Are You Using New Tools to Support Patients With DD-CKD Anemia?
Understanding the Role of HIF-PHIs, Current Evidence, and Strategies to Close Gaps in Care
Anemia is one of the most common and clinically significant complications of dialysis-dependent chronic kidney disease (DD-CKD). Despite advances in nephrology care, anemia management in this population remains complex and suboptimal for many patients. Traditional treatment approaches—primarily erythropoiesis-stimulating agents (ESAs) and iron supplementation—have improved outcomes but are associated with important limitations. As a result, new therapeutic strategies are emerging to address persistent gaps in care. Among the most promising are hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs).
This continuing medical education (CME) overview explores the evolving role of HIF-PHIs, reviews current clinical evidence, and outlines practical approaches to improving anemia management in patients with DD-CKD.
The Burden of Anemia in Dialysis-Dependent CKD
Anemia in CKD is driven primarily by reduced erythropoietin production, iron deficiency, chronic inflammation, and shortened red blood cell survival. In patients receiving dialysis, anemia is often more severe and difficult to control, contributing to fatigue, reduced quality of life, increased cardiovascular risk, and higher rates of hospitalization and mortality.
While ESAs have been the cornerstone of therapy for decades, many patients experience ESA hyporesponsiveness, fluctuating hemoglobin levels, or require high doses that may increase cardiovascular risk. These challenges underscore the need for alternative or complementary treatment options.
HIF-PHIs: A New Mechanism for Anemia Management
HIF-PHIs represent a novel class of oral agents that target the body’s natural oxygen-sensing pathway. By inhibiting prolyl hydroxylase enzymes, these drugs stabilize hypoxia-inducible factor (HIF), leading to increased endogenous erythropoietin production and improved iron metabolism.
Unlike traditional ESAs, which deliver supraphysiologic erythropoietin levels, HIF-PHIs stimulate a more physiologic response. They enhance iron absorption, reduce hepcidin levels, and promote efficient utilization of iron stores—key advantages in patients with inflammation-driven functional iron deficiency.
Current Evidence Supporting HIF-PHIs in DD-CKD
Clinical trials have demonstrated that HIF-PHIs are effective in increasing and maintaining hemoglobin levels in patients with dialysis-dependent CKD. Studies comparing HIF-PHIs with ESAs have shown comparable efficacy in hemoglobin control, with some evidence suggesting more stable hemoglobin levels over time.
Additionally, HIF-PHIs have been associated with improved iron parameters and reduced need for intravenous iron in certain patient populations. Ongoing research continues to evaluate long-term cardiovascular safety, thromboembolic risk, and other outcomes critical to dialysis patients.
Addressing Gaps in Current Anemia Management
Despite available therapies, gaps in anemia care persist. These include delayed treatment initiation, inconsistent hemoglobin monitoring, inadequate iron assessment, and limited individualized treatment strategies. Integrating HIF-PHIs into clinical practice may help address some of these challenges, particularly for patients who are ESA-hyporesponsive or struggle with iron management.
However, successful adoption requires clinician education, careful patient selection, and an understanding of how these agents fit within existing treatment algorithms. Shared decision-making and close monitoring remain essential to optimize outcomes and minimize risk.
Practical Considerations for Clinicians
When considering HIF-PHIs for patients with DD-CKD anemia, clinicians should evaluate baseline iron status, inflammation markers, cardiovascular risk, and dialysis modality. Monitoring hemoglobin trends, iron parameters, and potential adverse effects is critical, particularly during treatment initiation and dose adjustments.
As with any emerging therapy, staying informed about evolving guidelines, regulatory approvals, and post-marketing safety data is essential. CME programs play a key role in equipping healthcare professionals with the knowledge needed to confidently integrate new tools into practice.
Conclusion
Anemia management in dialysis-dependent CKD is entering a new era. HIF-PHIs offer a promising alternative to traditional therapies by addressing both erythropoietin deficiency and disordered iron metabolism through a more physiologic mechanism. While challenges remain, these agents have the potential to close long-standing gaps in care and improve outcomes for patients with DD-CKD anemia.
Ongoing education, evidence-based decision-making, and individualized treatment strategies will be crucial as clinicians incorporate these new tools into comprehensive anemia management plans.
News in the same category

Sugary Soft Drinks, Gut Bacteria, and Depression: How What You Drink May Shape Mental Health

Drug Shortages in the United States Are Forcing Major Changes in Primary Care Practice

Five Reasons to Eat One Banana a Day: A Simple Habit for Better Health and Longevity

