WARNING: This common pill causes dementia
Are you currently taking common medications for allergies, insomnia, anxiety, depression, or bladder problems? It may be time to take a closer look, because many of these everyday drugs could be silently increasing your risk of developing dementia. A growing body of research indicates that taking certain medications daily for just 12 months may raise dementia risk by up to 50%. What’s most concerning is that these are not rare or experimental drugs—they are medications that millions of people use routinely, often without realizing their long-term effects.
🧠 Understanding Anticholinergics: How They Disrupt the Brain
These medications belong to a drug class known as anticholinergics. They work by blocking a crucial neurotransmitter called acetylcholine, which plays an essential role in transmitting signals between brain cells. You can think of acetylcholine as the brain’s internal wiring system—necessary for memory formation, attention, muscle control, and overall cognitive function.
When anticholinergic medications are taken repeatedly over long periods, they interfere with this communication system. The signals between neurons become less efficient, contributing to memory problems and, with continued use, potentially increasing the risk of dementia. The alarming part is how often these drugs are prescribed or purchased over the counter with little awareness of their cognitive impact.
📌 Key Takeaways
-
Anticholinergic medications block acetylcholine, a neurotransmitter essential for memory, learning, and attention.
-
Long-term use is linked to brain shrinkage, impaired communication between neurons, and a significant increase in dementia risk.
-
These drugs appear in many common over-the-counter and prescription medications, sometimes without clear labeling.
-
Older adults and people taking multiple anticholinergics face particularly high risks.
-
Safer alternatives are available for many common conditions.
🔍 Where These Drugs Hide: Common Sources of Anticholinergics
Anticholinergic activity is found in a surprising number of familiar medications. Many people take these drugs without ever being told they carry cognitive risks:
-
Allergy Medications: First-generation antihistamines such as Benadryl (diphenhydramine).
-
Sleep Aids: Popular over-the-counter products like Tylenol PM and Unisom.
-
Anxiety Medications: Drugs such as hydroxyzine (Vistaril, Atarax).
-
Bladder Control Medications: Common prescriptions like Ditropan (oxybutynin) or Detrol (tolterodine).
-
IBS Medications: Antispasmodics like bentyl (dicyclomine).
-
Motion Sickness Treatments: Scopolamine patches used for nausea prevention.
Whether prescription or OTC, these drugs can have similar long-term effects on the brain, especially when used daily.
⚙️ The Science Behind the Cognitive Risks
A large number of clinical studies have explored the association between anticholinergic use and cognitive decline:
-
A systematic review and meta-analysis involving more than 1.5 million people found that anticholinergic use is an independent risk factor for both all-cause dementia and Alzheimer’s disease. Importantly, the risk increased with higher cumulative exposure.
-
Another meta-analysis of 21 studies showed that using anticholinergics for longer than three months was associated with an average 46% higher risk of dementia compared to no use.
-
Brain-imaging studies have revealed that anticholinergic medications are linked to increased brain atrophy, particularly in regions responsible for memory and learning. These changes suggest a real, physical impact on brain structure—not just temporary drowsiness or confusion.
Together, these findings create a compelling case that long-term use of anticholinergics is not harmless and may contribute to accelerated cognitive aging.
🛠️ How Anticholinergics Impair the Brain
Acetylcholine normally binds to muscarinic receptors located throughout the brain. These receptors play essential roles in learning, memory consolidation, and attention. Areas such as the hippocampus—the brain’s memory center—rely heavily on acetylcholine to function properly.
By blocking these receptors, anticholinergic drugs interrupt the communication pathways required for normal cognitive processing. Short-term consequences may include:
-
Brain fog
-
Confusion
-
Impaired attention
-
Slower reaction times
But with prolonged exposure, these disruptions can lead to:
-
Loss of synaptic efficiency
-
Structural brain changes
-
Accelerated cognitive decline
-
Higher risk of dementia diagnoses later in life
This is especially harmful for older adults, whose natural acetylcholine levels already decrease with age. Adding anticholinergic medications creates a compounding effect that may significantly heighten cognitive vulnerability.
⚠️ Who Is Most at Risk?
While anyone can experience the cognitive side effects of anticholinergic medications, certain groups face considerably higher risk:
-
Adults over 60: Natural age-related decreases in acetylcholine make this group more susceptible.
-
Individuals with pre-existing memory issues or mild cognitive impairment: Anticholinergics may worsen symptoms.
-
People taking multiple anticholinergic medications: Even small doses can add up.
-
Example: A person taking a sleep aid, allergy medication, and bladder control drug simultaneously may unknowingly be exposed to a high cumulative anticholinergic burden.
-
✅ Safer Alternatives: What You Can Choose Instead
Although some anticholinergic medications are medically necessary, many are used for conditions that have safer, equally effective alternatives. Here are some options to discuss with your doctor:
For Sleep
-
Melatonin
-
Magnesium
-
Ashwagandha
-
Chamomile
-
Prescription option: Trazodone, which has minimal anticholinergic activity
For Allergies
-
Second-generation antihistamines like Zyrtec, Claritin, or Allegra
-
These have much lower anticholinergic activity than older options such as Benadryl.
-
For Bladder Control
-
Non-anticholinergic option: Mirabegron (Myrbetriq)
For IBS
-
Peppermint oil
-
Targeted prescription treatments depending on whether IBS is constipation- or diarrhea-predominant
-
Dietary interventions such as low-FODMAP diets under medical guidance
What You Should Do First
-
Review your medication list carefully.
-
Speak with your doctor or pharmacist about which medications carry anticholinergic effects.
-
Never discontinue medications without medical guidance.
🚀 Protecting Your Brain for the Long Term
If you’ve been using anticholinergic medications for a while, there is no need to panic. There are many steps you can begin taking today to reduce risk and promote long-term brain health:
-
Prioritize high-quality sleep
-
Incorporate regular physical activity
-
Support cardiovascular health, since heart health and brain health are closely linked
-
Address other risk factors such as insulin resistance, hypertension, and chronic inflammation
By becoming more aware of the medications you use and discussing safer options with your healthcare provider, you can take meaningful steps toward reducing your dementia risk and protecting your cognitive function as you age.
News in the same category


