Brain Pacemakers and Alzheimer’s: How Deep Brain Stimulation Could Slow Memory Loss
Johns Hopkins Medicine is leading an innovative approach in the fight against Alzheimer’s disease by testing implantable “brain pacemakers” designed to stimulate key memory-related circuits in the brain. Unlike conventional treatments that rely on medication, this experimental technique uses deep brain stimulation (DBS) to deliver approximately 130 low-voltage electrical pulses per second, with the goal of preserving brain activity and slowing cognitive decline.
The devices are surgically implanted to target the fornix, a critical bundle of nerve fibers that connects to the hippocampus, the brain region essential for memory formation and learning. In Alzheimer’s disease, the hippocampus is one of the first areas to deteriorate, leading to progressive memory loss and impaired thinking. By directly stimulating the fornix, researchers hope to activate neural pathways that are weakened by the disease and help maintain communication within the brain’s memory network.
Early evidence supporting this approach comes from clinical studies conducted in Canada, where patients with mild Alzheimer’s disease received deep brain stimulation targeting the same region. Results showed that these patients maintained higher levels of glucose metabolism in certain brain areas for more than a year compared to those who did not receive stimulation. Glucose metabolism is a widely used indicator of active and healthy brain cells, suggesting that DBS may help slow the functional decline associated with Alzheimer’s.
This strategy represents a significant departure from traditional drug-based therapies. Most Alzheimer’s medications aim to alter chemical processes in the brain, such as reducing amyloid-beta plaques or modifying neurotransmitter levels. In contrast, deep brain stimulation bypasses chemical targets altogether, directly activating neural circuits involved in memory and cognition. Researchers believe this circuit-based approach may be especially valuable given the limited success of many drug treatments in halting disease progression.
At present, eligibility for the procedure is restricted. Only patients with mild cognitive impairment or early-stage Alzheimer’s disease, and who are still able to provide informed consent, can participate in ongoing trials. This cautious approach reflects both ethical considerations and scientific evidence suggesting that earlier intervention may be more effective. Once extensive neuronal damage has occurred, stimulating weakened circuits may offer limited benefit.
Looking ahead, scientists hope that applying deep brain stimulation at even earlier stages could help preserve brain function for longer periods, potentially delaying the most debilitating symptoms of Alzheimer’s disease. While the technique is still experimental and not without risks, it highlights a growing shift in neuroscience toward treating brain disorders by modulating neural networks rather than relying solely on pharmaceuticals. If successful, brain pacemakers could become a powerful new tool in the effort to combat one of the world’s most challenging neurodegenerative diseases.
News in the same category


Dog Swept Away by Typhoon Floods in the Philippines Miraculously Finds His Way Home After Two Weeks

