
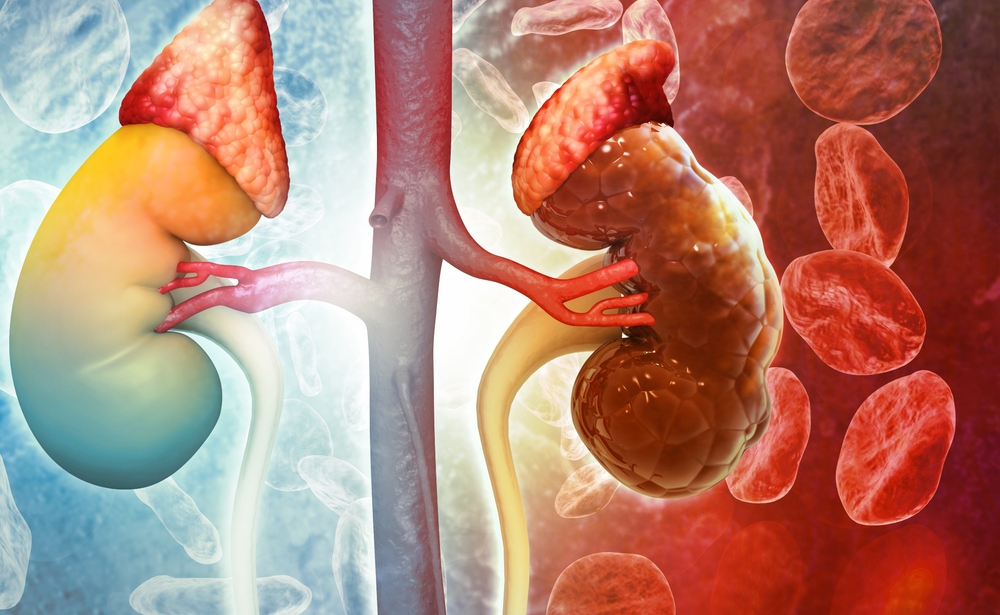
A Wearable Kidney May Finally Free Patients From Hospital Dialysis and Restore Real Independence

The Future of Kidney Care: From Dialysis Chairs to Wearable Artificial Organs
Every week, hundreds of thousands of Americans find themselves tethered to dialysis machines for survival—three times a week, four hours at a time. These hours, stretched across months and years, mean missing out on work, family gatherings, and the simple freedom of living on one’s own terms. For many patients, dialysis feels less like a treatment and more like a second, punishing job—one they never applied for but cannot quit. Alongside the time commitment come rigid restrictions on food, fluid, and activity, paired with debilitating side effects that leave patients exhausted.
Now imagine shrinking that bulky machine down to the size of a paperback book—or smaller—and making it wearable or even implantable. Instead of interrupting life, it would work silently in the background, mimicking the constant, tireless function of a healthy kidney. That vision, once science fiction, is steadily moving toward reality. Researchers worldwide are racing to develop bioartificial kidneys that could liberate patients from dialysis chairs, bypass the shortage of donor organs, and restore what dialysis rarely delivers: independence.
The Heavy Burden of Dialysis Today
Dialysis is rightly celebrated as a life-saving invention, yet it comes with enormous costs. More than half a million Americans rely on it, most through hospital-based hemodialysis. Each session lasts around four hours, three times a week, adding up to over 600 hours a year. This grueling schedule not only drains patients physically, but it also eats away at their freedom, making everyday activities—travel, work, socializing—difficult to maintain.
Unlike healthy kidneys, which filter blood continuously 24/7, dialysis only works intermittently. That gap allows toxins, electrolytes, and fluids to build up between sessions, creating dangerous swings in blood chemistry. Patients often describe the “dialysis crash”: nausea, headaches, dizziness, or muscle cramps that leave them drained long after treatment ends. Strict fluid restrictions and carefully measured diets only add to the burden, making patients feel like prisoners of their own bodies.
The toll is not only physical. Studies reveal that dialysis patients face higher rates of depression, social withdrawal, and unemployment. Families also shoulder emotional and financial strain, juggling medical appointments, transportation, and the unpredictable crises of kidney failure. Even alternatives like peritoneal dialysis—which can be done at home—are limited; the technique typically loses effectiveness after several years, forcing many patients back into clinical care.
Ultimately, dialysis is a compromise: a way to keep people alive while they wait for a kidney transplant that may never come. For many, it feels like existing in limbo—surviving, but not truly living.
Why Innovation Cannot Wait

