Drug Shortages in the United States Are Forcing Major Changes in Primary Care Practice

Drug shortages across the United States have reached a critical level, placing increasing strain on primary care clinicians and reshaping the way they deliver care. According to data from a recent national survey of nearly 900 healthcare professionals, 87% of clinicians reported having to modify their clinical practice as a direct result of ongoing medication shortages. These findings highlight not only the scale of the problem, but also its profound impact on patient care, clinician workload, and the overall healthcare system.
A Widespread and Persistent Problem
Medication shortages are no longer isolated or temporary disruptions. Over the past several years, shortages have affected a wide range of commonly prescribed drugs, including antibiotics, diabetes medications, cardiovascular agents, pain relievers, and emergency medications. Many of these drugs are essential first-line therapies, leaving clinicians with limited or less effective alternatives.
Survey respondents indicated that shortages are occurring more frequently and lasting longer than in previous years. As a result, clinicians are often forced to make real-time decisions with incomplete information, uncertain supply timelines, and limited therapeutic options.
How Clinicians Are Adapting Their Practice
The survey revealed that nearly nine out of ten clinicians have had to change how they practice medicine due to drug shortages. These changes take many forms. Physicians and nurse practitioners report switching patients to second- or third-line medications, adjusting dosages, delaying treatment, or splitting available supplies among patients. In some cases, clinicians must spend additional time searching for available medications across pharmacies or coordinating with hospitals and suppliers.
These adaptations are not without consequences. Alternative medications may be less effective, carry different side-effect profiles, or be more expensive for patients. Clinicians also expressed concern that frequent medication changes can confuse patients, reduce adherence, and undermine trust in treatment plans.
Increased Burden on Primary Care
Primary care settings appear to be particularly vulnerable to the effects of drug shortages. Unlike large hospital systems, many primary care practices lack dedicated pharmacy teams or supply chain support. Clinicians themselves must often manage the logistical challenges associated with shortages, adding to already heavy workloads.
Respondents reported spending significant time on administrative tasks related to shortages, such as contacting pharmacies, rewriting prescriptions, and counseling patients about medication changes. This additional burden contributes to clinician frustration and burnout, which are already major concerns in primary care.
Impact on Patient Safety and Quality of Care
Drug shortages raise serious concerns about patient safety. When first-choice therapies are unavailable, clinicians may be forced to use less familiar medications, increasing the risk of dosing errors or adverse drug reactions. Delays in treatment can also worsen disease outcomes, particularly for patients with chronic conditions such as diabetes, hypertension, or cardiovascular disease.
Many clinicians surveyed expressed worry that shortages disproportionately affect vulnerable populations, including older adults, low-income patients, and those with limited access to healthcare resources. Higher out-of-pocket costs for alternative medications can further widen existing health disparities.
Calls for System-Level Solutions
The survey findings underscore the urgent need for systemic solutions to address drug shortages. Clinicians emphasized the importance of improved transparency around drug supply disruptions, earlier notification of impending shortages, and stronger coordination between manufacturers, regulators, and healthcare providers.
Policy experts have also called for increased domestic drug manufacturing, diversification of supply chains, and incentives to produce low-profit but essential generic medications. Without meaningful reform, clinicians warn that shortages will continue to compromise care quality and place unsustainable pressure on the healthcare workforce.
Conclusion
The fact that 87% of clinicians are changing their practice due to drug shortages is a clear signal that the problem has moved beyond inconvenience and into the realm of patient safety and healthcare sustainability. As shortages persist, primary care clinicians are being asked to do more with less—often at the expense of time, resources, and emotional well-being. Addressing this crisis will require coordinated action at the national level to ensure reliable access to essential medications and protect the integrity of patient care.
News in the same category

Sugary Soft Drinks, Gut Bacteria, and Depression: How What You Drink May Shape Mental Health

Five Reasons to Eat One Banana a Day: A Simple Habit for Better Health and Longevity