Snowball the Leucistic Alligator: A Rare Living Wonder Lost to Human Greed
Scientists Identify a Low-Cost, Widely Available Antidote That Could Reduce Cobra Venom Damage
China Uncovers a “Supergiant” Gold Deposit in Hunan, Potentially Reshaping Global Supply
Your Breath Is a Biometric Signature: How Breathing Patterns Can Identify Individuals and Reveal Mental Health Clues
Tree-Climbing Crocodiles: New Research Redefines What We Know About Ancient Predators
Revolutionary Microneedle Patch Offers Hope for Natural Tooth Regrowth
Revolutionizing Communication: Danny Manu's Mymanu CLIK Breaks Language Barriers Worldwide
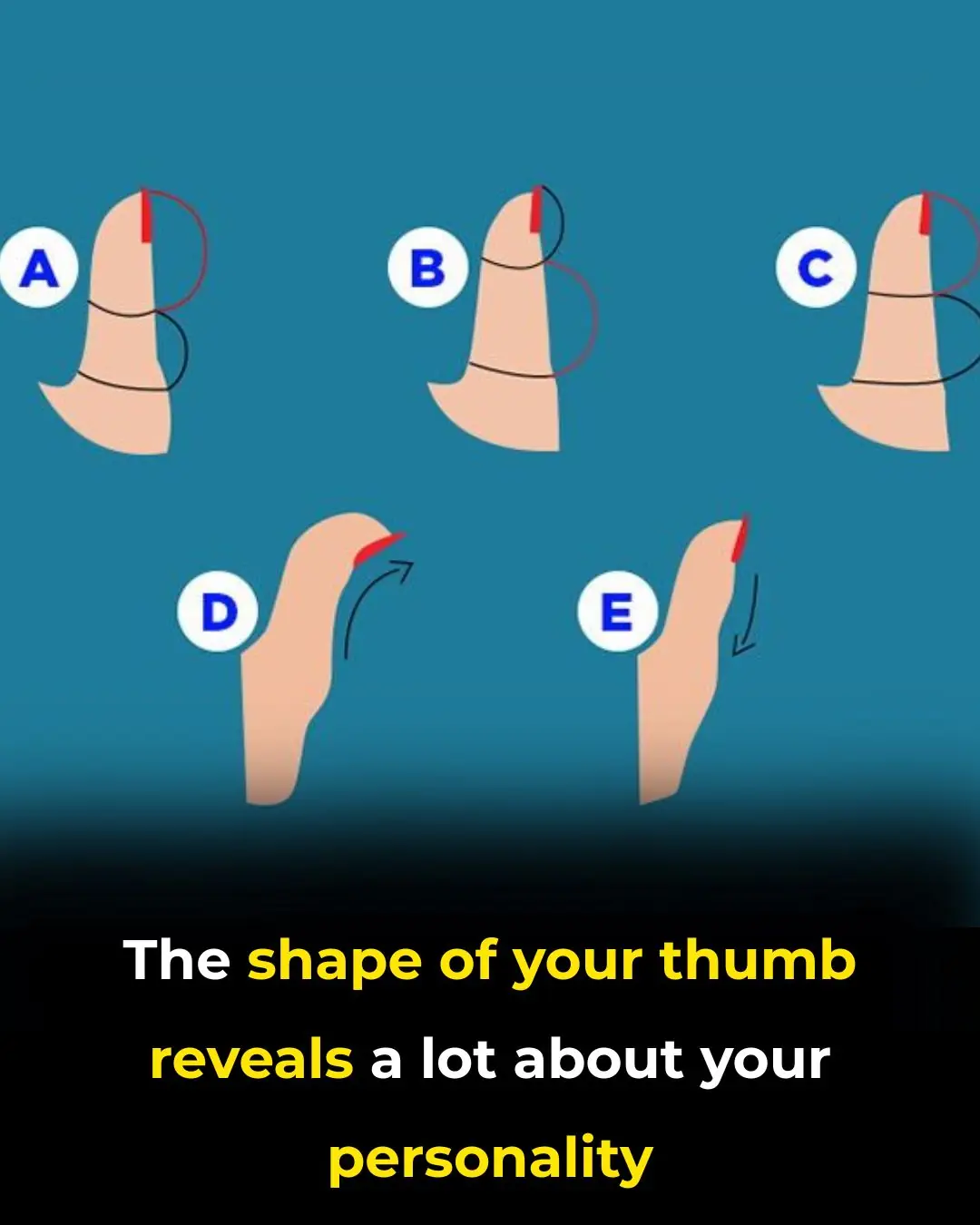
The Secrets Your Thumb Shape Reveals
Don’t Throw Away Rice Water

Say Goodbye to Swelling
Norway’s Unique Approach to Raising Confident and Healthy Children: A Deep Connection with Nature

