Natural Ways to Keep Your Arteries Healthy and Improve Blood Circulation
Thrombosis — a silent danger, and how to fight it (detailed, practical guide)
What is thrombosis?
A thrombosis is a blood clot (thrombus) that forms inside a blood vessel and blocks or reduces blood flow.
Clots in veins (venous thrombosis) most often occur in deep leg veins (DVT — deep vein thrombosis) and can break off and travel to the lungs (pulmonary embolism, PE).
Clots in
arteries (arterial thrombosis) block oxygen delivery to organs and cause heart attacks or ischemic stroke.Both can be life-threatening and require prompt attention.
Why thrombosis happens — major risk factors
-
Stasis (slow blood flow): long bed rest, long flights, immobilization.
-
Hypercoagulability: inherited clotting disorders, cancer, pregnancy, some medications (e.g., certain hormonal therapies).
-
Endothelial injury: vessel damage from surgery, trauma or inflammation.
-
Other important risks: older age, obesity, smoking, dehydration, uncontrolled diabetes, high blood pressure, high cholesterol.
This combination (stasis + hypercoagulability + vessel injury) is the classic explanation for why clots form.
Early warning signs to NEVER ignore
Venous thrombosis (DVT): swelling (usually one leg), pain or tenderness (often in calf), warmth and redness over a vein.
Pulmonary embolism (PE — emergency):
Arterial thrombosis (heart/stroke): chest pain, sudden weakness or numbness (one side of body), slurred speech, vision problems — seek emergency care.
Medical treatment (must-see-your-doctor)
-
Anticoagulants (“blood thinners”) — the mainstay for most DVT/PE cases (e.g., heparin, low-molecular-weight heparin, direct oral anticoagulants like apixaban/rivaroxaban). They prevent clot growth and new clots. Treatment length depends on cause (often 3–6 months or longer for unprovoked clots).
-
Thrombolysis (clot-busting drugs) — used selectively for large, limb-threatening, or life-threatening clots (in hospital).
-
Mechanical thrombectomy / IVC filters / surgery — used for specific cases when drugs are insufficient or contraindicated.
-
Follow-up tests (ultrasound, CT angiography, blood tests) guide therapy.
Important: Do not self-treat. Only a clinician can choose and monitor anticoagulation safely.
Natural & lifestyle strategies to keep arteries healthy and improve circulation
These reduce your long-term risk of clotting and improve vascular health — excellent complements to medical care but not replacements for prescribed treatment.
1) Move regularly — reduce stasis
-
Aim:
at least 150 minutes/week moderate aerobic exercise (brisk walking, cycling) plus two sessions of resistance training weekly. Even short walks every 30–60 minutes during long sitting/flight reduce clot risk. -
Why:
movement improves venous return, lowers blood pressure and insulin resistance, and reduces obesity.
2) Maintain a healthy weight & manage metabolic risks
-
Losing excess weight reduces pressure on leg veins and lowers inflammation, blood pressure and diabetes risk. Manage blood sugar, blood pressure and cholesterol with lifestyle and meds when indicated.
3) Diet for circulation and artery health
Follow a Mediterranean–style eating pattern:
-
Eat more: oily fish (salmon, mackerel — omega-3s), nuts, seeds, legumes, whole grains, plenty of vegetables and fruits, olive oil, garlic, and foods high in fiber and antioxidants.
-
Limit: processed meats, refined carbs, added sugars, trans fats, and excess salt.
-
Why: a balanced diet lowers atherosclerosis (arterial plaque), reduces obesity and insulin resistance — all reduce thrombosis risk.
4) Hydration
-
Drink enough water — dehydration thickens blood and can increase clot risk, especially during travel or heat. Sip steadily and avoid excess alcohol.
5) Stop smoking & limit alcohol
-
Quit smoking — tobacco damages vessels and raises clot risk. Cut alcohol (none is best for heart/vascular health).
6) Compression stockings when appropriate
-
Graduated compression stockings (properly fitted) reduce DVT risk in people with chronic venous insufficiency or after some surgeries — discuss use with a clinician.
7) Manage stress & sleep
-
Chronic stress raises inflammatory hormones and BP; good sleep and stress reduction (meditation, breathing, social support) support vascular health.

