Shift Work Migraine Disorder: The Newly Proposed Headache Condition
Night shift work has long been associated with poor sleep and fatigue, but new research suggests its impact may go much deeper. A groundbreaking study has found that irregular or rotating shift schedules may dramatically increase the risk of debilitating migraines, prompting experts to call for the recognition of a brand-new medical condition: shift work migraine disorder.
Irregular Shifts Raise Migraine Risk by Over 60%
According to a systematic review and meta-analysis covering more than 51,000 participants across 20 studies, people working irregular or rotating shifts were 61% more likely to experience migraines compared to those on consistent schedules. The disruption of the circadian rhythm — the body’s internal clock that governs sleep-wake cycles — appears to play a critical role.
Although standard night shifts already strain the body, rotating schedules pose an even greater challenge. Frequent changes in work hours disrupt sleep cycles, interfere with recovery time, and create instability in diet and lifestyle patterns. This combination increases neurological stress and can trigger recurring migraines.
“Unlike migraines linked to hormones or frequency, those caused by irregular shifts are rooted in rotating schedules, inadequate recovery between shifts, exposure to intense lighting, and unstable eating habits,” explained Dr. Yohannes Woldeamanuel, lead author and assistant professor of neurology at the Mayo Clinic in Phoenix.
A Call for a New Migraine Subtype
Dr. Woldeamanuel and his team argue that migraines caused by shift work are distinct enough to deserve their own diagnostic category. Speaking at the American Headache Society’s 2025 Annual Meeting, he highlighted how circadian rhythm disturbances can alter activity in the hypothalamus and influence circadian genes, setting the stage for chronic headaches.
The proposed diagnostic term — “shift work migraine disorder” — would apply to patients who:
- Work irregular shifts for at least three months.
- Experience migraines or worsening symptoms within 24 hours of a schedule change.
- Show evidence of circadian rhythm disruption, such as erratic sleep or daytime fatigue.
- Have other medical causes for headaches ruled out.
This would separate the disorder from other well-established migraine types, such as menstrual or chronic migraine, by tying it to a specific environmental trigger: irregular shift work.
Gender Differences and Health Impact
The review also revealed striking gender differences. In studies involving nearly 29,000 participants, women working irregular shifts were more than twice as likely (OR: 2.48) as men to develop migraines. Researchers suspect that biological factors, hormonal influences, and lifestyle differences may contribute, but further studies are needed.
The implications are serious: migraines not only lower quality of life but also contribute to lost productivity, absenteeism, and higher healthcare costs. With millions of people worldwide engaged in rotating or night shift work, the public health burden could be substantial.
Reducing Migraine Risks for Shift Workers
While the debate on classification continues, experts agree that prevention strategies are essential. Recommendations include:
- Limiting consecutive night shifts to no more than three.
- Allowing at least 48 hours of recovery between shift rotations.
- Avoiding “quick returns,” or shifts spaced less than 11 hours apart.
- Designing forward-rotating schedules (morning → evening → night) instead of backward rotations.
- Using circadian tools, such as blue light filters, blackout curtains, or timed light exposure, to stabilize sleep cycles.
Small changes to workplace policies could make a major difference in protecting workers’ neurological health.
Debate Among Experts
Not all specialists agree that “shift work migraine disorder” deserves its own classification. Dr. Noah Rosen, a neurologist at Northwell Health in New York, expressed caution:
“The findings are intriguing, but they don’t yet prove a unique pain mechanism. Migraines related to irregular shifts may still fall under the broader umbrella of sleep-disruption migraines. More controlled studies, including sleep lab data, are needed before creating a new category.”
This divergence highlights the ongoing tension between evolving scientific discoveries and the need for rigorous evidence before rewriting medical classifications.
Looking Ahead
The study, funded by the National Institute of Neurological Disorders and Stroke, underscores the importance of considering work schedules as a serious health determinant. While debate continues over its official recognition, the research shines a spotlight on the neurological toll of modern labor demands and could pave the way for tailored treatments in the future.
For now, what is clear is that shift work does more than disrupt sleep — it may reshape brain function in ways that significantly increase the risk of migraines. Recognizing and addressing this could transform how both medicine and workplaces approach employee well-being.
News in the same category
How To Get Rid of Phlegm And Mucus

Hidden Clues Before the Tremor: Early Warning Signs of Parkinson’s Disease You Shouldn’t Ignore
Catching these subtle, non-motor clues may help identify Parkinson’s long before the motor stage, opening the door to interventions that could delay its full expression.