Japan’s Bullet Trains: The Pinnacle of Precision and Passenger Respect
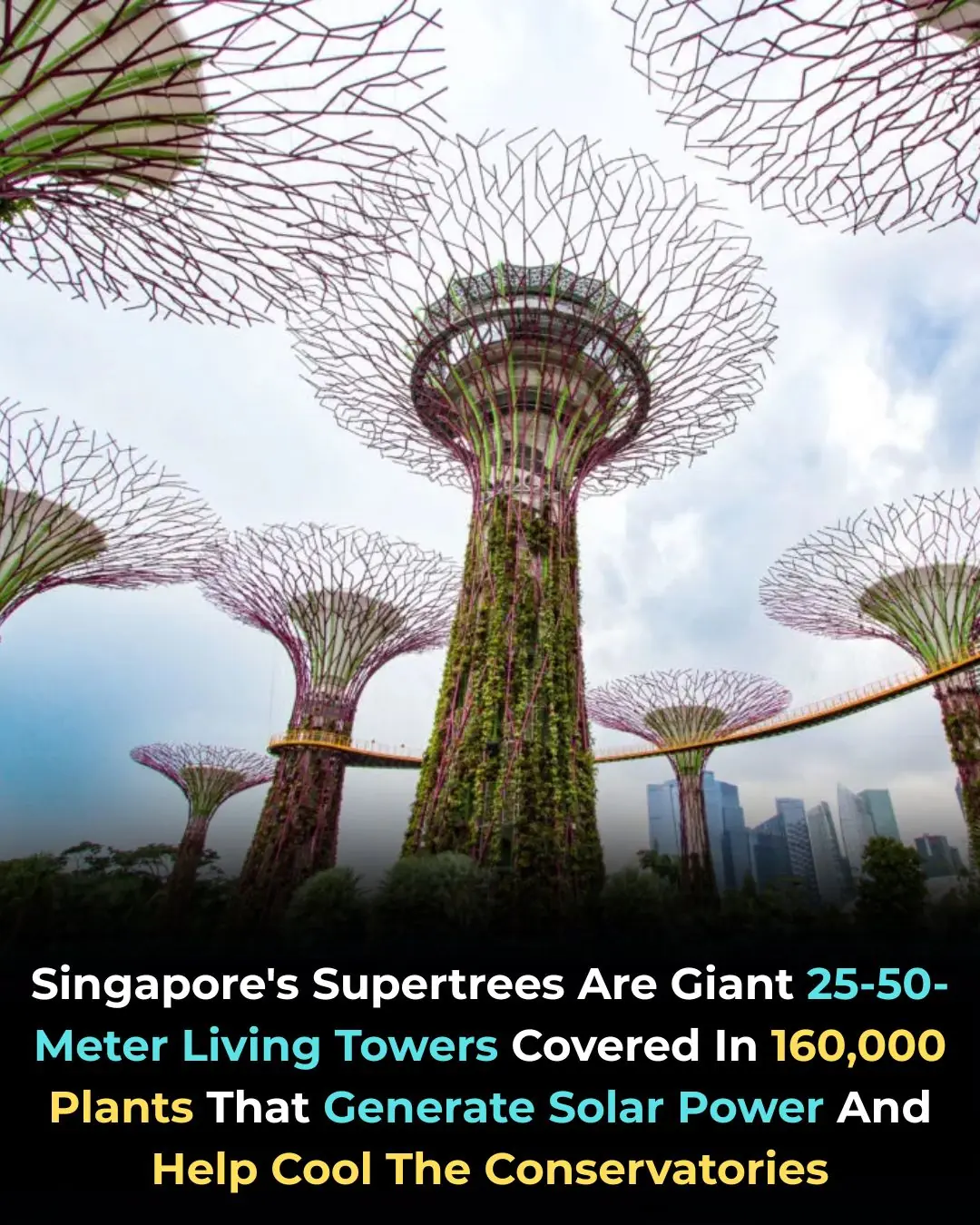
Singapore’s Supertrees: A Fusion of Architecture, Nature, and Clean Energy
The Hidden Health Risks of Eating Instant Noodles 2-3 Times a Week: What Science Really Says

Garrett Morgan: The Self-Taught Inventor Who Revolutionized Safety and Saved Lives

How Rob Kenney Became the Father Figure Millions Needed After Losing His Own Father
News Post

Bee Venom Shows Promise in Destroying Aggressive Breast Cancer Cells in Under 60 Minutes

Dog Swept Away by Typhoon Floods in the Philippines Miraculously Finds His Way Home After Two Weeks
China Tests Jumbo-Sized Hypersonic Jet Reaching Mach 6.5, Redefining Ultra-Fast Air Travel
How to Grow Rosemary Abundantly at Home: Your Aromatic, Memory-Supportive Garden Ally
Blood pressure creeping up? 10 natural fixes before meds
What does it symbolize when a person who passed away appears in your dream

Snowball the Leucistic Alligator: A Rare Living Wonder Lost to Human Greed
Scientists Identify a Low-Cost, Widely Available Antidote That Could Reduce Cobra Venom Damage
China Uncovers a “Supergiant” Gold Deposit in Hunan, Potentially Reshaping Global Supply
Your Breath Is a Biometric Signature: How Breathing Patterns Can Identify Individuals and Reveal Mental Health Clues
Tree-Climbing Crocodiles: New Research Redefines What We Know About Ancient Predators
Revolutionary Microneedle Patch Offers Hope for Natural Tooth Regrowth
Revolutionizing Communication: Danny Manu's Mymanu CLIK Breaks Language Barriers Worldwide
🫁 The Real Causes of Constant Phlegm and Mucus in Throat — And How to Get Rid of It

