
Why D-Dimer Testing Alone May Miss Pulmonary Embolism in Pregnancy

Pulmonary embolism (PE) is one of the leading causes of maternal morbidity and mortality worldwide, yet it remains a diagnostic challenge during pregnancy. Symptoms such as leg swelling, chest pain, or sudden shortness of breath are often attributed to normal physiological changes of pregnancy, potentially delaying life-saving evaluation and treatment. Emerging evidence suggests that relying solely on D-dimer testing may fail to detect the full spectrum of thromboembolic risk in pregnant and postpartum women.
Pregnancy and Thromboembolism: A High-Risk State
Pregnancy is a naturally hypercoagulable state. According to the American College of Obstetricians and Gynecologists (ACOG), pregnant women and those in the postpartum period carry a four- to fivefold higher risk of thromboembolism compared with nonpregnant women. Approximately 80% of these events are venous, including deep vein thrombosis (DVT) and pulmonary embolism.
This increased risk is driven by several physiological changes:
-
Elevated clotting factors to prevent excessive bleeding during childbirth
-
Reduced fibrinolytic activity
-
Venous stasis caused by uterine compression of pelvic veins
-
Endothelial injury during delivery
While these changes are protective during labor, they significantly increase the likelihood of venous thromboembolism (VTE).
The Diagnostic Challenge of Pulmonary Embolism in Pregnancy
Diagnosing PE during pregnancy is particularly difficult because symptoms overlap with normal pregnancy-related discomforts. Dyspnea, tachycardia, mild leg swelling, and fatigue are common during pregnancy, often leading clinicians to underestimate the severity of symptoms.
Traditional diagnostic tools used in nonpregnant patients may not perform the same way during pregnancy. Among these tools, D-dimer testing—widely used to rule out PE in low-risk individuals—has significant limitations in pregnant populations.
Why D-Dimer Alone Is Not Enough
D-dimer is a fibrin degradation product that rises when blood clots are formed and broken down. In nonpregnant patients, a normal D-dimer level can reliably exclude PE in low-risk cases. However, during pregnancy, D-dimer levels naturally increase with gestational age, even in healthy women without thrombosis.
This physiological elevation reduces the specificity of the test and increases the likelihood of false-positive results. Conversely, normal or borderline D-dimer values may provide false reassurance, potentially delaying further diagnostic evaluation in women who actually have PE.
Recent studies and expert guidance highlight that D-dimer testing alone may miss clinically significant thromboembolism, particularly in women with atypical presentations or underlying risk factors.
A More Comprehensive Diagnostic Approach
Current best practices emphasize that D-dimer testing should not be used in isolation. Instead, clinicians are encouraged to adopt a multimodal diagnostic strategy, which may include:
-
Careful clinical risk assessment
-
Consideration of pregnancy-adapted clinical prediction rules
-
Compression ultrasound for suspected DVT
-
Imaging studies such as ventilation-perfusion (V/Q) scanning or computed tomography pulmonary angiography (CTPA) when indicated
While concerns about radiation exposure exist, modern imaging techniques deliver relatively low fetal radiation doses, and the risk of missing a potentially fatal PE far outweighs the theoretical radiation risk.
Postpartum Risk: An Often Overlooked Period
The risk of thromboembolism does not end with delivery. The postpartum period, especially the first six weeks after childbirth, carries the highest risk for PE. Surgical delivery, prolonged immobility, infection, and hemorrhage further increase thrombotic risk.
Clinicians must maintain a high index of suspicion during this period, particularly when women present with sudden respiratory symptoms or unilateral leg swelling.
Improving Awareness and Clinical Outcomes
Pulmonary embolism in pregnancy is both preventable and treatable when identified early. Greater awareness among clinicians, combined with updated diagnostic pathways, can significantly reduce maternal morbidity and mortality.
Key takeaways include:
-
Pregnancy significantly increases the risk of venous thromboembolism
-
Symptoms of PE may mimic normal pregnancy changes
-
D-dimer testing alone is insufficient and may be misleading
-
A structured diagnostic approach improves safety and accuracy
Conclusion
Pulmonary embolism remains a silent and dangerous threat during pregnancy and the postpartum period. While D-dimer testing plays a role in VTE evaluation, it should never be the sole determinant in pregnant patients. Prompt recognition, comprehensive assessment, and appropriate imaging when necessary are critical to saving lives.
As evidence continues to evolve, clinicians must adapt diagnostic strategies to the unique physiological realities of pregnancy—ensuring that life-threatening thromboembolic events are neither overlooked nor underestimated.
News in the same category