Kidney transplantation remains the gold standard for end-stage renal disease, but access is painfully limited. In the United States, the median wait time for a kidney transplant is 3.6 years. Only about 20,000 transplants occur annually, far fewer than the number of people in need. And even after a successful transplant, patients must take lifelong immunosuppressant drugs, which increase the risk of infections, diabetes, heart disease, and even certain cancers.
Meanwhile, the vast majority of patients remain dependent on dialysis. The urgency of new solutions is magnified by the scale of the problem: nearly 37 million Americans live with chronic kidney disease—more than one in seven adults. Globally, around 3 million people rely on dialysis, a number projected to rise sharply as diabetes and hypertension increase worldwide. Kidney disease already causes more deaths each year than breast or prostate cancer, yet it receives far less attention and funding.
This is why innovation matters. The quest for wearable or implantable kidneys is not about convenience alone. It is about transforming care from a stopgap measure into a sustainable pathway that restores dignity, independence, and health.
The Promise of Wearable and Implantable Artificial Kidneys

Imagine replacing hours in a dialysis chair with a device that functions continuously, quietly balancing blood chemistry and removing toxins. This is the dream that motivates projects like The Kidney Project, a collaboration between UC San Francisco and Vanderbilt University. Their bioartificial kidney merges two systems: a filter to clear waste and a bioreactor filled with living kidney cells that carry out complex regulatory functions. Early animal trials have been promising: the device operated inside pigs for a week, performing essential kidney-like tasks without triggering immune rejection.
Dr. Shuvo Roy, the project’s technical director, explained: “Our goal is to replicate the essential functions of a kidney safely, reliably, and comfortably. The bioartificial kidney will not only make treatment more effective, but also allow patients to live without the constant burdens of dialysis.”
Wearable devices are also making strides. In 2016, a portable “wearable artificial kidney” weighing about 5 kilograms allowed patients to walk freely during 24-hour treatment sessions, successfully removing toxins without confining them to a chair. More recently, Singapore-based AWAK Pte Ltd has tested even lighter systems for peritoneal dialysis, achieving significant toxin clearance while patients went about their daily lives. These experiments demonstrate that smaller, mobile dialysis systems could extend freedom and flexibility to millions.
For patients, the appeal is obvious: no more rigid schedules, fewer hospital visits, and the possibility of traveling, working, or simply enjoying daily life with fewer interruptions. For healthcare systems, the benefits are equally compelling. In the United States alone, dialysis costs Medicare over $50 billion annually. A shift toward wearable or implantable devices could dramatically reduce costs while improving outcomes.
How the Technology Works

Building an artificial kidney requires solving two intertwined challenges: mechanical filtration and biological regulation.
-
Filtration: Devices must remove toxins like urea and excess water efficiently, just as natural kidneys do. Urea removal is particularly challenging since it is produced in large amounts daily. Scientists are experimenting with advanced sorbents, enzyme-based systems, and electrochemical methods to break down or capture urea safely.
-
Bioreactor Function: Kidneys don’t just filter—they regulate blood pressure, electrolyte balance, and hormone production. To replicate these tasks, researchers incorporate living kidney cells into a protected bioreactor. These cells are shielded from immune attack using ultra-thin silicon membranes that allow nutrients and oxygen to pass while blocking immune cells. This innovation could eliminate the need for lifelong immunosuppressants, a major advantage over transplants.
The convergence of these two systems—filtration plus biological regulation—makes artificial kidneys one of the most ambitious biomedical engineering challenges of our time.
What’s Next for Patients
The artificial kidney is moving from theoretical concept to practical reality. Early trials in animals and small-scale human studies show promise, but the road ahead requires extensive testing to prove safety and reliability over months and years. Regulatory approval from the U.S. Food and Drug Administration (FDA) will be another critical step before devices can reach patients.
Encouragingly, momentum is building. The Kidney Project recently won a $650,000 KidneyX prize, part of a government initiative to fast-track breakthroughs in kidney care. Pilot trials of wearable dialysis devices have already given patients a glimpse of greater freedom. Each milestone signals not just scientific progress, but a cultural shift: recognition that dialysis is no longer enough, and that patients deserve better.
For individuals and families, the potential impact is enormous. Reduced cardiovascular strain, fewer hospitalizations, and improved quality of life could become the norm. Patients could plan vacations, maintain careers, and engage in community life without dialysis schedules dictating every move.
Restoring Freedom, One Kidney at a Time
For decades, dialysis has been the only lifeline for millions—a way to prolong life, but rarely to restore its full richness. The promise of wearable and implantable artificial kidneys changes that. It offers a future where kidney failure is managed with dignity, where patients are no longer defined by machines and schedules, but by the lives they choose to lead.
The science is still evolving, and obstacles remain. Yet the breakthroughs achieved so far suggest a profound shift in how we approach kidney disease: not as a permanent sentence to dependency, but as a challenge that technology and medicine together can overcome. Achieving this vision will require ongoing investment, policy support, and global commitment to kidney health.
For the millions living with kidney disease today—and the millions more at risk tomorrow—these innovations represent more than medical devices. They represent hope, freedom, and the chance to reclaim ordinary life from the grip of illness.
News in the same category

PlayStation handing out rare refunds to gamers over popular new game
These three iconic iPhones set to become obsolete this month making them unable to update again

Elon Musk sparks debate with terrifying prediction about robots people claim will turn into 'nightmare'
Stephen Hawking Predicts the End of the World Is Nearer Than We Think

Why expert believes Princess Diana could have survived her 'incredibly rare' fatal injury

Man who's been walking non-stop for 27 years was banned from entering Russia

Husband of woman caught on kiss cam with CEO speaks out for first time since viral incident

Samsung blasts Apple's new iPhone with brutal posts just minutes after launch
Samsung wasted no time trolling Apple, firing off cheeky social media posts just minutes after the iPhone 17 reveal. The playful jabs have reignited the fierce rivalry between the two tech giants and sparked heated debates among fans worldwide.

