How Gut Bacteria Influence Anxiety, Stress, and Emotional Well-Being
Many people think of mood as something controlled almost entirely by the brain, but modern research shows that the gut plays a much larger role than most of us realize. A substantial portion of the body’s serotonin—the neurotransmitter commonly associated with feelings of well-being, motivation, and emotional balance—is produced in the digestive system rather than in the brain itself. Although serotonin made in the gut does not directly cross into the brain, the systems that regulate it are closely linked, helping explain why digestive health and mental health so often rise and fall together.
This powerful connection exists because the gut is lined with millions of neurons, forming an extensive communication network known as the “enteric nervous system,” sometimes called the body’s “second brain.” It is directly connected to the brain through the vagus nerve, a major information highway that allows signals to travel continuously in both directions. Through this pathway, processes such as digestion, immune response, stress hormones, and emotional regulation constantly influence one another. As a result, discomfort in the gut can influence mood, energy, and clarity of thought, while psychological stress, anxiety, or fear can in turn disrupt digestion, appetite, and bowel habits.
A growing body of scientific research shows that the composition of gut bacteria—the microbiome—can influence anxiety levels, emotional regulation, memory, and even aspects of social behavior. These microbes interact with immune cells, produce bioactive compounds, and influence neurotransmitters such as serotonin and GABA that help regulate mood and calm the nervous system. When beneficial microbes thrive, they help reduce inflammation, strengthen the gut lining, and support smoother communication between the gut and brain. When this microbial balance is disturbed, however, people may experience increased stress sensitivity, mood fluctuations, gastrointestinal discomfort, and changes in sleep or appetite. Scientists are actively exploring whether targeted changes to the microbiome could one day complement psychological treatments.
Diet plays a central role in shaping this microbial environment. Fermented foods such as yogurt, kefir, kimchi, miso, and sauerkraut naturally contain live cultures that support the growth of helpful bacteria in the gut. High-fiber plant foods—fruits, vegetables, whole grains, nuts, and legumes—also provide prebiotics, the nutrients that feed these microbes and allow them to flourish. A diverse diet tends to produce a diverse microbiome, which is generally associated with greater resilience to stress and illness. In contrast, diets high in added sugar and ultra-processed foods may disrupt microbial balance, increase inflammation, and are frequently associated with worse stress-related and mood symptoms. Sleep quality, physical activity, and chronic stress levels also shape the microbiome, making lifestyle patterns an important part of the gut–brain connection.
It is important to emphasize that nutrition and gut health are not standalone cures for anxiety, depression, or other mental health conditions. These disorders arise from complex interactions among genetics, life events, personality, environment, and brain chemistry. However, maintaining a balanced microbiome, managing stress, exercising regularly, and eating a varied diet appear to support better emotional resilience and overall psychological well-being over time. Many clinicians view gut health as one piece of a comprehensive approach that can include therapy, medication when appropriate, social support, and lifestyle change. For individuals experiencing severe or persistent symptoms, professional medical or psychological care remains essential; dietary strategies should be seen as helpful complements rather than replacements.
The emerging science of the gut–brain axis represents an exciting frontier in health research. It highlights how closely the body and mind are intertwined and why digestive health deserves attention not only for physical comfort but also for emotional and cognitive well-being. Paying attention to gut health—through thoughtful nutrition, adequate sleep, regular movement, stress management, and when appropriate, medically guided use of probiotics—may help support a calmer mood, steadier energy, and clearer thinking in daily life. As research continues, the connection between what we eat, how our gut functions, and how we feel emotionally will likely become even better understood, opening the door to more holistic approaches to mental health.
Reputable sources for further reading on the gut–brain axis and mood
-
World Health Organization (WHO): Mental health, lifestyle, and noncommunicable diseases
-
National Institutes of Health (NIH): Human microbiome research and health outcomes
-
American Psychological Association (APA): The gut–brain connection and emotional regulation
-
Harvard Medical School / Harvard Health Publishing: The gut–brain axis, probiotics, and mood
-
Nature Reviews Gastroenterology & Hepatology: Reviews on microbiome–brain communication
-
The Lancet Psychiatry: Research on inflammation, microbiome, and mood disorders
News in the same category