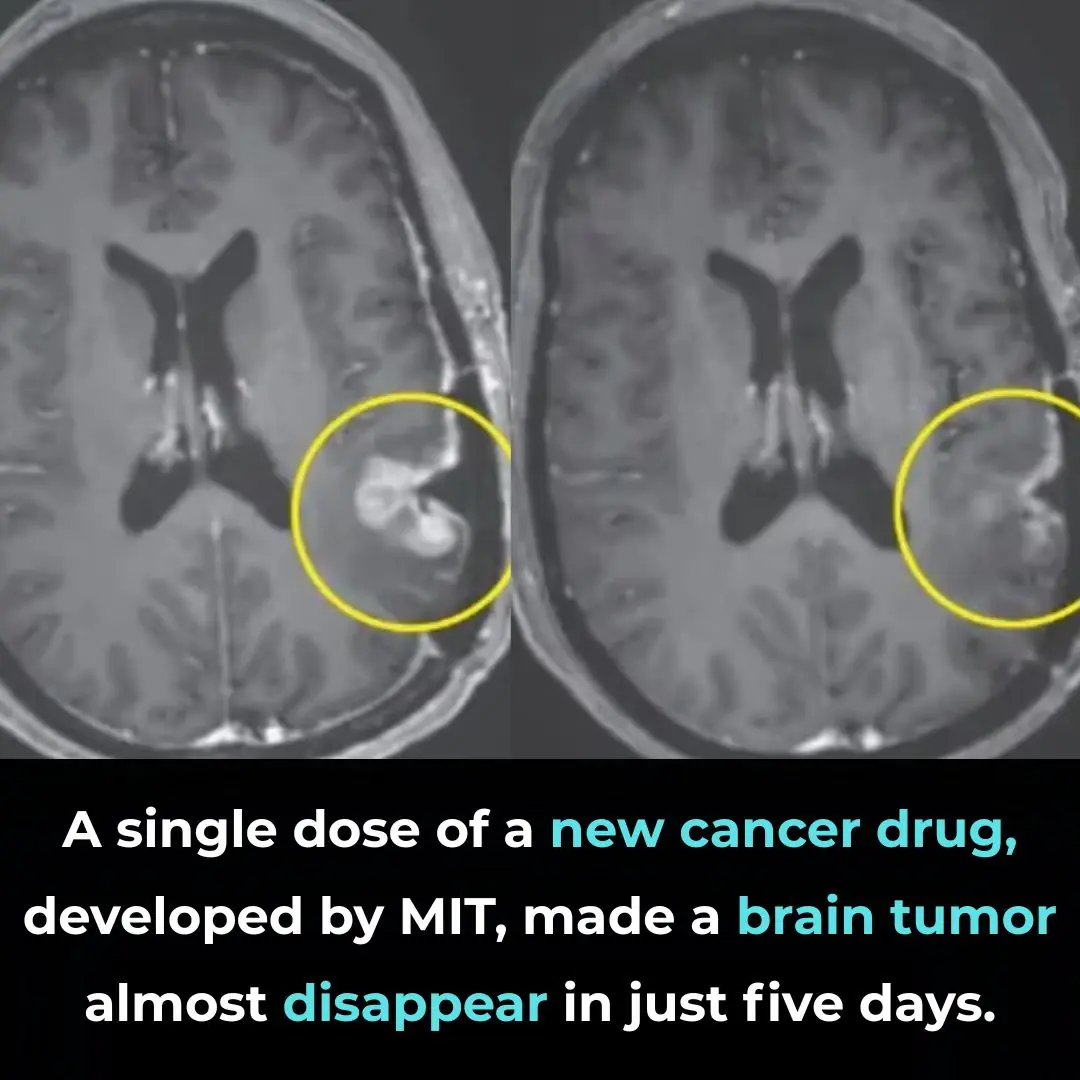
A Breakthrough in Glioblastoma Immunotherapy: Rapid Tumor Regression with CARv3-TEAM-E