Three Simple Ways to Use White Radish to Reduce Phlegm, Relieve Cough, and Support Lung Health
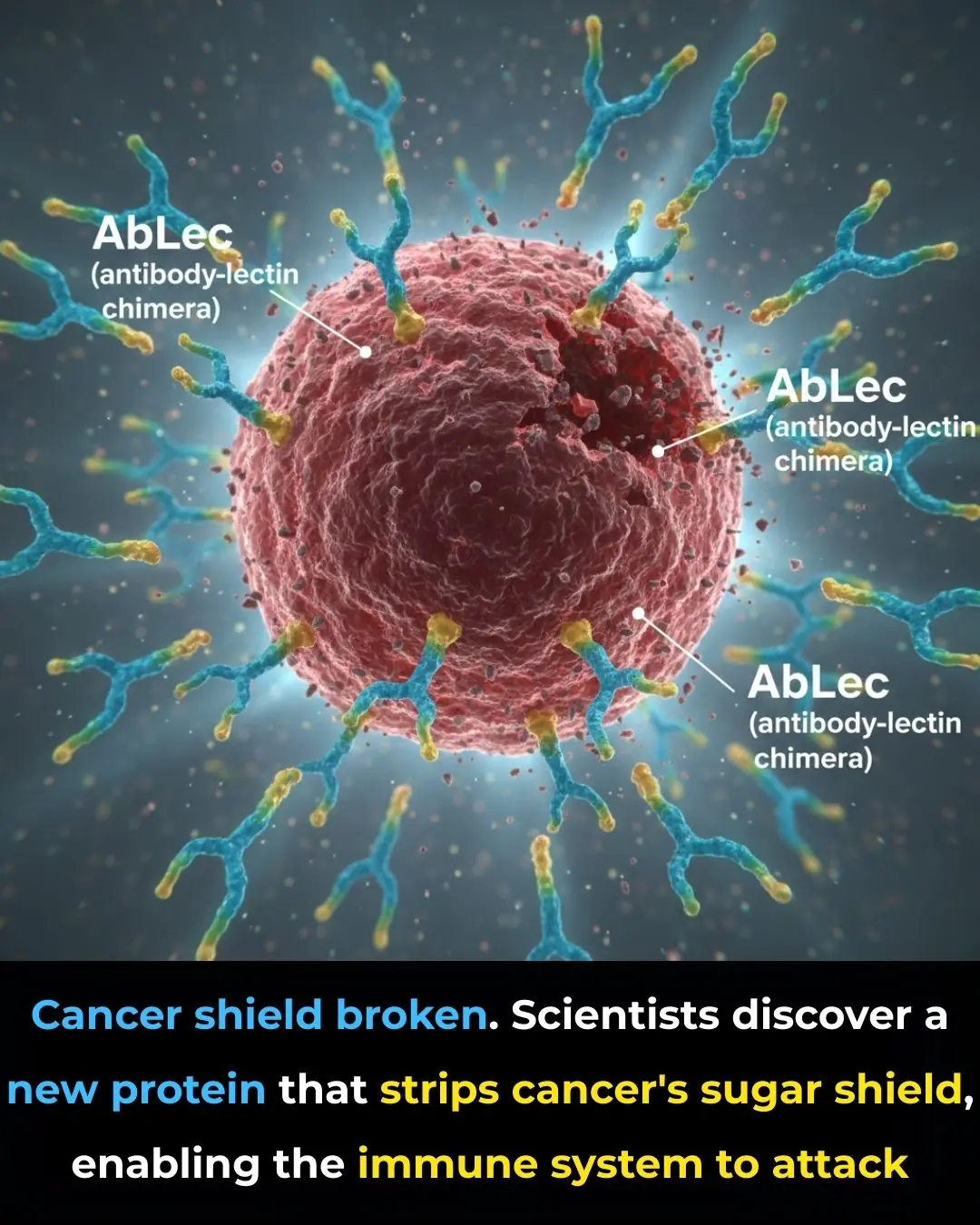
A Couple Diagnosed With Liver Cancer at the Same Time: Doctors Urgently Warn After Opening Their Refrigerator
🌙 If You Notice These 3 Signs at Night, Your Kidneys Are Likely in Great Shape
Diagnosed with terminal cancer that had metastasized to the brain, the woman went for a check-up and burst into tears upon learning that her husband and son were the culprits

Doctors warn: 4 types of inflammation can easily turn into cancer in just one year if treatment is delayed
Triple Therapy Linked to Lower Lung Clearance Index in Children With Cystic Fibrosis

Drink Water First: Hydration on Waking May Sharpen the Brain More Than Your Morning Coffee
Nobel-Winning Discovery Reveals How to Stop the Immune System From Attacking the Body

Why Sugar Matters More Than Cholesterol in Heart Disease Risk

Single-Injection Gene Therapy Restores Vision in Patients With Inherited Blindness
Smelly but Smart? Weird Study Claims Your Own Gas Could Benefit Brain Health
Vitamin K2 Supplementation Slows Arterial Plaque Progression in Chronic Kidney Disease