The Science of Touch: How Hugging Improves Stress, Mood, and Immunity
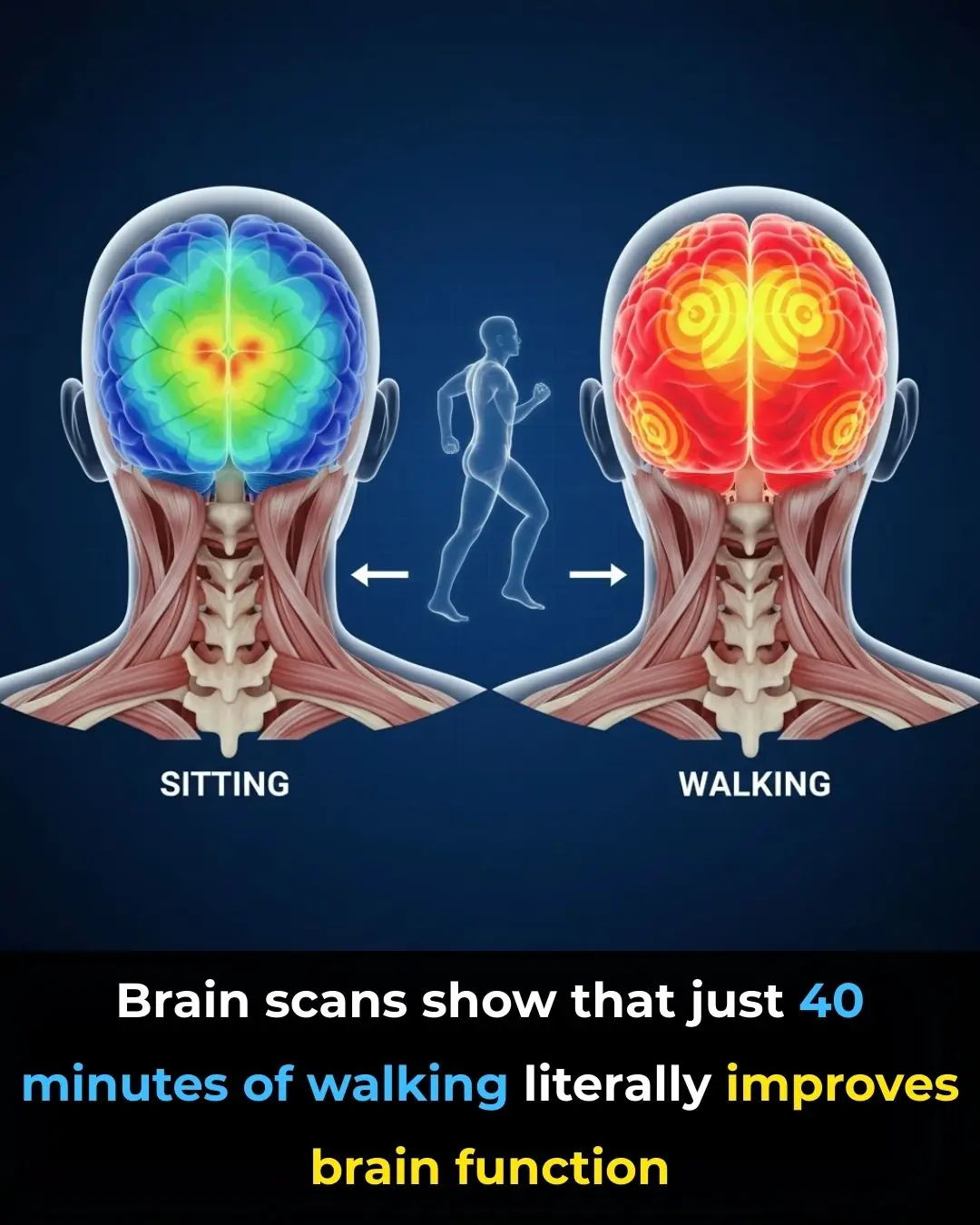
Your Brain on Walking: Why Movement Sparks Mental Clarity
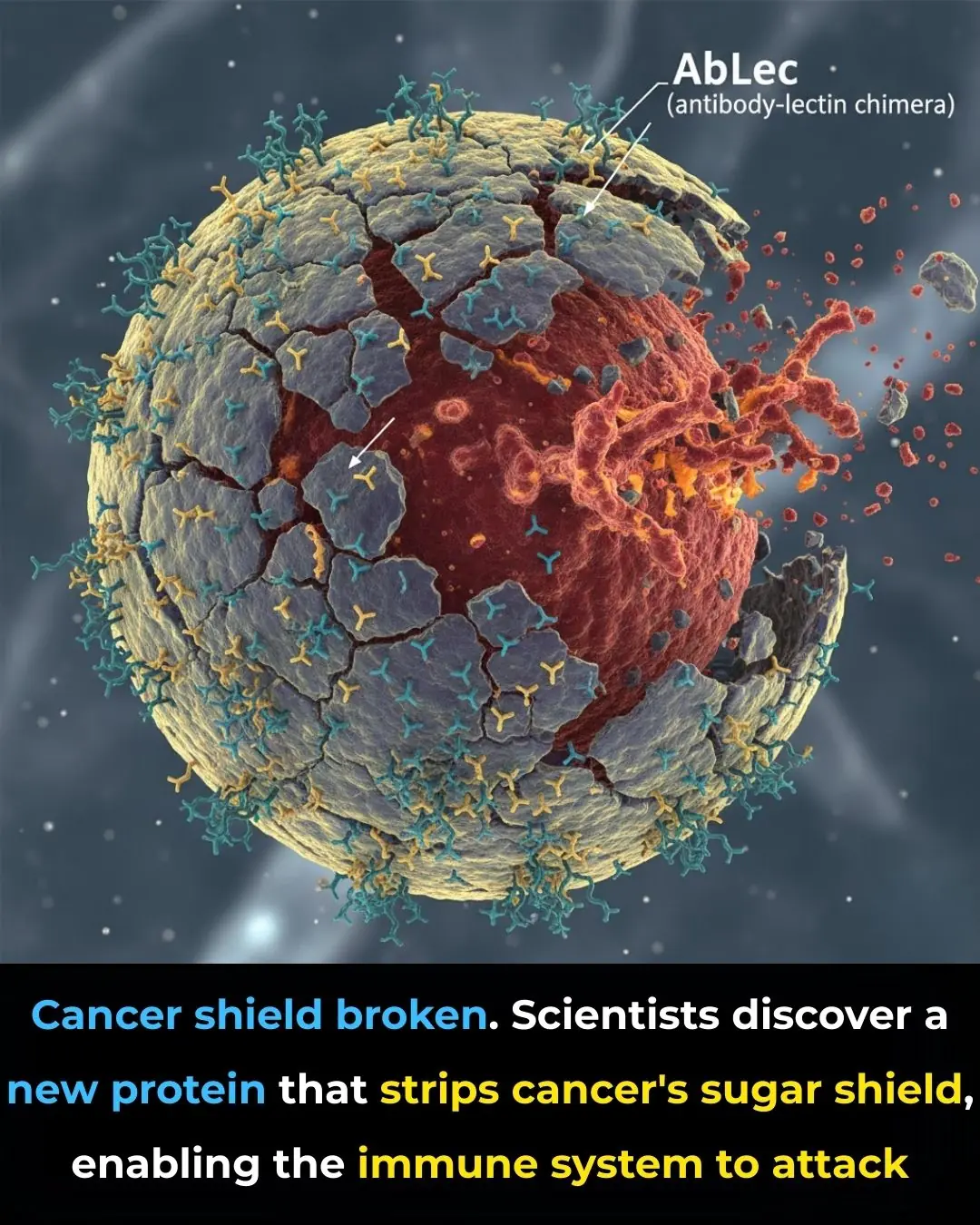
New Protein Breakthrough Helps Immune System Unmask and Destroy Cancer Cells