Pomegranate Seed Oil Supplementation and Cognitive Improvement in Mild Cognitive Impairment

Selective Anti-Cancer Effects of Frankincense: Evidence from Laboratory Studies

Kimchi Consumption and Immune Balance: Evidence from a 12-Week Human Clinical Study
Selective Anti-Cancer Activity of Dandelion Root Extract in Colorectal Cancer
Inducing Lethal Autophagy in Glioblastoma Through Drug Repurposing

mRNA Flu Vaccines Show Higher Effectiveness Than Traditional Quadrivalent Shots, Phase 3 Trial Finds
Early Signs of Multiple Sclerosis

11 Benefits of Going Caffeine-Free

5 Early Signs of Cervical Cancer That Are Often Ignored: 90% of Women Overlook Them

The Cheap Drink That Can Help Prevent Stroke, Reduce Blood Fat, and Fight Cancer

8 Signs You’re Eating Too Much Sugar

Accidental discovery of bone-eroding cancer after a fall: It turns out the body had been crying for help for a long time but was ignored
10 Eye Symptoms to Watch Out For

Does Eating Bananas Before Bed Have Any Benefits?
Can’t Fall Back Asleep After Waking Up to Use the Bathroom? Try These 5 Hacks

What Is Preventive Botox (or ‘Baby Botox’) — and Is It Safe?
News Post
10 Simple Ways to Help Your Body Detoxify and Cleanse Itself

The butcher's mysterious handkerchief: What are they wiping?

After buying a lot of clams, an experienced fisherman with 10 years of experience shares this trick: clean the clams in 5 minutes without any fuss.
Some people blanch ribs in water, others braise them directly, but the chef says: Both are wrong; few people know the correct way.

Add a few drops of this, and the fried eggs will puff up to twice their size, become fluffy and smooth, and have no fishy smell.

Homemade Okra Face Gel – Collagen Gel for Glowing Skin

Teeth Whitening – Natural Home Remedies

DIY Collagen Powder Recipe for Glowing Skin & Thick Hair

“mom, i have a fever… can i stay home from school today?” the girl said. her mother touched her forehead and allowed her to stay.

I heard voices in our bedroom and hid in the closet. My husband walked in with her, holding papers. She whispered, ‘What’s your plan?’ He laughed, ‘2 million when she dies. Accident on the stairs. I’ve already made her…

MY HUSBAND HAD PROMISED ME A BIG SURPRISE FOR OUR 55TH CHRISTMAS TOGETHER—BUT HE PASSED AWAY TWO MONTHS BEFORE.

My husband sent me to prison for 2 years over his mistress’s miscarriage. Every month they came to visit me, but I always refused to see them. The day of my release will also be the day they lose everything.

I ran to see my husband in the operating room. Suddenly, a nurse whispered to me: “Quick, ma’am, hide and trust me! It’s a trap!” And 10 minutes later… I froze when I saw him. It turns out that he…

My son and his wife locked my husband and me in the basement of our house. While I panicked, my husband whispered: ‘Quiet… they don’t know what is behind this wall.’ When they left, my husband moved a brick and showed me a secret he had kept hidde