Specific exercises that help circulation (how to do them)
-
Walking: 20–30 minutes daily; add short 3–5 minute walks every hour if sitting long.
-
Calf pumps: sit or stand, point toes up and down 20–30 reps, repeat hourly while seated — powerful for venous return.
-
Ankle circles and leg lifts: mobilize lower limb blood flow.
-
Resistance training: 2×/week (squats, lunges, light weights) to improve muscle pump and metabolic health.
-
Stretching & yoga: improve flexibility, reduce venous stasis, and reduce stress.
Always start slowly if deconditioned and get medical clearance if you have cardiopulmonary disease.
Supplements — what to know
-
Omega-3 (fish oil) can help cardiovascular health but discuss dose with a doctor if you take anticoagulants (it can increase bleeding risk).
-
Vitamin K (in green leafy vegetables) affects some anticoagulants (warfarin) — keep intake consistent and inform your clinician.
-
Don’t start herbal “blood thinners” (ginkgo, high-dose garlic, turmeric) without medical advice — they can interact with prescribed anticoagulants.
How to prevent thrombosis during travel, surgery or illness
-
On long flights/car rides: stand and walk every 1–2 hours, do seated calf exercises, wear loose clothes, consider compression stockings if high-risk.
-
Before surgery or when immobile: follow pre-op and hospital guidance — hospitals often use anticoagulant prophylaxis and mechanical measures (stockings, pumps).
When to see a doctor — urgent signs
-
Sudden leg swelling or pain (especially one leg).
-
Sudden shortness of breath, chest pain, fainting, or coughing up blood.
-
Sudden neurological deficits (weakness, slurred speech, vision loss).
These situations are emergencies. Prompt diagnosis and treatment save lives.
Practical daily checklist to reduce your risk
-
Move every hour if sitting long.
-
Walk 20–30 minutes daily and do strength exercises twice weekly.
-
Eat Mediterranean-style: fish, veg, fruit, whole grains, nuts; limit sugar and processed foods.
-
Hydrate, stop smoking, limit alcohol.
-
Maintain healthy weight, control BP/cholesterol/diabetes.
-
Use compression stockings when recommended and follow medical advice about anticoagulation if you’re high-risk.
Thrombosis can be silent until it causes a major problem. Lifestyle changes strongly reduce risk, but they do not replace medical diagnosis or prescribed anticoagulation when a clot exists or when you have high clinical risk.
If you think you have symptoms or are at increased risk, see a healthcare professional promptly for testing and individualized treatment.
News in the same category

Soak garlic in vinegar, do this way, ensure white garlic crispy, attractive

Vinegar Soaking: 4 Great Uses Recognized by Families, Everyone Loves It

Don't put the ginger you don't eat all in the refrigerator. Do this so the ginger doesn't dry out or rot. After 1 year, it's still fresh.

Sprouted foods are more precious than 'pure gold'
Tips to clean rust from gas stoves with rice water and cooking oil. It sounds like a joke but the effect is surprising, the stove is sparkling clean.

How to use Fo-ti to stimulate hair growth, make hair black, shiny and smooth

When buying honey, just turn the honey bottle upside down and at a glance you can tell real and fake honey. Don't buy it randomly.

No need for mosquito coils, use this readily available thing in your home to make mosquitoes run away, cheap and safe