Everyone Fears Diabetes, but Diabetes “Fears” These 5 Foods

A Hard-Earned Lesson for Middle-Aged Parents: Let Go of These Habits, and Your Children Will Naturally Grow Closer
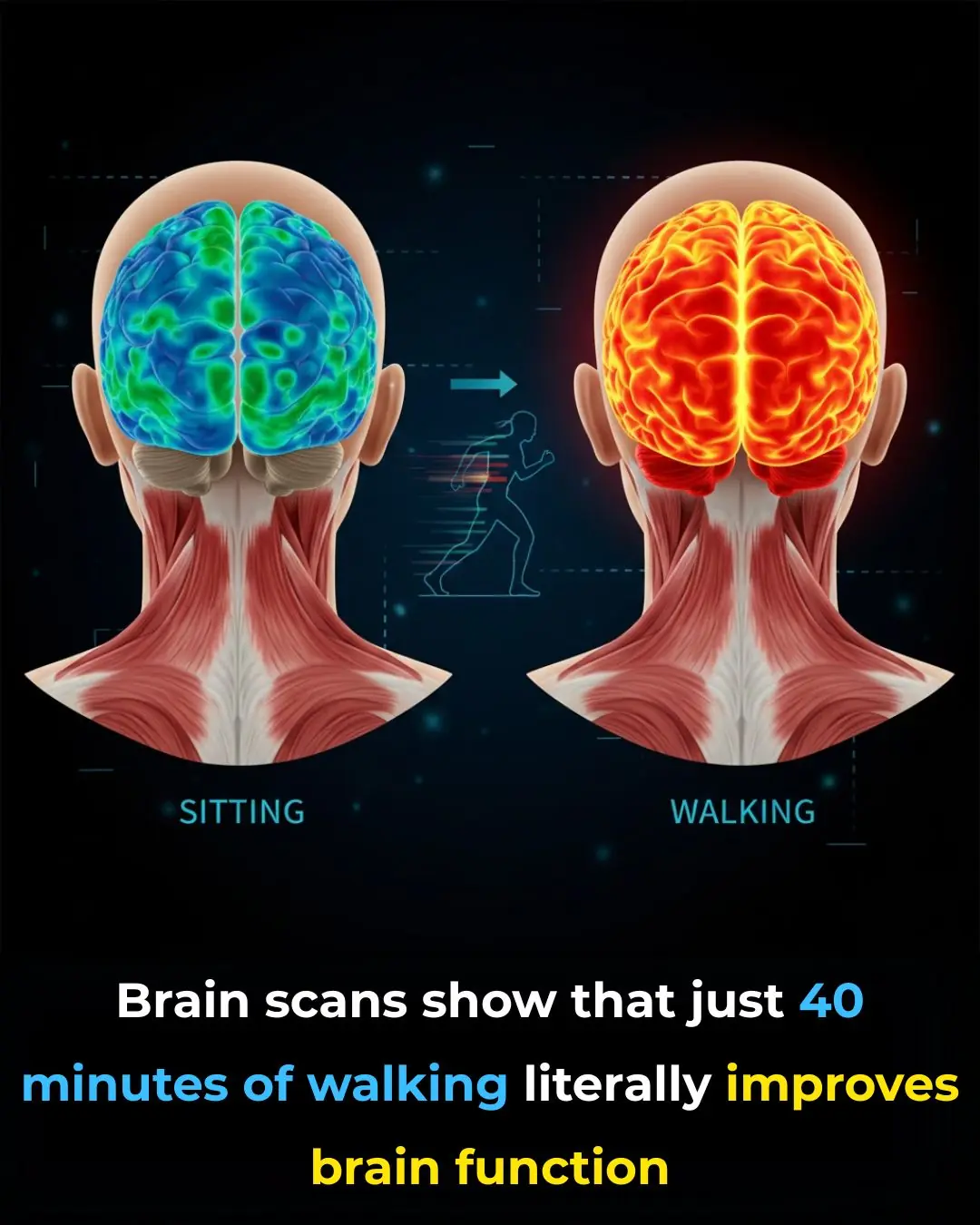