The Hidden Danger on Your Fruit — and the Simple Method That Can Make It Safer
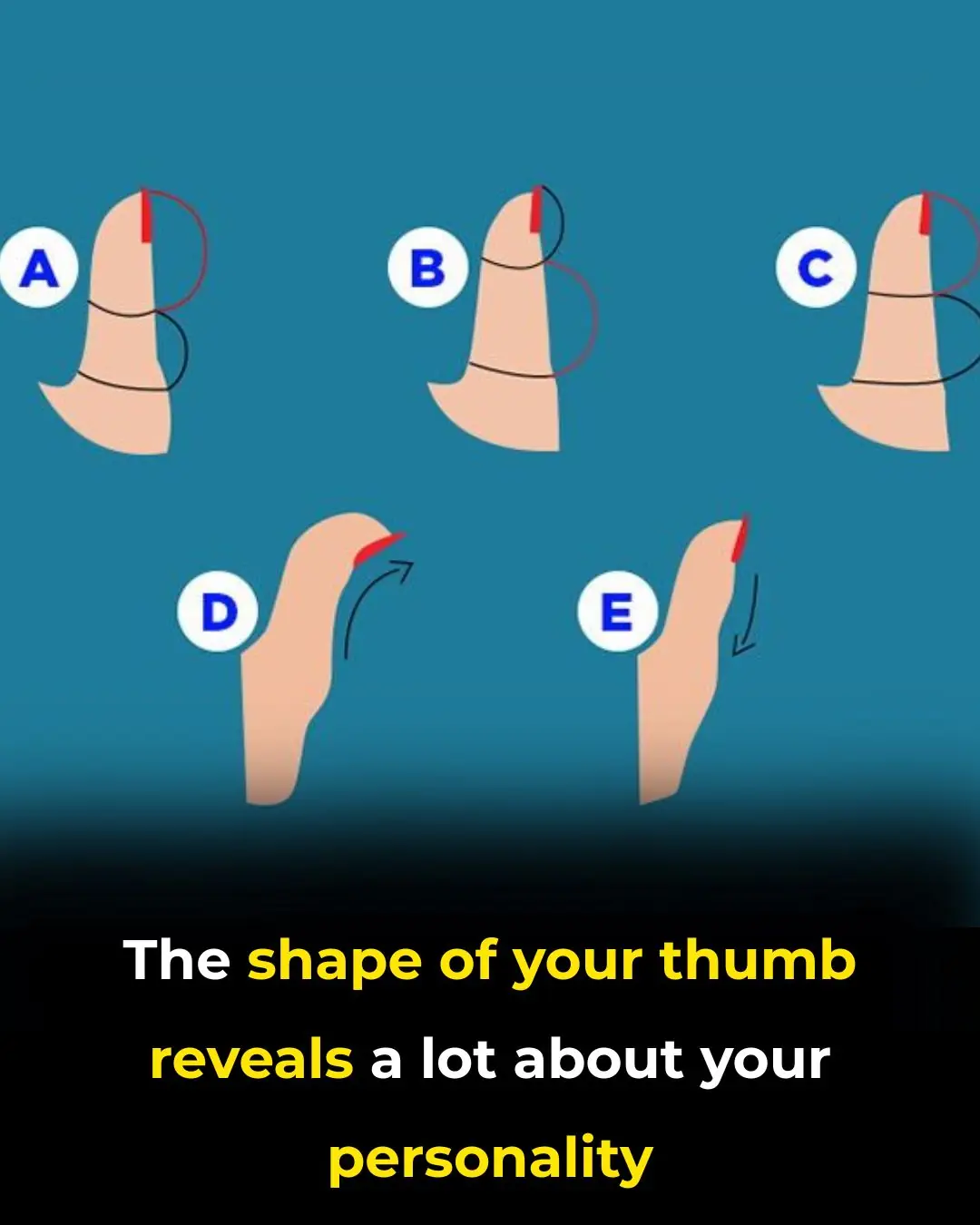
The Secrets Your Thumb Shape Reveals
5 Signs Your Lungs are Being Exposed to Mold
How Cancer Spreads Through The Lymphatic System (And How To Keep It Healthy)