This Is One Of The Most C.ancer-Causing Foods – Stop Eating It!

Improve Eyesight Naturally With Onion Tea: Benefits, Uses & How to Make It

Roll your feet daily—unlock rapid healing throughout your body!
Diabetes? Just boil these leaves to lower blood sugar (without medications)!
How to Get Rid of Bad Breath (Halitosis): Scientifically Proven Home Remedies

One simple scoop a day can spark full-body healing — here’s what happens next
Losing Just 1 Gram of Fat In The Pancreas Will Have THIS Effect On Your Body
The best way to lower blood pressure fast!

Top 12 Symptoms of Poor Blood Circulation in Legs

5 Serious Health Problems Your Nails Could Be Trying to Warn You About

How to Get Rid of Bad Breath (Halitosis): Scientifically Proven Home Remedies

Got High Blood Pressure? Try This 2-Ingredient Tea!

5 Foods That Dramatically Improve Blood Flow to Your Legs
Doctors warn: Statins may deplete vitamin K₂ and raise your risk of dangerous artery calcification

The step-by-step plan to drop 30 pounds quickly in 2025

7 Surprising Health Benefits of Cloves for Men

The Medicinal Powers of Turmeric That Doctors Rarely Mention
The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain
News Post

Canadian Scientists Develop Mini Robot to Treat Kidney Stones Without Surgery

12 medications you should never mix with coffee

Juniper: 20 Remarkable Benefits and How to Use It

🚿 8 Bathroom Habits That Ruin Your Feeling of Freshness (And How to Fix Them)

Homemade Herbal Hair Oil – Adivasi Hair Oil

Rebuilding with Purpose: Japan’s Monumental Tsunami Wall and Living Forest Shield

Which Raw Food Would You Eat
A Heartfelt Goodbye: Graduate’s Simple Thank-You Moves Security Guard to Tears

This Is One Of The Most C.ancer-Causing Foods – Stop Eating It!