How Walking Activates the Brain: The Hidden Link Between Movement, Focus, and Mental Clarity
News Post
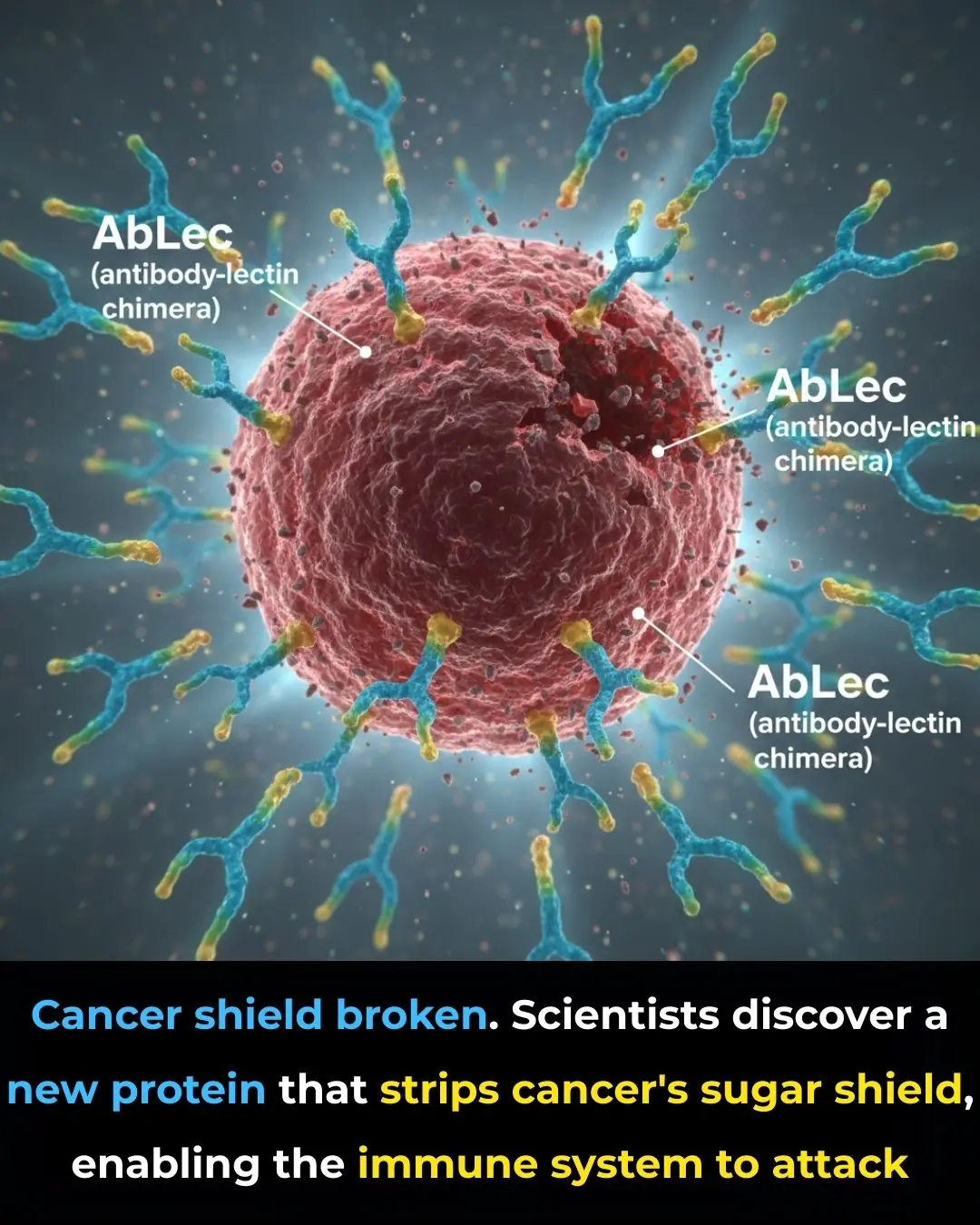
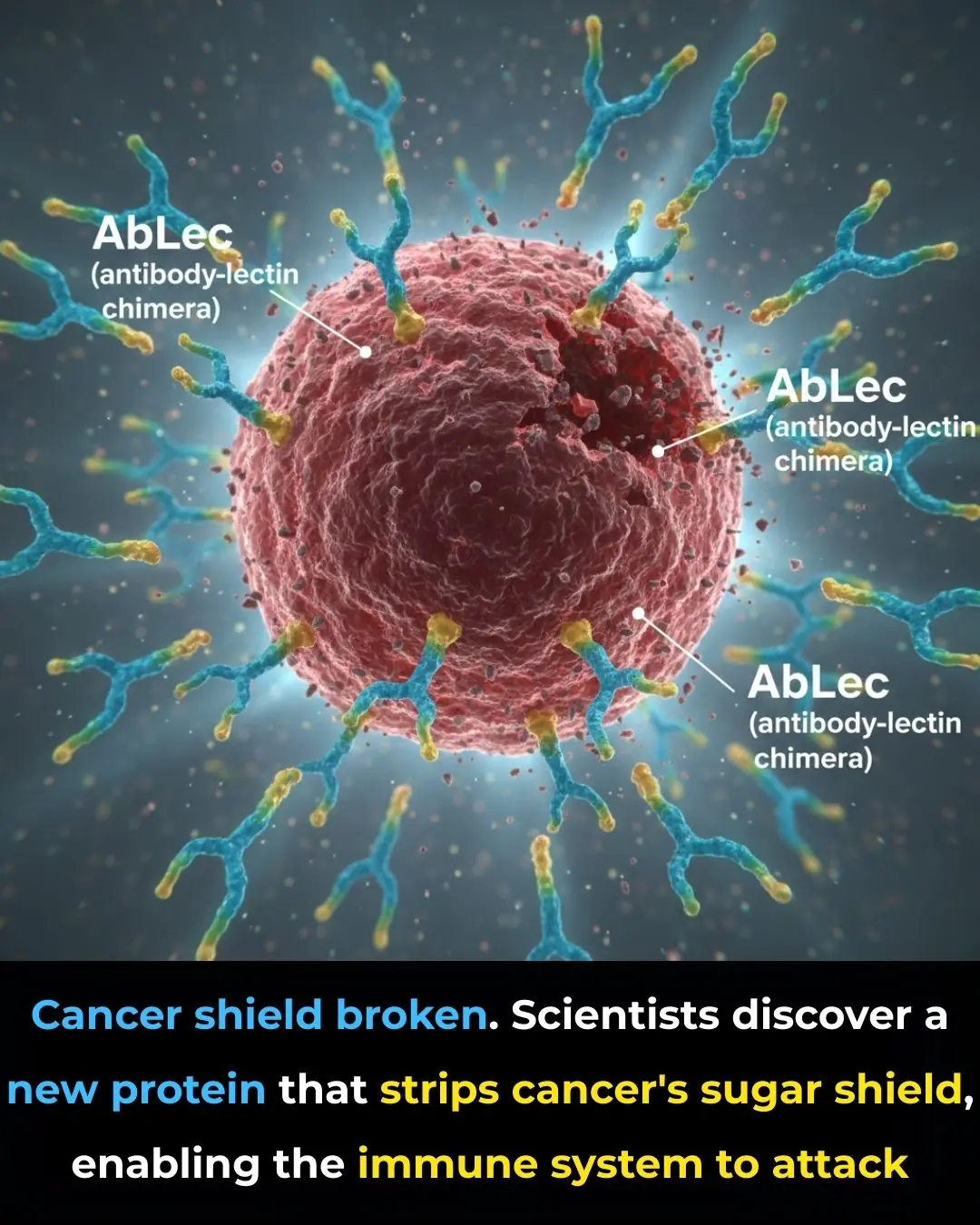
New Protein Breakthrough Unmasks Cancer Cells, Boosting the Power of Immunotherapy