Gut Health in Early Pregnancy Tied to Gestational Diabetes Development
The study authors emphasize that these findings mark only the beginning.
Simple Homemade Cough Syrup Removes Phlegm From The Lungs

Eat this #1 meal to help unclog your arteries naturally

Canker Sores Are The Absolute WO:RST…Here’s How To Get Rid of Them Fast!

Cloves: 10 Health Benefits of Eating 2 Daily
How to Spot the Early Warning Signs of Cancer Growing in Your Body

New Research Finds 40-50% of Colon Cancer Cases Can Be Prevented by Doing These Simple Things

The Simple Trick to Get Rid of Ingrown Toenails Fast—You’ll Wish You Knew Sooner!

Statins warning: new research confirms these harmful side effects
5 Herbs Your Liver Wished You’d Start Eating More Often (Or At Least Try!)
If cancer is present, 3 key symptoms often appear in the morning

The Warning to People Who Regularly Walk Around Their Homes Barefoot

Foods That Add Inches to Your Waistline
Why the Neck Sags with Age: Causes, Solutions, and Prevention Tips

Top 3 Vitamins for Hip Arthritis

Anyone Who Wants to Avoid Having a Stroke Needs to Start Eating these 15 Foods Immediately
News Post
Donald Trump Says There Could Be People in Epstein Files Who ‘Don’t Deserve to Be’ There in Shocking Statement
Clean Your Kidneys and Urinary Tract Naturally: One Teaspoon a Day
Think Bottled Water Is Safer Think Again
A Surprising Drink That May Help Prevent Cancer – And It's Not Tea or Coffee
How To Get Rid of Phlegm And Mucus

5 Early Warning Signs of Cervical Cancer That 90% of Women Overlook
Cervical cancer is not a silent killer—it sends out warnings. The challenge is whether women notice and act on them in time.

8 Shocking Toilet Clues That Could Signal Cancer: Don’t Ignore These Early Warnings
Many people dismiss subtle changes in bathroom habits as minor or temporary issues. However, certain unusual signs when you go to the toilet could be early red flags of serious health problems. Recognizing them in time can make the difference between earl

3 Powerful Ways to Keep Snakes Out of Your Home and Protect Your Family
By combining natural repellents, careful use of traditional methods, and the protective instincts of pets, households can greatly reduce the likelihood of encountering these stealthy reptiles.

Study Reveals How Earth’s Orbit Triggers Ice Ages, And There’s One in The Next 11,000 Years

This 3,200-Year-Old Tree Is So Big, It’s Never Been Captured In A Single Photograph…