Three Simple Ways to Use White Radish to Reduce Phlegm, Relieve Cough, and Support Lung Health
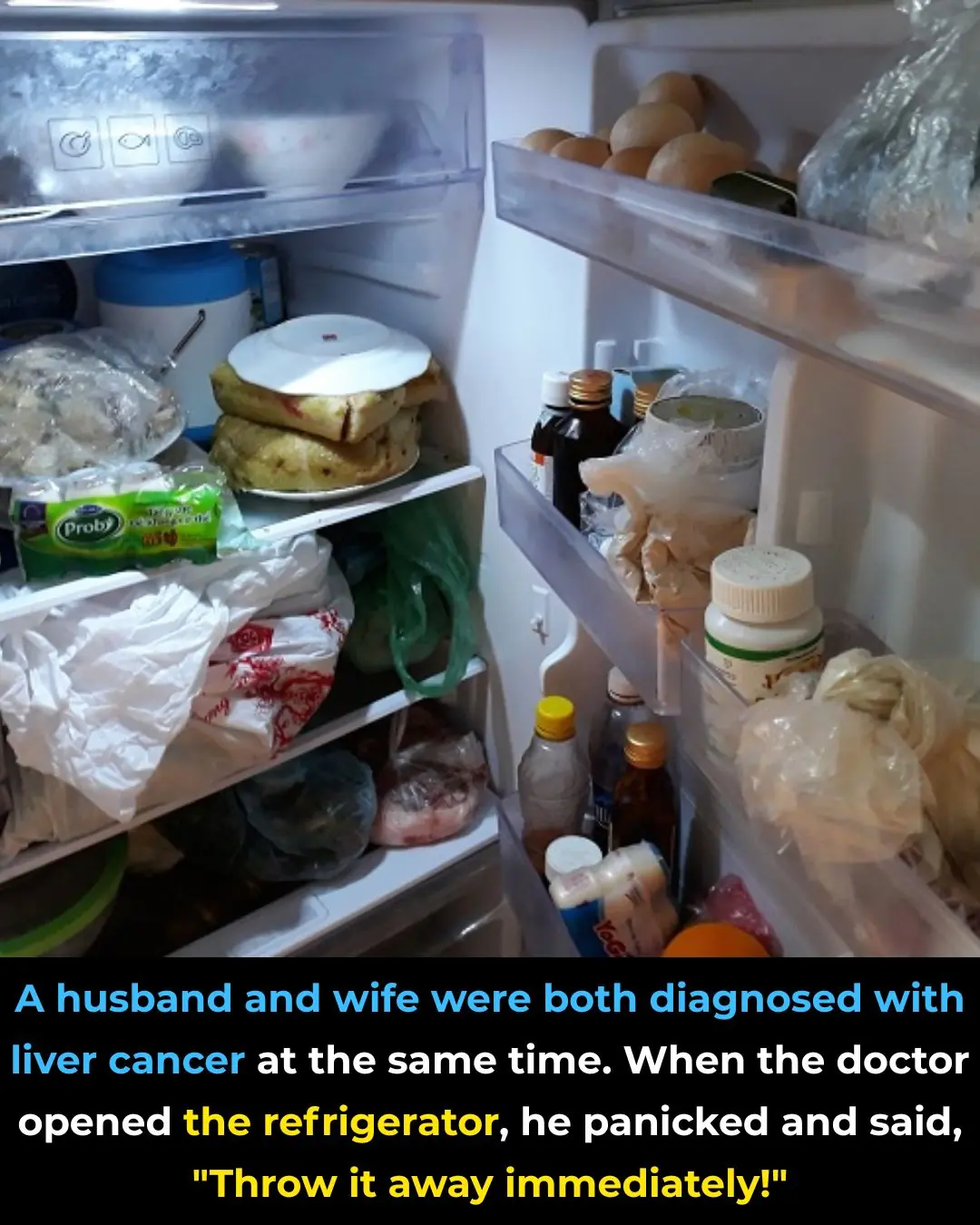
A Couple Diagnosed With Liver Cancer at the Same Time: Doctors Urgently Warn After Opening Their Refrigerator
🌙 If You Notice These 3 Signs at Night, Your Kidneys Are Likely in Great Shape
Diagnosed with terminal cancer that had metastasized to the brain, the woman went for a check-up and burst into tears upon learning that her husband and son were the culprits

Doctors warn: 4 types of inflammation can easily turn into cancer in just one year if treatment is delayed
Triple Therapy Linked to Lower Lung Clearance Index in Children With Cystic Fibrosis

