How Chronic People-Pleasing Could Increase Your Risk of Autoimmune Disease
New research suggests that constantly trying to please others may have more serious consequences for your health than previously understood. People who chronically prioritise the needs and expectations of others — often at the expense of their own well-being — may be placing their bodies under sustained psychological pressure. This prolonged pattern of emotional self-sacrifice can activate long-lasting stress responses, which, over time, may weaken the immune system and make the body more vulnerable to illness.
Scientists warn that persistent stress activates the body’s hypothalamic–pituitary–adrenal (HPA) axis, resulting in elevated cortisol levels for extended periods. While cortisol is helpful in short bursts, chronic overproduction can suppress normal immune function and disrupt inflammatory pathways. According to a review published in Nature Reviews Immunology, long-term emotional stress can promote immune dysregulation and increase susceptibility to chronic inflammatory disorders. In the context of autoimmune diseases — where the immune system begins to attack the body’s own healthy tissues — this stress-related dysregulation may play an important contributory role.
Growing evidence links high levels of emotional stress to an increased risk of autoimmune conditions such as rheumatoid arthritis, systemic lupus erythematosus, Hashimoto’s thyroiditis, and multiple sclerosis. A study in JAMA Psychiatry found that individuals who experienced chronic psychological stress had a significantly higher likelihood of developing certain autoimmune diseases later in life. While stress alone is not the direct cause, it is considered a meaningful risk factor that can exacerbate underlying genetic or environmental vulnerabilities.
This research highlights the profound — and often hidden — impact that emotional and behavioural patterns can have on physical health. People-pleasing habits, such as overcommitting, avoiding conflict, difficulty saying “no,” and prioritising others’ needs above one’s own, are frequently associated with burnout, anxiety, and emotional exhaustion. Experts emphasise that these psychological strains, when left unaddressed, may gradually influence biological systems in ways that undermine immune resilience.
Health professionals increasingly encourage individuals to establish healthy boundaries, practice assertive communication, and prioritise regular self-care. Cultivating mental well-being — through stress management techniques such as mindfulness, therapy, exercise, and balanced lifestyle choices — is essential for protecting not only emotional health but also immune function. As explained by researchers at the National Institute of Mental Health (NIMH), mental well-being plays a crucial role in regulating stress hormones and supporting immune balance.
Understanding the intricate link between behaviour, stress, and immunity could transform future approaches to preventing autoimmune diseases. Instead of focusing solely on biological and environmental triggers, researchers argue that emotional health should be viewed as a central pillar of disease prevention. This integrative perspective underscores that mental well-being is just as critical as physical well-being, particularly in a world where chronic stress is increasingly common.
As scientists continue to explore how psychological habits shape long-term health outcomes, it becomes ever clearer that protecting the immune system requires a holistic approach. Recognising the health risks associated with chronic people-pleasing is a powerful first step toward promoting healthier behaviour patterns — and ultimately fostering a stronger, more resilient body and mind.
News in the same category

🚶 The Power of Post-Meal Movement: Why a Ten-Minute Walk is a Game-Changer for Blood Sugar Control
✨ The Unsung Mineral: How Magnesium Deficiency Compromises Nerve Signaling and Undermines Holistic Health
🎮 The Virtual Battlefield: How the British Army is Leveraging Call of Duty for Next-Generation Tactical Training
🍔 The Hijacked Brain: How Ultra-Processed Foods Mimic Addiction and Disrupt Decision-Making
Autophagy: How Your Body's 'Self-Cleaning' Process Boosts Health and Longevity
Groundbreaking Stem Cell Therapy Reverses Type 1 Diabetes, Restoring Natural Insulin Production
Breakthrough Ready-Made Immune Cell Therapy Shows Promise in Treating Advanced Kidney Cancer
Early Detection of Testicular Cancer: The Key to Saving Lives in Young Men
New Research Shows Coffee Consumption Can Reduce Liver Cancer Risk by 43%

Why Do We Get Shocked by Static Electricity

What Clearing the Table Says About You

What is their purpose in doing so?
🛁 Say Goodbye to the Shower: Japan Unveils the 15-Minute "Human Washing Machine"
Fingerprint Individuality: A Story Written by Biology, Environment, and Chance

Northwestern Study Reveals Hidden Dangers in Youth Skincare Influencer Culture
Scientists Discover a Brain Receptor That Acts as a Natural Shield Against Alzheimer’s
A Fluorescent Breakthrough: New Dye Helps Surgeons Precisely Target Prostate Cancer
News Post