Hidden Clues Before the Tremor: Early Warning Signs of Parkinson’s Disease You Shouldn’t Ignore
Catching these subtle, non-motor clues may help identify Parkinson’s long before the motor stage, opening the door to interventions that could delay its full expression.
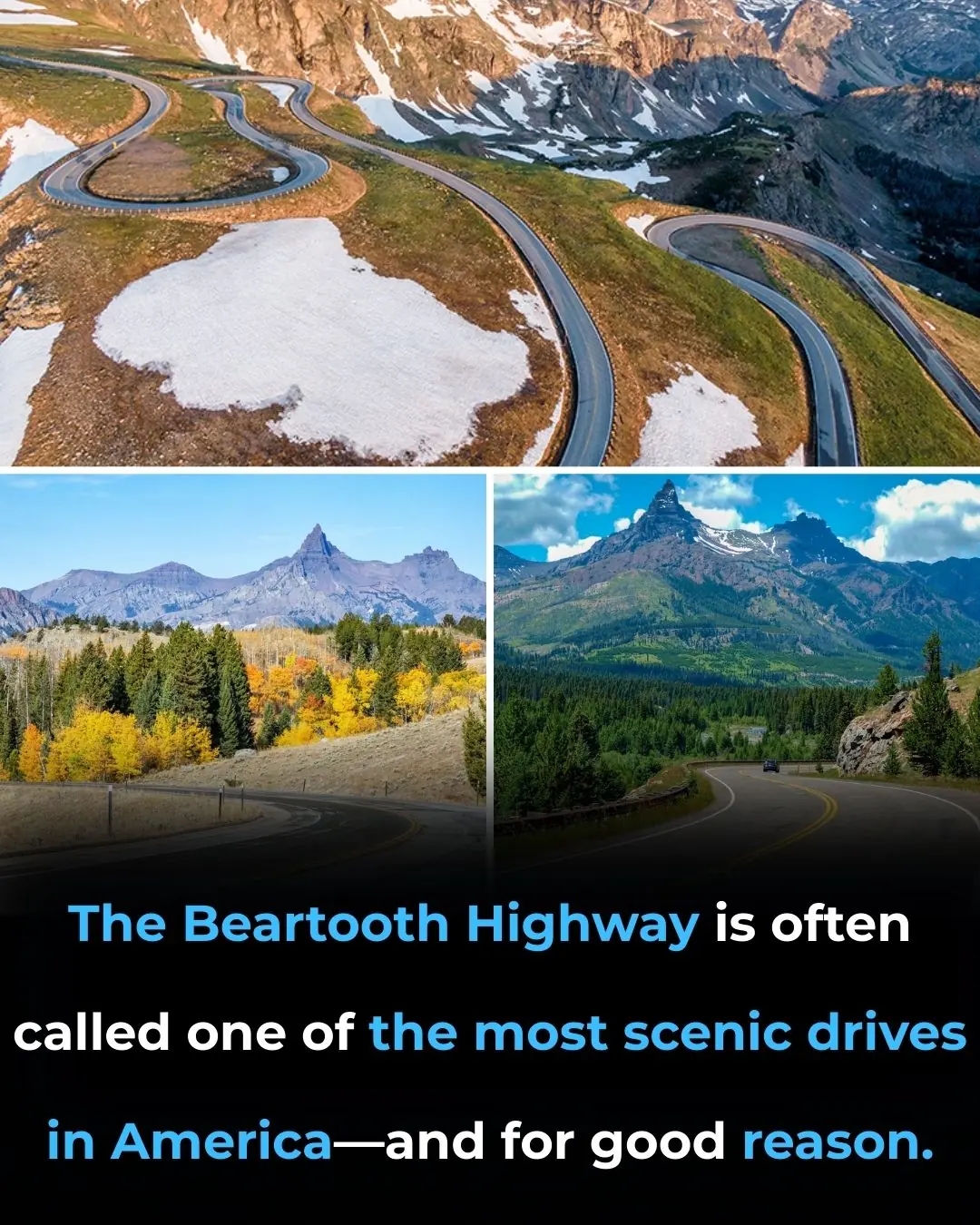
Travel Coast-to-Coast by Train and See America’s Greatest Sites For Just Over $200