Drink Water First: Hydration on Waking May Sharpen the Brain More Than Your Morning Coffee
Nobel-Winning Discovery Reveals How to Stop the Immune System From Attacking the Body

Why Sugar Matters More Than Cholesterol in Heart Disease Risk

Single-Injection Gene Therapy Restores Vision in Patients With Inherited Blindness
Smelly but Smart? Weird Study Claims Your Own Gas Could Benefit Brain Health
Vitamin K2 Supplementation Slows Arterial Plaque Progression in Chronic Kidney Disease

Everyone Fears Diabetes, but Diabetes “Fears” These 5 Foods

A Hard-Earned Lesson for Middle-Aged Parents: Let Go of These Habits, and Your Children Will Naturally Grow Closer
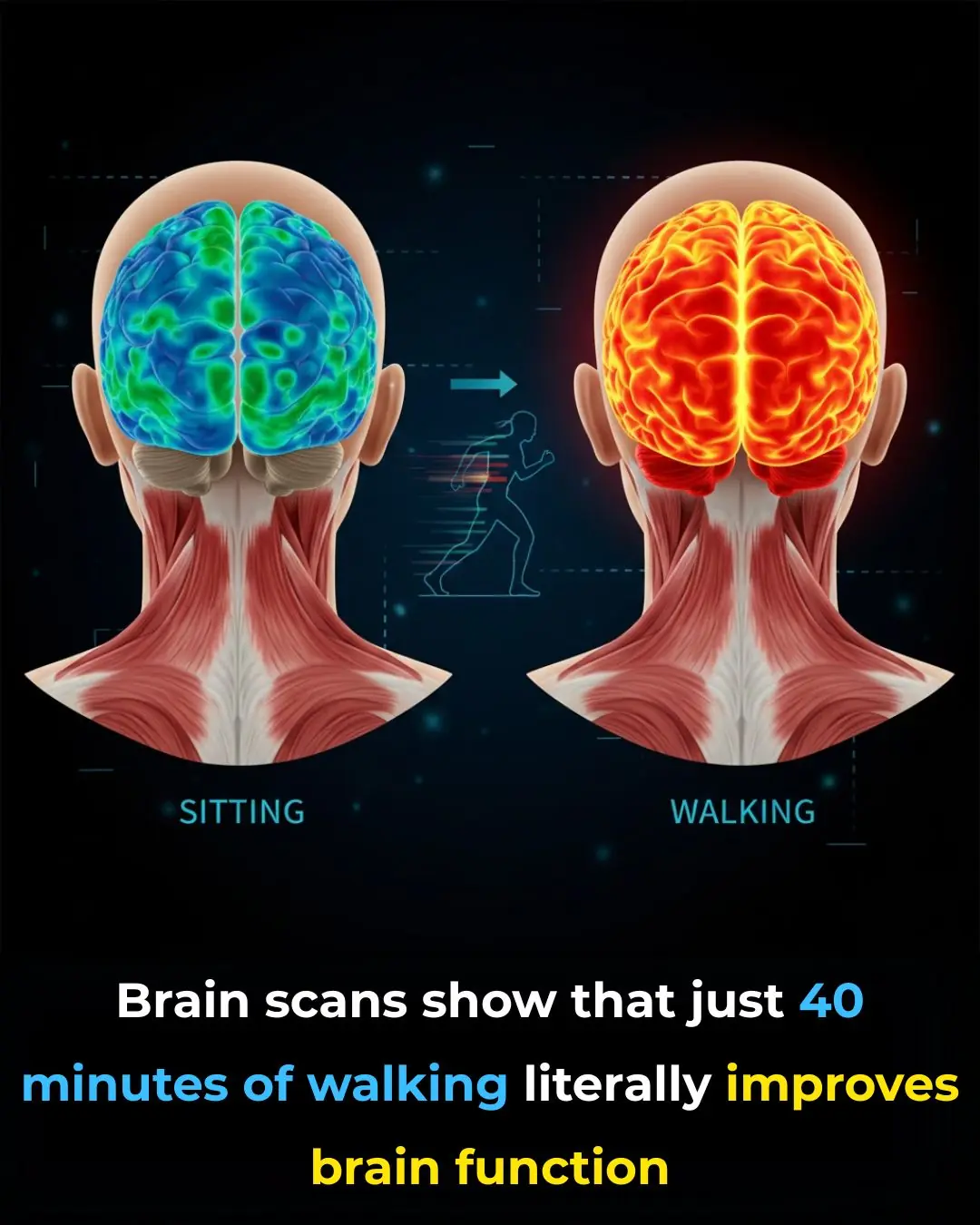
How Walking Activates the Brain: The Hidden Link Between Movement, Focus, and Mental Clarity
News Post
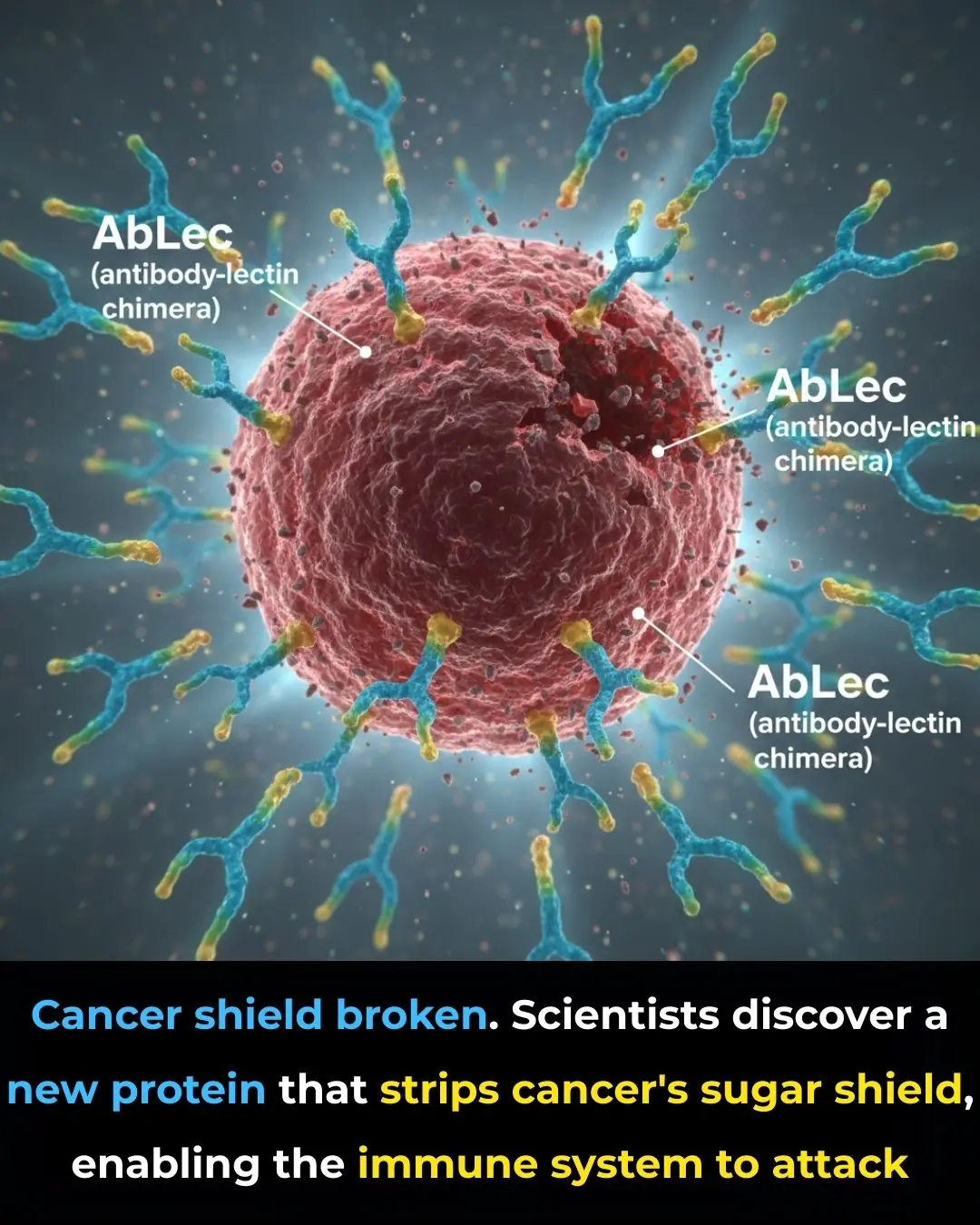
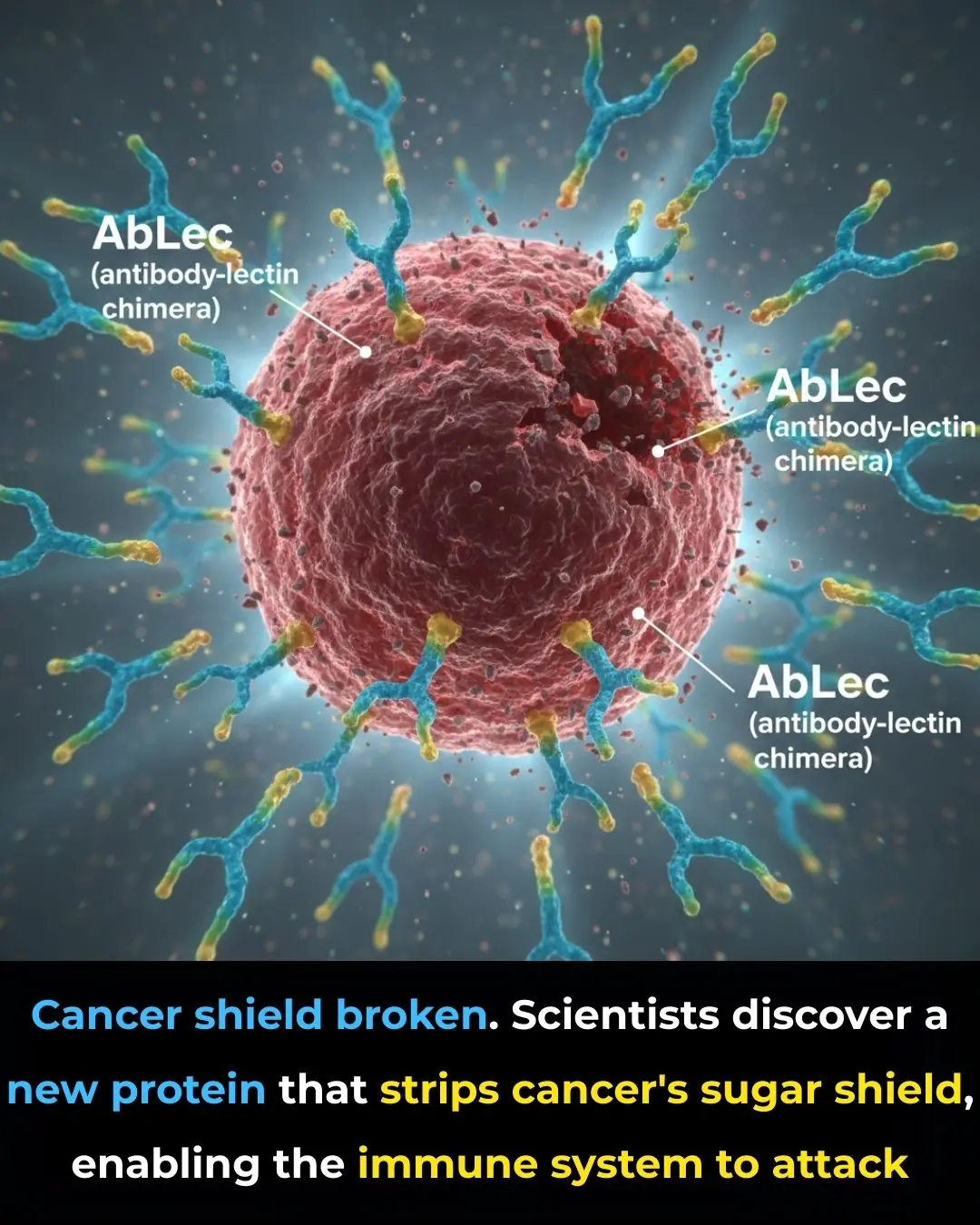
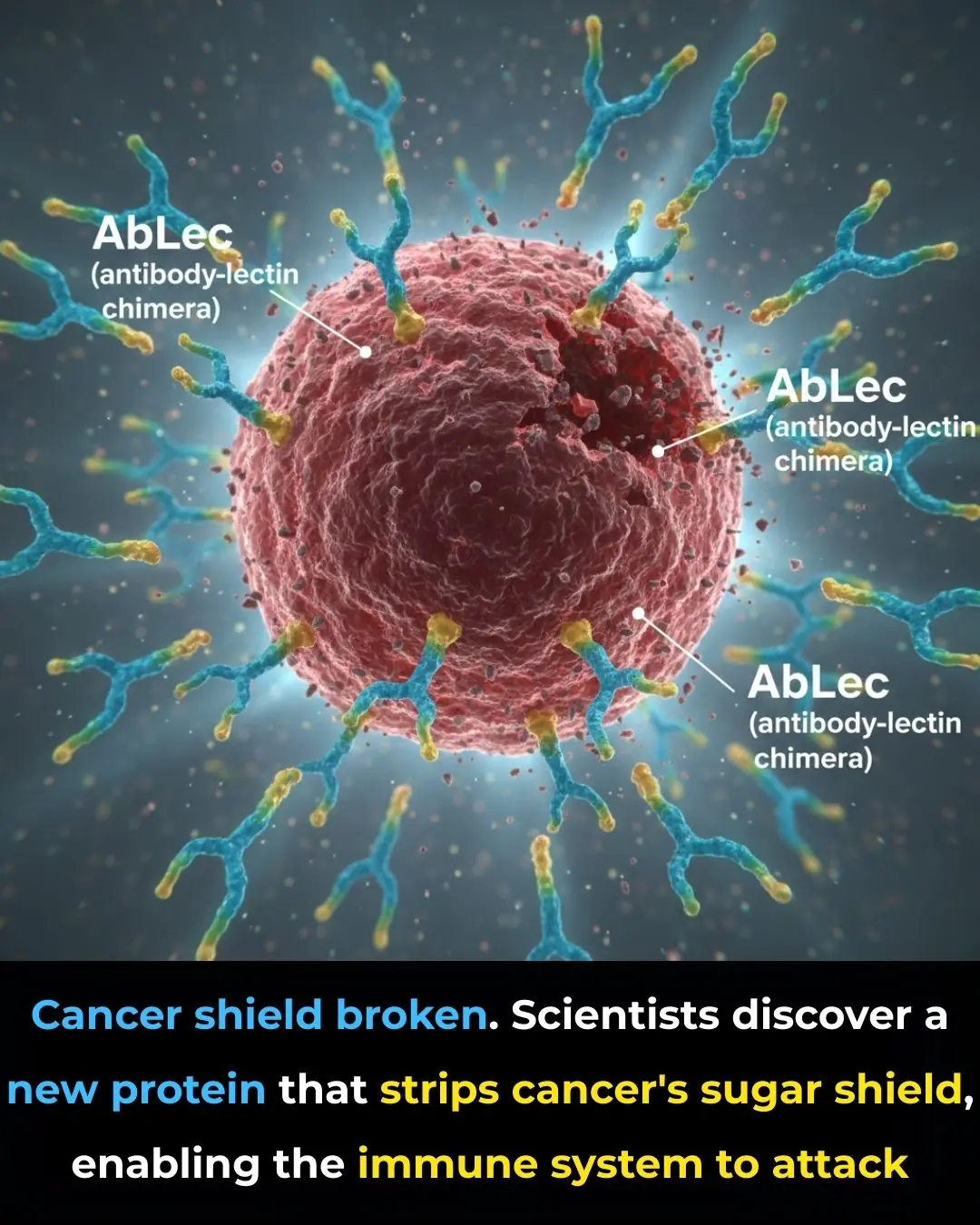
New Protein Breakthrough Unmasks Cancer Cells, Boosting the Power of Immunotherapy