Using Star Apple Leaves to Treat Acid Reflux: A Traditional Remedy
Early-stage fatty liver disease: 5 obvious signs that can be noticeable on your face; ignoring them could lead to serious health consequences

Walking Barefoot at Home
Stroke and Cerebral Infarction Prevention:

If You Notice This Sign on Your Ear, Here’s What It Could Mean

5 Foods That Boost Immunity Better Than Garlic
What Is Stomach Cancer?
How the “3-2-1” Rule Can Help You
What Is the Adam’s Apple
Proven Inflammatory Foods to Avoid According to Science

14 Signs Your Blood Sugar Is Way Too High (And 14 Ways to Reduce It)

Kidney Stones and Cancer Risk: What Recent Studies Are Revealing

When GLP-1 Medications Fall Short: Why Some Patients Don’t Lose Weight
CDC Restructures Childhood Vaccine Recommendations Into Three Categories
News Post

India Creates History at the Asian Para Youth Games 2025 🏅🇮🇳✨

Toxic Teaser Storm: Yash Redefines Cinematic Hype 🎬🔥

India’s Next Rail Leap: Vande Bharat Sleeper Train Aces Final High‑Speed Trial 🚆🇮🇳

Dashavatar: Marathi Cinema’s Historic Leap to the Academy Awards 🏆🌍✨
Supreme Court of India Reaffirms Merit in Public Employment ⚖️🇮🇳
The iBomma Shockwave: How Immadi Ravi’s Arrest Exposed a Cybercrime Empire 🎬🔥
Steaming crab often results in the claws falling off and a fishy smell, but a chef reveals: Just follow these steps and the crab will be sweet, the meat won't dry out, and it will be incredibly fragrant.

Don't put shrimp in the refrigerator right away after buying them; add one spoonful of this sweet seasoning and they'll stay fresh for a long time.
When simmering bones, you absolutely must add these three spices; the broth will be clearer and incredibly fragrant.

Tips for choosing shrimp: Look at this one spot and you'll know immediately whether it's natural shrimp or shrimp injected with additives.