Gut Health in Early Pregnancy Tied to Gestational Diabetes Development
The study authors emphasize that these findings mark only the beginning.
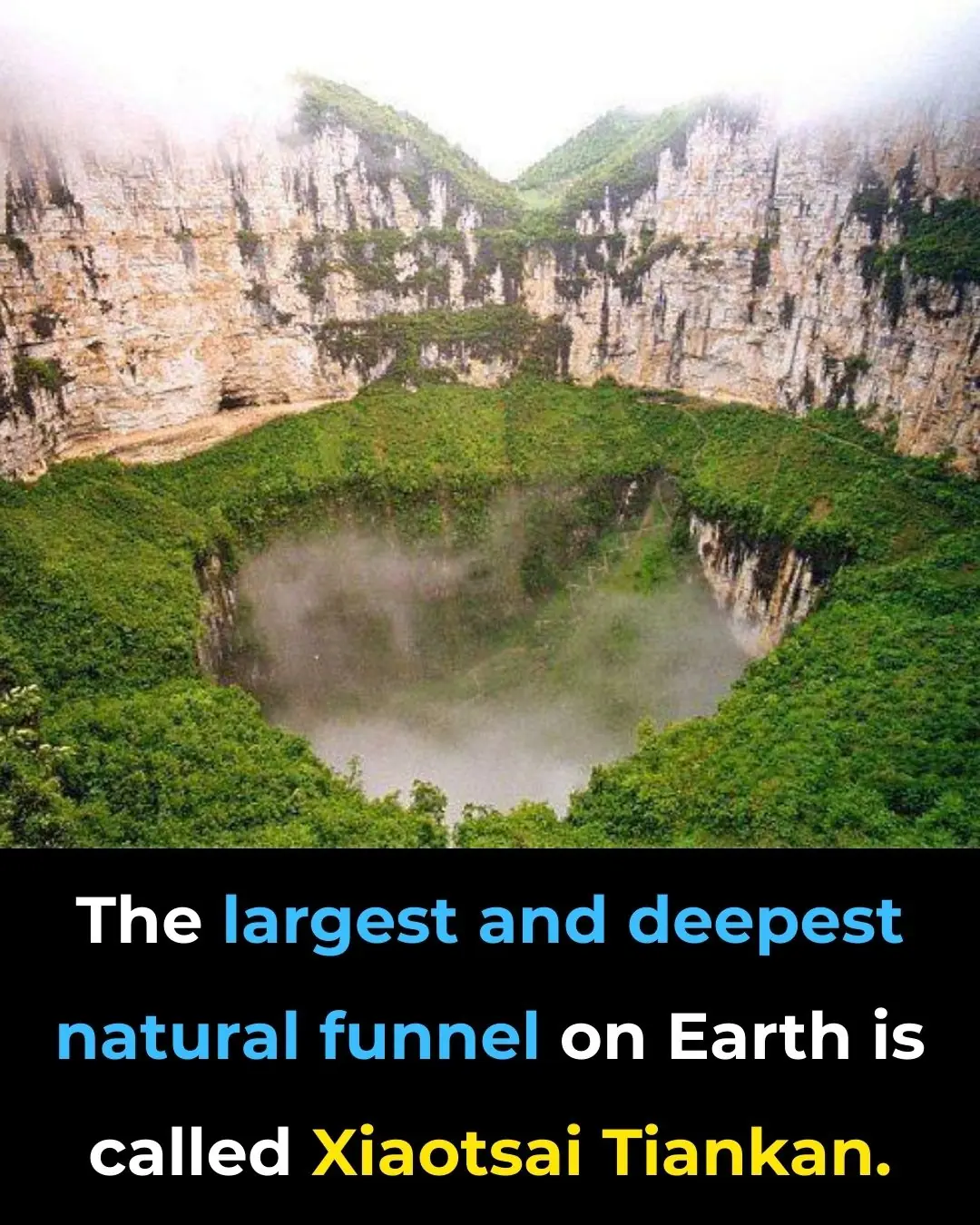
Descend Into the Heavenly Pit: Exploring Xiaozhai Tiankeng, the World’s Deepest Sinkhole

The Walking Trees of Ecuador: They Reportedly Move Up to 20 Meters Per Year

How to See Halos, Sun Dogs and Other Delights of the Daytime Sky
Save this valuable remedy that helps de:toxify and can save the life of someone bitten by a ra:bid d:og or snake in just 1 minute.
The method to drive away an entire rat colony using just a handful of rice, without the need for harmful poisons.