💉 The Future of Cardiac Screening: New Blood Test Detects Hidden Heart Disease Years Before Symptoms
Cardiovascular disease (CVD) remains the leading cause of death globally, primarily because its most dangerous stages—arterial damage and silent atherosclerosis—often progress undetected for years before culminating in acute events like heart attacks or strokes. However, a significant advancement in diagnostic medicine promises to fundamentally change this trajectory. Researchers have discovered a sophisticated blood test that can detect early heart disease years before symptoms like chest pain or shortness of breath manifest.
This innovative screening tool leverages the power of molecular biology and advanced diagnostics to identify hidden cardiovascular risk with unprecedented accuracy.
Decoding Silent Damage with Biomarkers
The new blood test moves beyond traditional risk factors (such as cholesterol and blood pressure) by measuring a panel of specific protein biomarkers and inflammatory markers that directly indicate subclinical atherosclerosis—the build-up of plaque within the arteries—and hidden arterial damage.
These markers provide a molecular snapshot of the body's inflammatory response to early disease progression:
-
Protein Signatures: The test focuses on a combination of specific proteins. Key examples include:
-
Immunoglobulin A2 ($\text{IgA2}$): A protein associated with chronic inflammation and immune responses that play a role in plaque development.
-
Apolipoprotein A ($\text{APOA}$): A component of HDL ("good") cholesterol, whose structure and function can be altered early in disease.
-
Haptoglobin ($\text{HPT}$): A protein associated with oxidative stress and the breakdown of hemoglobin, indicating systemic damage.
-
-
Inflammatory and Complement Markers: The inclusion of markers like complement protein $\text{C}5$—a central part of the body's immune system—provides evidence of low-grade, chronic inflammation, a known driver of arterial stiffness and plaque instability.
-
Baseline Risk Metrics: To ensure comprehensive predictive power, the test intelligently combines these novel proteins with established metrics, including lipid levels (cholesterol, triglycerides) and high-sensitivity troponin (a protein released when heart muscle is damaged, even minimally).
Predictive Power and Clinical Utility
Studies demonstrating the efficacy of this multi-marker panel have shown remarkable results: by combining the data from these proteins, lipids, and troponin, researchers can predict future cardiovascular events (such as non-fatal heart attacks or strokes) with significantly greater accuracy than current standard screening tools. The ability to detect arterial disease years in advance allows clinicians to establish a "risk window" before the disease becomes acute.
This early detection method transforms the clinical approach from reactive intervention (treating symptoms after an event) to proactive prevention. This has profound implications for patient care:
-
Timely Intervention: Doctors can identify asymptomatic, high-risk individuals and implement aggressive lifestyle modifications (diet, exercise) and targeted pharmacological treatments (statins, anti-inflammatory drugs) years before a catastrophic event might occur.
-
Personalized Risk Assessment: The precise signature of biomarkers allows for personalized treatment plans that address the specific biological drivers of the patient's disease (e.g., targeting inflammation versus lipid levels).
1
Advances in blood testing technology, leveraging sophisticated techniques like mass spectrometry and advanced immunoassay, have made this complex panel practical and cost-effective. By identifying the molecular fingerprints of silent disease, this innovation ensures that patients receive the timely intervention necessary for better long-term heart health, solidifying the test's role as a cornerstone of preventative cardiology.
📚 References
-
European Heart Journal / Circulation: (Leading cardiology journals where research on novel cardiovascular biomarkers and predictive panels is published).
2 -
American Heart Association (AHA) and European Society of Cardiology (ESC) Guidelines: (Official bodies that review and integrate new diagnostic technologies into clinical practice).
-
Clinical Chemistry / Atherosclerosis, Thrombosis, and Vascular Biology (ATVB): (Academic sources detailing the function and clinical relevance of proteins like $\text{IgA2}$ and $\text{HPT}$ in vascular disease).
News in the same category


Canadian Scientists Develop Mini Robot to Treat Kidney Stones Without Surgery

🚿 8 Bathroom Habits That Ruin Your Feeling of Freshness (And How to Fix Them)

Rebuilding with Purpose: Japan’s Monumental Tsunami Wall and Living Forest Shield