Put aluminum foil under the pillow before going to bed what happens
💉 The Future of Cardiac Screening: New Blood Test Detects Hidden Heart Disease Years Before Symptoms
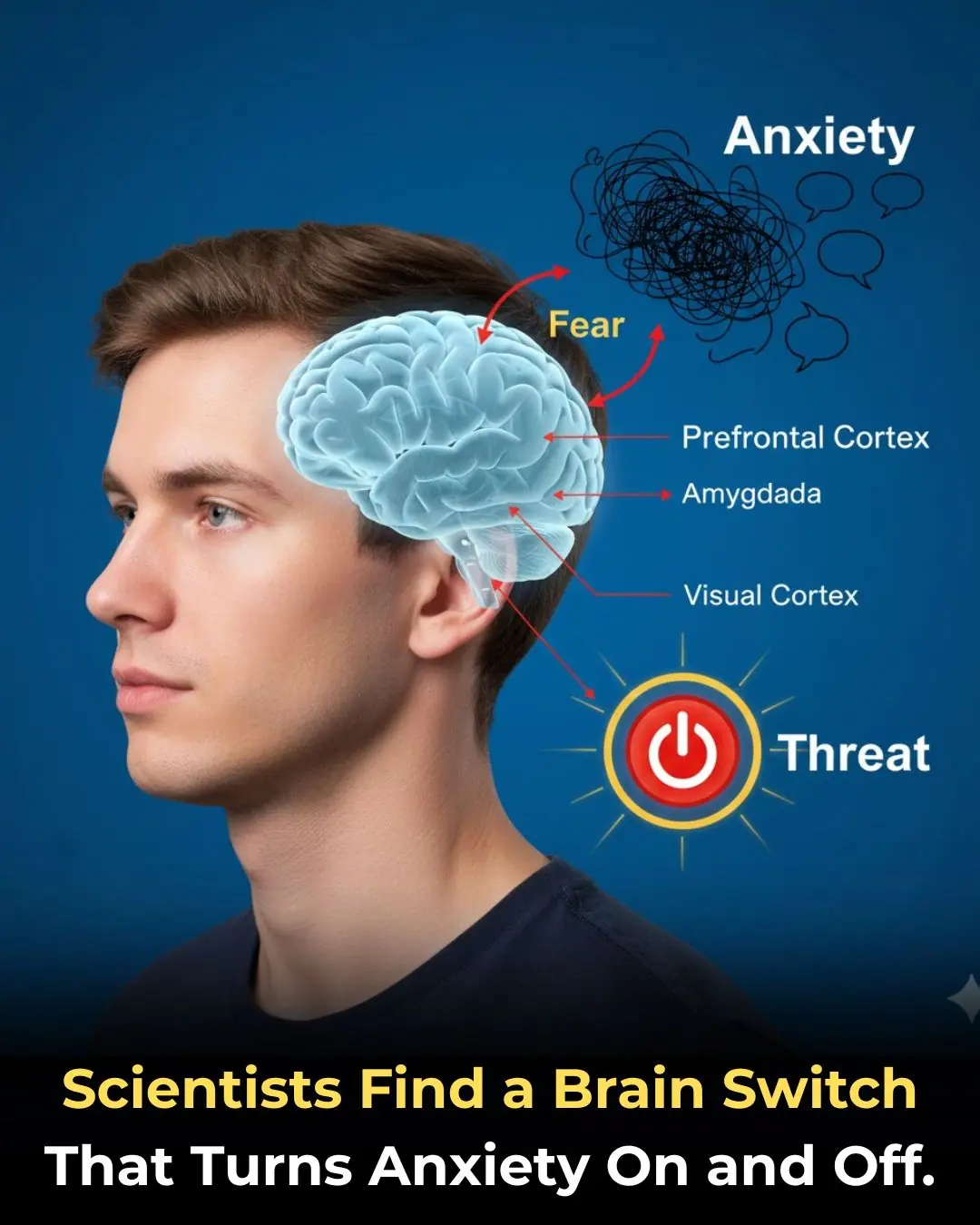
🧠 The Anxiety Circuit: Discovery of a Neural Pathway That Functions as an On/Off Switch for Fear

🚶 The Power of Post-Meal Movement: Why a Ten-Minute Walk is a Game-Changer for Blood Sugar Control
✨ The Unsung Mineral: How Magnesium Deficiency Compromises Nerve Signaling and Undermines Holistic Health
🎮 The Virtual Battlefield: How the British Army is Leveraging Call of Duty for Next-Generation Tactical Training
🍔 The Hijacked Brain: How Ultra-Processed Foods Mimic Addiction and Disrupt Decision-Making
Autophagy: How Your Body's 'Self-Cleaning' Process Boosts Health and Longevity
Groundbreaking Stem Cell Therapy Reverses Type 1 Diabetes, Restoring Natural Insulin Production
Breakthrough Ready-Made Immune Cell Therapy Shows Promise in Treating Advanced Kidney Cancer
Early Detection of Testicular Cancer: The Key to Saving Lives in Young Men
New Research Shows Coffee Consumption Can Reduce Liver Cancer Risk by 43%
Clothes are easily wrinkled when washed: Put something cheap in the machine when washing, the clothes will come out flat.
Refrigerator leaks water, slows down cooling: Women can learn how to fix it themselves, no need to call a technician

Why Do We Get Shocked by Static Electricity

What Clearing the Table Says About You
The Magic of Lemon Juice and Activated Charcoal: Natural DIY Solutions for Skin and Teeth

Improve Eyesight Naturally With Onion Tea: Benefits, Uses & How to Make It