Put your hand on the mirror and discover a 2-way mirror in a motel or hotel

Dirty bathroom mirror: Mix this with water and wipe it once to make the mirror shiny
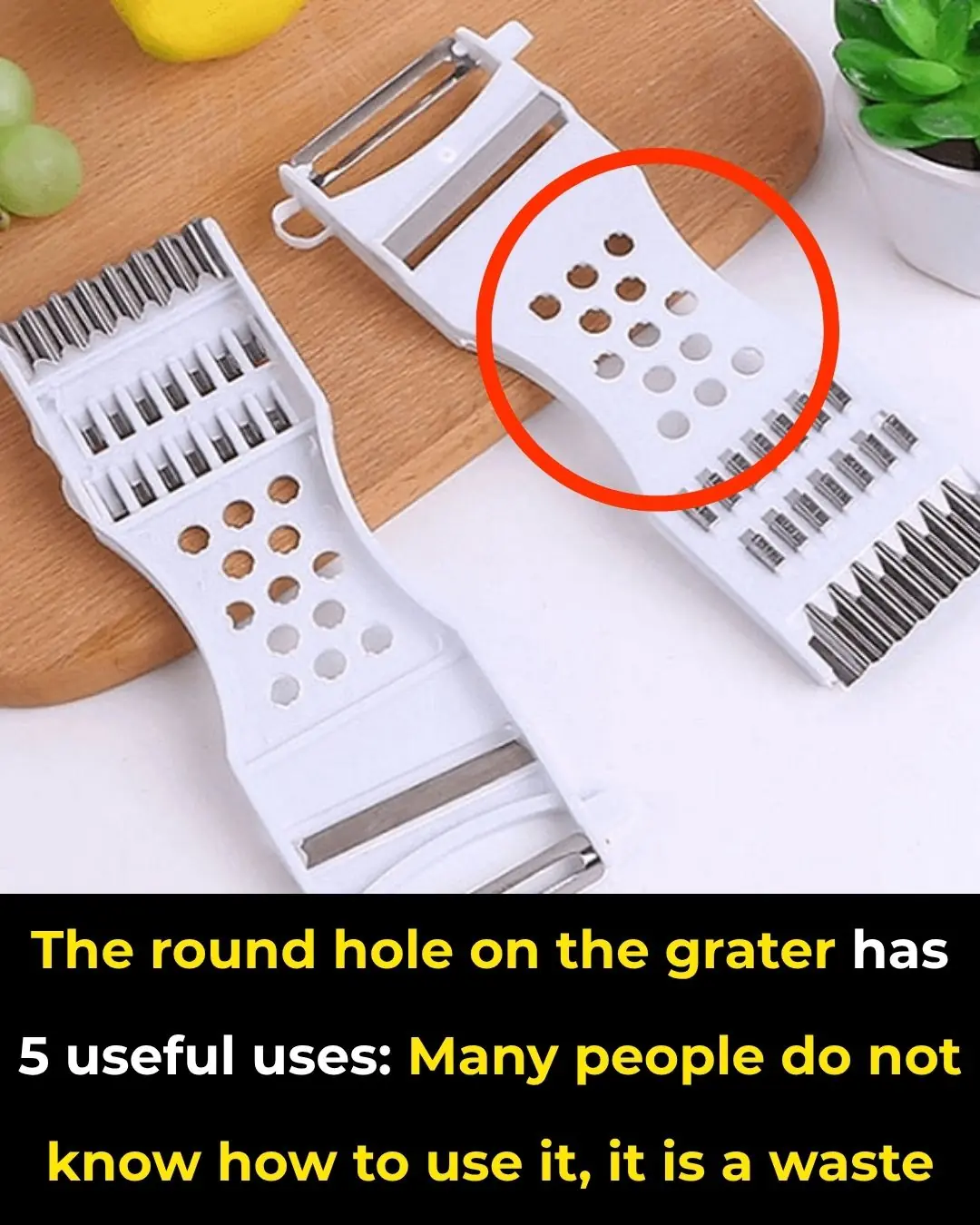
The round hole on the grater has 5 useful uses: Many people do not know how to use it, it is a waste

Check out this how-to right now. It will help you

Are Crocs Actually Bad for Your Feet

Don’t throw away bubble wrap — keep it in the kitchen and you’ll be surprised by its amazing uses!

Over time, kitchen sinks can become stained and dull — use this to scrub and make it shine like new

Place a plate of salted lemon at the head of the bed: Get 5 great benefits and secrets that unfortunately few people know

Add this to the water. Even when you don’t clean the floor in a week
News Post

The Man Who Remembers Hunger: Why One Act of Kindness Matters.

The Little Elephant Who Was Born Different: A Pink Calf in the Wild

When Love Has No Address: A Man and His Dogs

A Boy, a Soldier, and an Umbrella: A Timeless Gesture of Respect

Purslane: The Superfood That Tastes Better Than Meat – 7 Reasons to Grow It in Your Garden

Don't Throw Old Tomatoes in the Trash.Turn them into flavorful tomato powder.

Banana Blossom: Health Benefits, Recipes, and Uses

Onion, Garlic, and Olive Oil Remedy for Varicose Veins: Natural Treatment and Benefits

The Photo of the Year: A Glimpse of Courage the World Must Not Forget

7 Surprising Benefits of Euphorbia Hirta

How to Regrow Food in Water: 10 Foods that Regrow Without Dirt

Firefighters Save Trapped Fawn from Storm Drain, Reuniting It with Nature

10 benefits of pigweed

Wild Lettuce Sap: Benefits and Uses

When “Just a Dog” Becomes the Difference Between Life and Death

Teddy’s Hug: A Rescue Story of Unbreakable Love

Benny’s Redemption: A Journey from Loneliness to Love
Man has stroke after bathing right after meal: 3 mistakes you shouldn’t make

Redemption in Yarn and Paws: How a Cat Gave My Brother Back His Life