Opioids and Surgery: How to Know Your Usage Risk Going In
Feb. 25, 2025 – Planning surgery? Talking to your doctor about pain management beforehand could keep you off the path to long-term opioid use, a risk factor for addiction.
If the operation is of the spine, head, or neck, that goes double for you. People who have these procedures are among the most likely to get “new persistent opioid use,” or NPOU, according to a new study from Austria. Other surgeries with higher NPOU rates included knee replacement and removal of part or all of the colon.
“Pain relief after surgery is a key component to successful recovery after surgery,” said Mark Bicket, MD, PhD, an expert in pain management after surgery who was not involved in the study. “For patients worried about taking opioids, how to manage pain is an important topic to discuss with your surgeon before your procedure.”
The findings, published this month in JAMA Network Open, align with previous research in the U.S. But this latest study is notable because Austrian doctors are considered less liberal in prescribing opioids than American ones are, and also because Austria has public health insurance. Among the efforts to curb the U.S. opioid epidemic is a focus on reducing opioid prescribing.
The researchers concluded that although health care system factors like prescribing restrictions likely play a role, a surgical patient’s history is important to consider as well. The study adds weight to an established link between prior opioid use and heightened risk of NPOU – meaning surgical patients who have previously taken opioids for any reason are at risk of taking them for months afterward, compared to those who are “opioid naïve,” a medical term for people who’ve never taken the highly addictive drugs.
NPOU is not considered an addiction or misuse necessarily, but instead is defined as a “complication” of surgery. In the study, it was defined as filling at least one opioid prescription within the first 90 days after surgery, and then filling at least one more within the subsequent 90 to 180 days. The study included all types of opioid prescriptions, including for buprenorphine, dihydrocodeine, fentanyl, methadone and levomethadone, morphine, oxycodone, and tramadol.
The study included more than 550,000 people who had one of these surgery types sometime from 2016 through 2021: abdominal wall hernia repair, appendectomy, cholecystectomy, colectomy, mastectomy and other breast surgery, prostatectomy, thyroidectomy, laryngeal surgery and other head and neck procedures, hysterectomy, spine surgery, coronary artery bypass graft, and knee or hip replacement. Overall, 1.7% of people developed NPOU, with the highest rate observed among people who had spinal surgery, at 6.8%.
Studies in the U.S. have shown much higher rates of post-surgical NPOU (as high as 7%), the study authors noted. A study published in 2021 found that 1 in 5 people used opioids for longer than three months after total hip or knee replacement.
The takeaway is not to tough out pain after surgery, though.
“It is important for patients to communicate with their physicians if their pain is not well managed after surgery,” said Bicket, a University of Michigan anesthesiologist and pain medicine specialist who cares for patients in the operating room, hospital, and outpatient clinic who have acute and chronic pain.
“Poor pain management may signal a need to be examined by their surgical team. That check-in can help determine the right next step to keep their recovery on track,” he said. “One key risk from untreated or undertreated pain is chronic pain, so it’s important that pain is managed well after surgery.”
News in the same category

Mediterranean Diet Linked to Lower Risk of Multiple Sclerosis, Study Finds
Four Common Foods You Should Never Combine with Chicken: A Common Mistake That Can Harm Your Health