Sugary Soft Drinks, Gut Bacteria, and Depression: How What You Drink May Shape Mental Health

Exploring the Traditional Uses and Potential Wellness Benefits of Prickly Lettuce Leaves (Lactuca serriola)

Pumpkin Seeds for Health: Natural Remedies, Recipes, and Benefits
11 Benefits of Dandelion Roots
7 Essential Leaves to Naturally Improve Your Eye Health
Are You Using New Tools to Support Patients With DD-CKD Anemia?

Five Reasons to Eat One Banana a Day: A Simple Habit for Better Health and Longevity

Three Simple Ways to Use White Radish to Reduce Phlegm, Relieve Cough, and Support Lung Health
Dreaming of Deceased Loved Ones: Is It a Good or Bad Sign?
A Couple Diagnosed With Liver Cancer at the Same Time: Doctors Urgently Warn After Opening Their Refrigerator

11 dishes you should never cook in an air fryer; don't try it or you'll regret it.

Put Bay Leaves in the Corners of Their Kitchen

The Simple Nighttime Habit That Can Help You Fall Asleep Faster
🌙 If You Notice These 3 Signs at Night, Your Kidneys Are Likely in Great Shape
Diagnosed with terminal cancer that had metastasized to the brain, the woman went for a check-up and burst into tears upon learning that her husband and son were the culprits

Doctors warn: 4 types of inflammation can easily turn into cancer in just one year if treatment is delayed
Why Some People Rub Onions on Their Windows