How to use baking soda correctly for more effective cleaning.
How Swimming Rewires the Brain and Strengthens Cognitive Health

A mistaken text connected them. Now they’ve become one of America’s favorite Thanksgiving traditions

Four Golden Times to Drink Coffee for Maximum Health Benefits
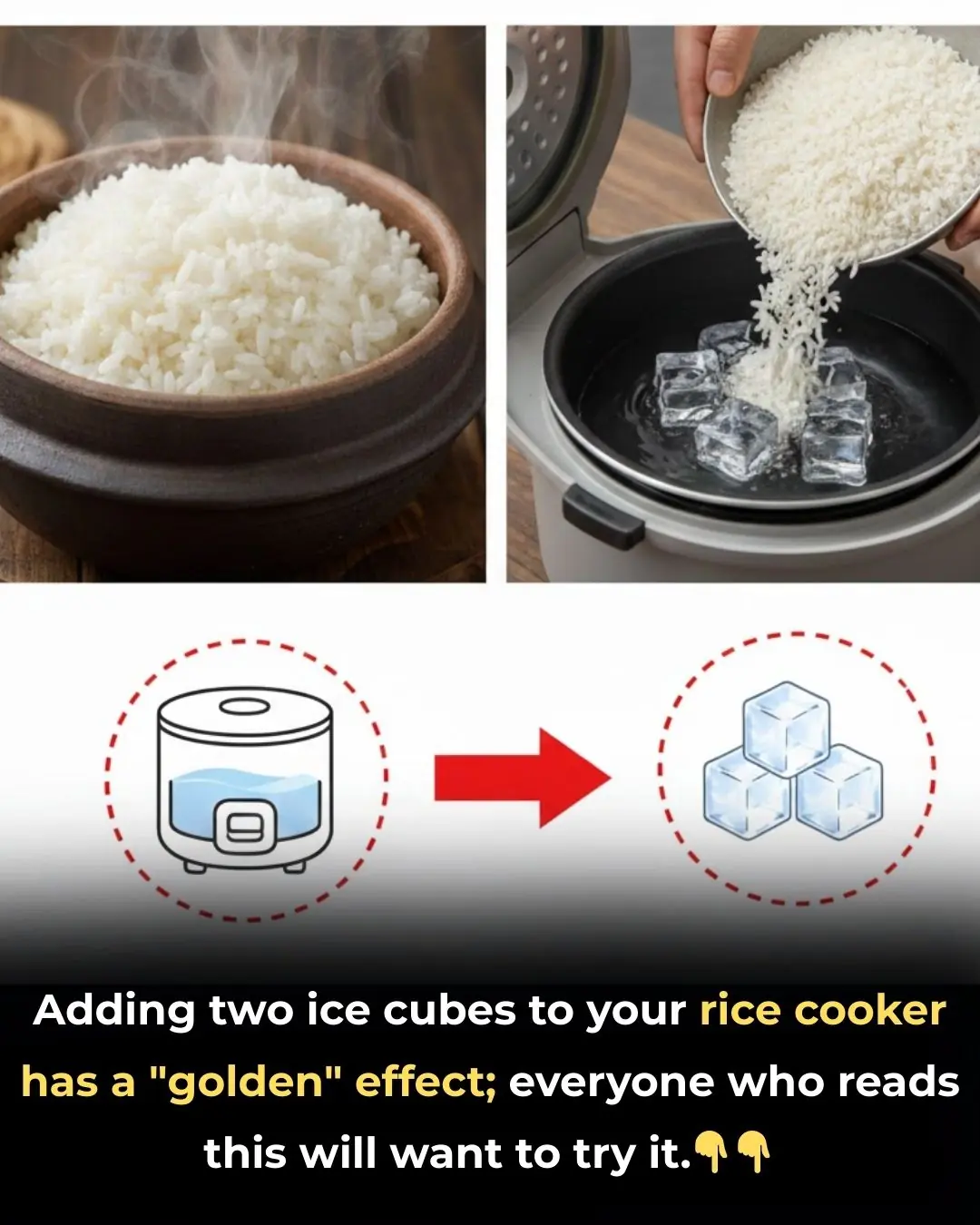
With just two ice cubes, you can achieve surprisingly delicious and fluffy rice!

Cut an onion and place it in the corner of your bed overnight. You will see a miracle the next morning.

Regularly eating tofu can cause four unexpected changes in the body.

7 foods that, if cooked once and not finished, should be thrown away instead of being kept overnight in the refrigerator or reheated, as it's extremely harmful.

Pickled onions for Tet (Vietnamese New Year) only require one ingredient readily available in the kitchen; the onions become fragrant, crispy, and have a uniquely delicious taste.