Don’t Soak Frozen Meat in Cold Water: A Chef’s 5-Minute Thawing Trick That Keeps Meat Tasty and Nutritious
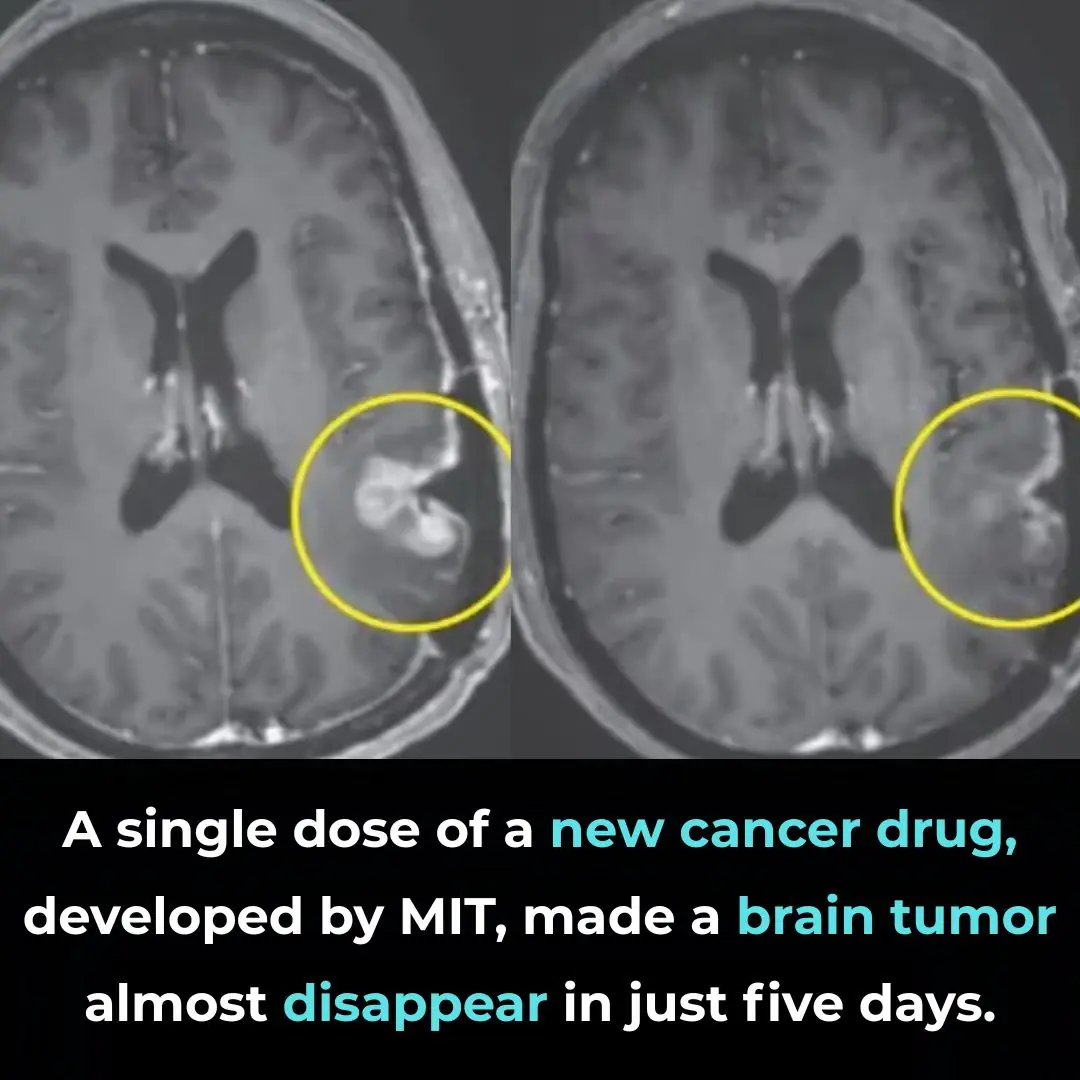
A Breakthrough in Glioblastoma Immunotherapy: Rapid Tumor Regression with CARv3-TEAM-E

Pomegranate Seed Oil Supplementation and Cognitive Improvement in Mild Cognitive Impairment

Selective Anti-Cancer Effects of Frankincense: Evidence from Laboratory Studies