Put aluminum foil under the pillow before going to bed what happens
💉 The Future of Cardiac Screening: New Blood Test Detects Hidden Heart Disease Years Before Symptoms
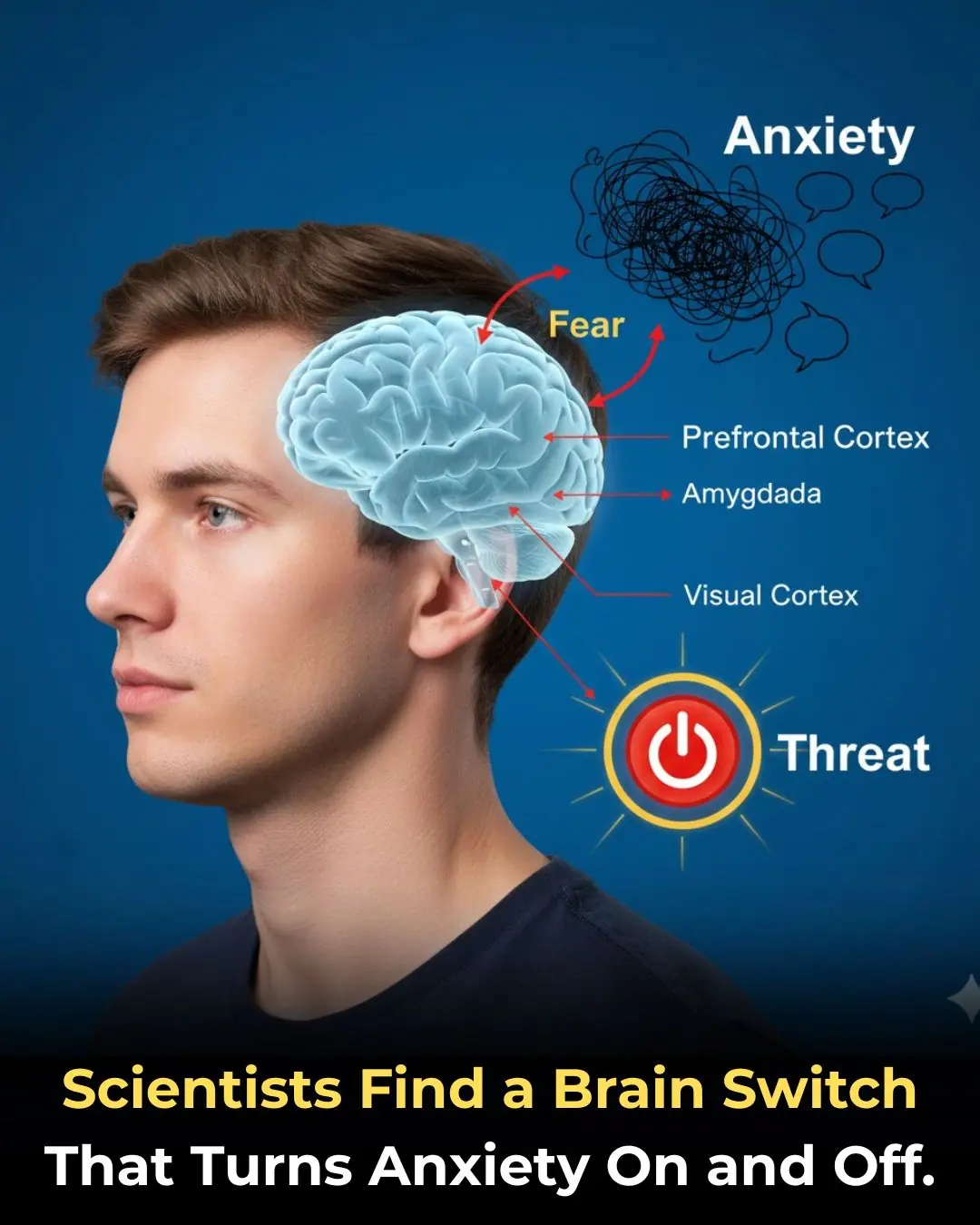
🧠 The Anxiety Circuit: Discovery of a Neural Pathway That Functions as an On/Off Switch for Fear

🚶 The Power of Post-Meal Movement: Why a Ten-Minute Walk is a Game-Changer for Blood Sugar Control
✨ The Unsung Mineral: How Magnesium Deficiency Compromises Nerve Signaling and Undermines Holistic Health
🎮 The Virtual Battlefield: How the British Army is Leveraging Call of Duty for Next-Generation Tactical Training
🍔 The Hijacked Brain: How Ultra-Processed Foods Mimic Addiction and Disrupt Decision-Making
How Chronic People-Pleasing Could Increase Your Risk of Autoimmune Disease
Autophagy: How Your Body's 'Self-Cleaning' Process Boosts Health and Longevity