Sugary Soft Drinks, Gut Bacteria, and Depression: How What You Drink May Shape Mental Health

Exploring the Traditional Uses and Potential Wellness Benefits of Prickly Lettuce Leaves (Lactuca serriola)

Pumpkin Seeds for Health: Natural Remedies, Recipes, and Benefits
11 Benefits of Dandelion Roots
7 Essential Leaves to Naturally Improve Your Eye Health

Drug Shortages in the United States Are Forcing Major Changes in Primary Care Practice

Five Reasons to Eat One Banana a Day: A Simple Habit for Better Health and Longevity

Three Simple Ways to Use White Radish to Reduce Phlegm, Relieve Cough, and Support Lung Health
Dreaming of Deceased Loved Ones: Is It a Good or Bad Sign?
A Couple Diagnosed With Liver Cancer at the Same Time: Doctors Urgently Warn After Opening Their Refrigerator

11 dishes you should never cook in an air fryer; don't try it or you'll regret it.

Put Bay Leaves in the Corners of Their Kitchen

The Simple Nighttime Habit That Can Help You Fall Asleep Faster
🌙 If You Notice These 3 Signs at Night, Your Kidneys Are Likely in Great Shape
Diagnosed with terminal cancer that had metastasized to the brain, the woman went for a check-up and burst into tears upon learning that her husband and son were the culprits

Doctors warn: 4 types of inflammation can easily turn into cancer in just one year if treatment is delayed
Why Some People Rub Onions on Their Windows