Which Raw Food Would You Eat
A Heartfelt Goodbye: Graduate’s Simple Thank-You Moves Security Guard to Tears
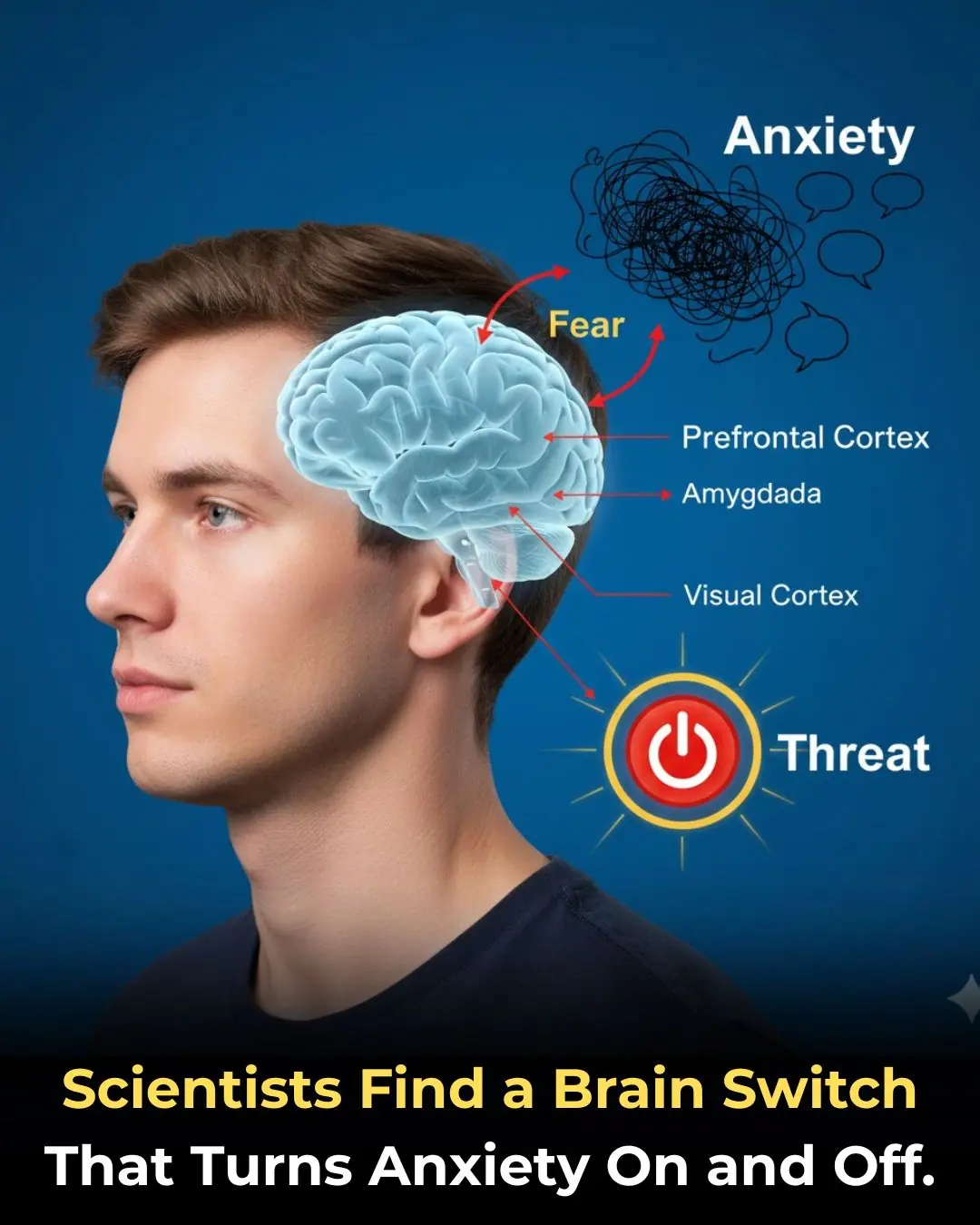
🧠 The Anxiety Circuit: Discovery of a Neural Pathway That Functions as an On/Off Switch for Fear

🚶 The Power of Post-Meal Movement: Why a Ten-Minute Walk is a Game-Changer for Blood Sugar Control
✨ The Unsung Mineral: How Magnesium Deficiency Compromises Nerve Signaling and Undermines Holistic Health
🎮 The Virtual Battlefield: How the British Army is Leveraging Call of Duty for Next-Generation Tactical Training
🍔 The Hijacked Brain: How Ultra-Processed Foods Mimic Addiction and Disrupt Decision-Making
How Chronic People-Pleasing Could Increase Your Risk of Autoimmune Disease
Autophagy: How Your Body's 'Self-Cleaning' Process Boosts Health and Longevity
Groundbreaking Stem Cell Therapy Reverses Type 1 Diabetes, Restoring Natural Insulin Production
Breakthrough Ready-Made Immune Cell Therapy Shows Promise in Treating Advanced Kidney Cancer
Early Detection of Testicular Cancer: The Key to Saving Lives in Young Men
New Research Shows Coffee Consumption Can Reduce Liver Cancer Risk by 43%

Why Do We Get Shocked by Static Electricity

What Clearing the Table Says About You
News Post

You’re doing it all wrong. Here’s the right way to organize fridge

Canadian Scientists Develop Mini Robot to Treat Kidney Stones Without Surgery

12 medications you should never mix with coffee

Juniper: 20 Remarkable Benefits and How to Use It

🚿 8 Bathroom Habits That Ruin Your Feeling of Freshness (And How to Fix Them)

Homemade Herbal Hair Oil – Adivasi Hair Oil

Rebuilding with Purpose: Japan’s Monumental Tsunami Wall and Living Forest Shield

Which Raw Food Would You Eat
WARNING: This common pill causes dementia
A Heartfelt Goodbye: Graduate’s Simple Thank-You Moves Security Guard to Tears

This Is One Of The Most C.ancer-Causing Foods – Stop Eating It!

Put aluminum foil under the pillow before going to bed what happens
🧠 The Anxiety Circuit: Discovery of a Neural Pathway That Functions as an On/Off Switch for Fear

🚶 The Power of Post-Meal Movement: Why a Ten-Minute Walk is a Game-Changer for Blood Sugar Control
✨ The Unsung Mineral: How Magnesium Deficiency Compromises Nerve Signaling and Undermines Holistic Health
🎮 The Virtual Battlefield: How the British Army is Leveraging Call of Duty for Next-Generation Tactical Training
🍔 The Hijacked Brain: How Ultra-Processed Foods Mimic Addiction and Disrupt Decision-Making
How Chronic People-Pleasing Could Increase Your Risk of Autoimmune Disease