthol oil to onions is ten times more effective at repelling mosquitoes and promoting better sleep than pure gold.