Police release shocking new photos of ‘grim’ second campsite where father hid children after vanishing four years ago
Police in New Zealand have released haunting new photos of a hidden campsite where fugitive father Tom Phillips kept his three children while on the run for more than four years. The shocking discovery came just a day after Phillips was k:illed in a viole

Hacker with over 30 years experience shares the scariest things he’s seen on the dark web
Despite the bleak outlook, the hacker emphasized one hopeful trend: more former black hats like himself are turning to legitimate cybersecurity roles,

Keanu Reeves Revealed He’s Been ‘Married’ To Winona Ryder For Almost 30 Years
Keanu Reeves has stunned fans by revealing that he and Winona Ryder may have been “married” for nearly three decades—thanks to an unusual movie scene filmed in the early ’90s. What began as a role in Bram Stoker’s Dracula has turned into one of

Woman charges her husband $600 a month if he doesn't do his household chores

Trump uses shocking AI image to threaten US city with 'war'
Donald Trump has ignited outrage after posting an AI-generated image that depicts him declaring “war” on Chicago. The dramatic post, styled after Apocalypse Now, has triggered fierce backlash from state leaders and raised alarms about his political ta

Blind For 20 Years, Man Regains Sight Through His Tooth In Miracle Surgery
After two decades of darkness, a Canadian man can finally see the world again—through a groundbreaking surgery that uses his own tooth to restore vision. His emotional journey from blindness to sight has stunned both doctors and the public alike.
Angelina Jolie Says The ‘Best Sex’ She’s Ever Had On Set Was With Denzel Washington

‘Folded Boy’ Miraculously Stands Tall After Years Living With 180° Spine Bend
For over a decade, a young man in China lived with his body bent nearly in half, trapped in a painful “Z-shaped” posture that made everyday life a struggle. Now, after years of suffering and a series of groundbreaking surgeries, he has finally stood u
Man who built $20,000,000 White House replica on top of skyscraper might never get to live in it
A jaw-dropping $20 million replica of the White House, perched atop a 400-foot skyscraper in India, has been gathering dust for years. Despite its grandeur and eccentric design, the palatial home’s creator, tycoon Vijay Mallya, may never get the chance

Facebook users urged to check their bank account after 1,200,000,000 users' data is stolen in historic breach
A new cyber shockwave is sending panic through the digital world as claims emerge that 1.2 billion Facebook users may have had their personal data stolen in what could be the largest data breach in internet history. Experts are now urgently advising users
News Post

"The best plant for eyesight 👀 and much more… See more in the first comment."

The Spiritual Meaning of Black Butterflies Entering Your Home Revealed
Black butterflies carry meanings that are as complex as they are beautiful.
Add This Simple Ingredient to Your Mop Water and Keep Floors Shiny for Weeks
You don’t need fancy, high-priced cleaners to enjoy spotless, long-lasting results.
The Secret Use of the Tiny Hole in a Safety Pin Finally Revealed
That tiny hole in a safety pin is more than just decoration—it’s a brilliant example of how even the simplest tools can hold hidden design secrets. W

Bridal Glow Secret: One Glass of This Juice Daily Transforms Your Skin
This natural elixir is packed with antioxidants, anti-inflammatory compounds, and essential vitamins that work together to promote healthy, glowing skin.

Fenugreek & Onion: Thin To Thick Hair Naturally

Discover Garden Gold: Dandelion’s Hidden Power

DIY Anti-Aging Cream: Erase Wrinkles and Fine Lines Naturally at Home
By using natural ingredients like rice, honey, coconut oil, and aloe vera, you can create effective anti-aging creams that nourish, hydrate, and rejuvenate your skin.

The Black Serum To Get Long, Black Hair
Soak orange and grapefruit peels in vinegar to get a special type of water that can save you a lot of money.

Don't soak frozen meat in water. Listen to the chef's instructions on how to defrost it in 5 minutes and the meat will still be delicious.
Unbelievable amount Trump’s net worth has risen since taking office for second term

The Power of Chanca Piedra: 10 Benefits and Uses

Weight Loss Drink: Consume These 2 Detox Drinks To Lose Weight
Symptoms That Can Be Caused by Stress

What the Shape of Your Legs Might Say About Your Personality

How surgeon who amputated his own legs was caught as he's sentenced to 32 months in prison
PlayStation handing out rare refunds to gamers over popular new game

🌿 17 Health Conditions That May Benefit from Guava Leaf Tea + Easy Homemade Recipe