The 18 Best Low-Carb Vegetables to Eat on the Keto Diet

6 Tips for Recovering From a Sleepless Night
11 Ways to Break a Bad Habit

Exploring Potatoes and Ginger as a Natural Approach to Brighter and More Even Skin Tone
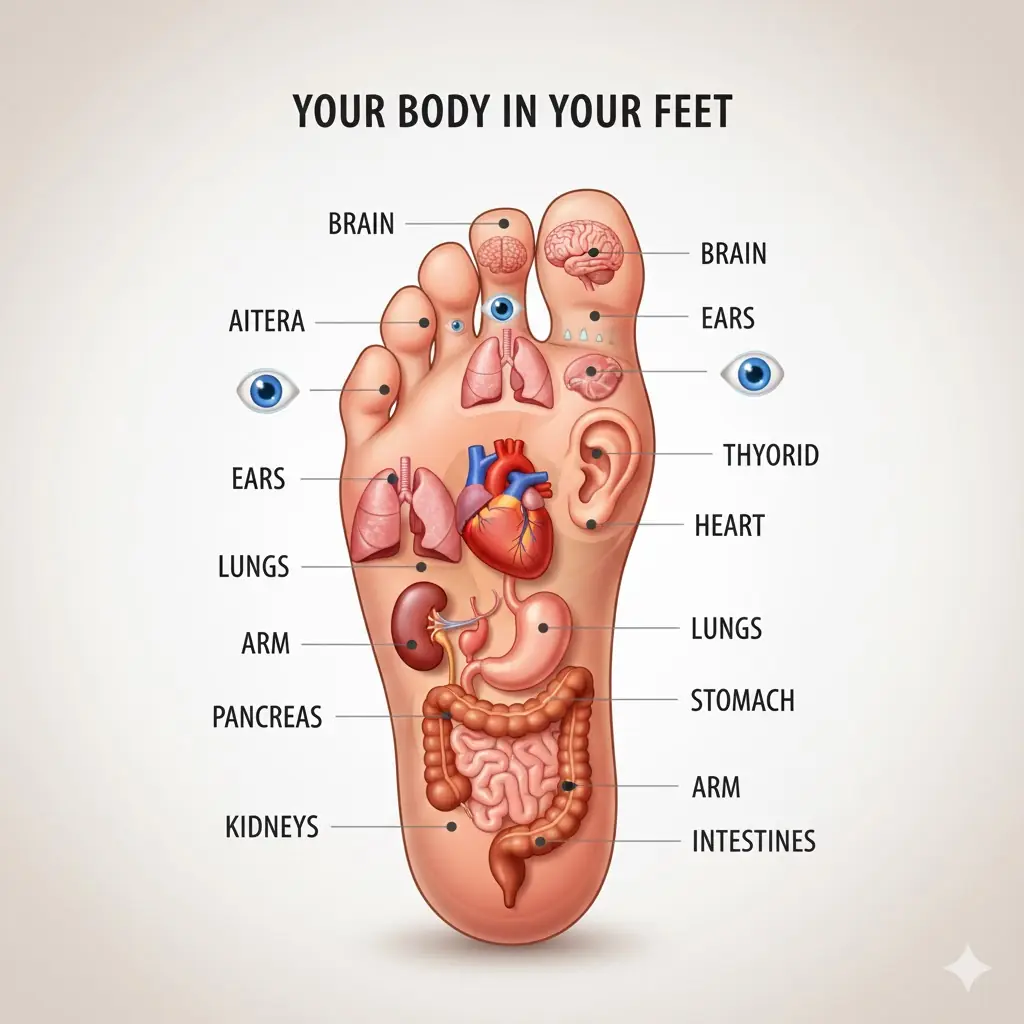
A Simple Bedtime Foot Oil Ritual: Traditional Wisdom and Modern Perspectives on Relaxation and Sleep

What Happens When You Try Incorporating Papaya Seeds into Your Diet?

6 Powerful Seeds That May Help Reduce Cancer Risk in Seniors – Eat Them Daily for Natural Support
Found these bumps on my son’s scalp. Doctor appt is so far away. What’s should I do? They look really painful

Can Wearable Devices Help Prevent Heart Disease?

A man with kidney failure collapsed in front of the toilet, his wife sobbing: "I advised him many times, but he wouldn't listen."
First Human Trial of Robotic-Assisted Cataract Surgery Reports No Treatment-Related Complications

Not All JAK Inhibitors Are the Same: Applying Evidence-Based Differences in Atopic Dermatitis Treatment
How daily showers after 65 can do more harm than good

A Common Refrigerator Mistake That Can Spread Bacteria and Make Your Whole Family Sick

Shoulder Pain from Sleeping: Causes, Solutions and More

Top Signs Your Body is Toxic and What to Do About It

How Water Fasting Can Regenerate the Immune System, Slow Aging, Reduce Heart Attack Risk and More
News Post

From Rising Living Costs to Sky-High Salaries: The Reality of Airline Pilot Pay

D.L. Hughley Says Nicki Minaj is 'Virtually Everything' Charlie Kirk Was 'Against'

Grammy winning Gospel star Richard Smallwood dies
“Beer Belly” Fat May Damage the Heart Differently Than General Obesity, Study Suggests

Mediterranean Diet Linked to Lower Risk of Multiple Sclerosis, Study Finds
Four Common Foods You Should Never Combine with Chicken: A Common Mistake That Can Harm Your Health

Divorce warning signs you might be ignoring

Don't use the 3 free things in motels and hotels

The 18 Best Low-Carb Vegetables to Eat on the Keto Diet

6 Tips for Recovering From a Sleepless Night

Tyler Perry Sued by Another Aspiring Actor Alleging Sexual Assault and Seeking $77 Million in Damages
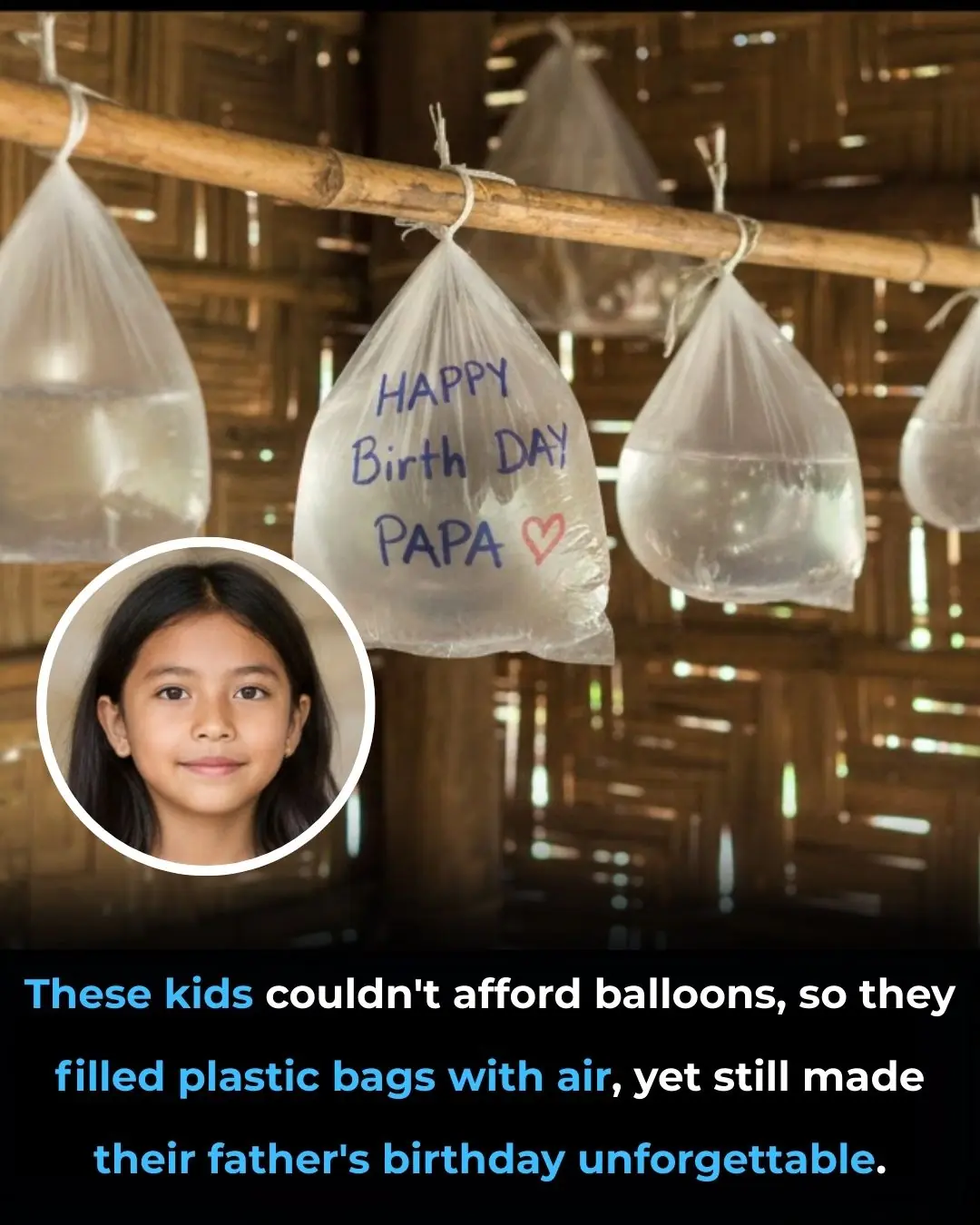
They Had No Money for Gifts—What They Did Instead Will Move You
Researchers Find Method to Trigger Retinal Repair Without Stem Cells

A Desperate Attempt: When a Driver Tried to Blame His Dog for Speeding
11 Ways to Break a Bad Habit

10 Benefits and uses of purslane
Banana Blossom: The Underrated Superfood Taking Over
Marty Supreme fans stunned after spotting viral homeless man in film 14 years after he became internet sensation

Experts issue warning for cancer symptom that can appear on pillows in the morning
