
Scientists install the world’s first electronic spine to restore movement after paralysis.

Redefining Paralysis: How a Groundbreaking “Electronic Spine” Reconnects the Brain and Body
For millions living with paralysis, the divide between brain and body has long been seen as an unbridgeable chasm—a devastating line that modern medicine could not cross. Traditional treatments for spinal cord injuries have typically focused on helping patients adapt to their new limitations rather than restoring what was lost. But that narrative is beginning to change, thanks to a pioneering breakthrough from Northwell Health’s Feinstein Institutes for Medical Research.
In a historic world-first, scientists have developed and successfully implanted a revolutionary “electronic spine”—a sophisticated system designed to restore both movement and sensation in a person with complete paralysis. This technological triumph marks the first time the brain, spinal cord, and limbs have been electronically reconnected in a human being, potentially ushering in a new era of neurorehabilitation.
Breaking Barriers: A New Era in Spinal Cord Injury Treatment
Spinal cord injuries (SCIs) have traditionally been considered irreversible. Damage to the spinal cord, particularly in the cervical vertebrae, often results in permanent paralysis. Most existing treatments aim to help patients cope through assistive devices and physical therapy, offering limited progress in functional restoration. However, a recent clinical trial led by Professor Chad Bouton at Northwell Health’s Feinstein Institutes is rewriting this medical rulebook.
The trial focused on Keith Thomas, a 45-year-old man who became quadriplegic in 2020 following a diving accident that fractured his C4 and C5 vertebrae. Left with no sensation or motor control below the chest, Thomas became the first human to receive the “double neural bypass” system—an integrated set of brain implants, spinal stimulators, and AI processors.
After a marathon 15-hour surgery and months of mental training, Thomas was able to voluntarily move his arm and, even more astonishingly, feel his sister’s touch for the first time in over three years. “This is the first successful demonstration of a full, bidirectional brain-body connection in a person with paralysis,” said Prof. Bouton, a leader in bioelectronic medicine.

How the Technology Works: Inside the “Double Neural Bypass”
At the heart of this innovation lies the concept of re-establishing communication between the brain and paralyzed limbs—not just to control movement, but also to restore feeling. The “double neural bypass” is a closed-loop system designed to allow two-way signal transmission between the brain and body, replacing the broken pathway in the spinal cord.
The journey began with advanced brain mapping using functional MRI to identify the precise regions responsible for both motor intent and sensory perception in Thomas's brain. Surgeons then implanted two motor chips and three sensory chips in those exact areas. In a rare and delicate step, part of the surgery was conducted while Thomas was awake, enabling real-time confirmation of accurate placement.
Once implanted, the brain chips capture electrical signals that represent thoughts of movement. These signals are decoded using AI and sent to external computers, which then activate electrode patches on Thomas’s spine and forearm. Simultaneously, sensors on his fingers collect data about pressure and touch, relaying that information back to the sensory implants in his brain.
This full-loop communication allows Thomas not only to move his limbs on command but also to feel texture, resistance, and touch—sensations previously lost to paralysis. “The brain isn’t just talking to the body again—it’s listening too,” Prof. Bouton explained.
A Leap Beyond Robotics: Toward Real-Time, Natural Movement
Earlier attempts at restoring mobility in paralyzed patients often involved robotic limbs or exoskeletons controlled by brain signals. While impressive, these systems lacked the essential feedback loop that allows natural motion. Patients could move a robotic limb, but they couldn’t feel it.
Northwell’s innovation bridges that gap by integrating the nervous system with bioelectronic components inside the body. Unlike previous systems reliant on bulky lab setups, this platform is designed with future mobility in mind. Its goal is not only function but autonomy—empowering patients to regain real control over their bodies.
The implications extend beyond the technology itself. The system taps into the brain’s remarkable capacity for adaptation. As Thomas continued therapy, his natural arm strength doubled—even when the implants were turned off. This suggests that the device may actually stimulate neuroplasticity, helping the nervous system to rewire itself and potentially heal over time.

Keith Thomas’s Journey: From Complete Paralysis to Feeling Again
For Keith Thomas, this clinical trial was far more than an experiment—it was a return to hope. Before the surgery, Thomas required round-the-clock care and had little chance of regaining any mobility. But following months of targeted neurorehabilitation with the double neural bypass, he made astonishing strides.
He could raise his arms voluntarily, feel pressure in his hands, and perform basic movements using only his thoughts. Perhaps most emotionally moving was the moment he felt his sister’s hand in his for the first time in years—a simple act that carried profound meaning.
“It felt like I got a part of my life back,” Thomas shared in a press briefing. The emotional and psychological impact of reclaiming agency over one’s own body cannot be overstated. His experience is living proof that even after years of paralysis, the human nervous system retains a powerful, dormant potential for renewal.

What’s Next: From Breakthrough to Widespread Application
With this unprecedented success, Northwell researchers are now focused on making the technology more practical and scalable. Their next steps involve refining the system’s hardware—moving from external ports to fully implantable devices, enhancing wireless communication, and reducing system size to make it wearable or even invisible under the skin.
They’re also planning to expand the technology’s applications to other conditions, including stroke, traumatic brain injury, and neurodegenerative diseases like ALS. By stimulating specific neural circuits, the team hopes to unlock recovery pathways that traditional treatments have failed to reach.
Long-term studies are underway to monitor durability, performance, and safety over time. Scaling this approach to larger patient populations will also involve tackling regulatory, ethical, and cost-related challenges.

A Future Reimagined: Bridging Science, Compassion, and Possibility
The installation of the world’s first electronic spine is not just a medical triumph—it’s a bold reimagining of what’s possible in the treatment of paralysis. It signals a shift from passive care to active restoration, from dependence to agency.
As research evolves, society must now confront important questions: How do we ensure fair access to such life-changing technologies? How do we prepare healthcare systems to support their integration? And how do we maintain human dignity and autonomy in the age of machine-assisted healing?
“This is just the beginning,” said Prof. Bouton. “Our mission is to help people with paralysis reclaim their lives—not just in labs, but in their homes, their communities, and their futures.”
The once unimaginable is becoming reality. For millions living with paralysis, hope has a new name—and it’s written in neural code.
News in the same category


Scientists Warn: Universe’s ‘Self-Destruct Button’ Could Trigger Without Warning

WORLD'S FIRST DATE SOFT DRINK
We weren’t the only humans just the last ones left to tell the tale

Japanese “Baba Vanga” Meme Resurfaces After July 2025 Tsunami Triggers Alerts
Why you should always put a coin in the freezer before you leave home

Heroic Teen Malaya Grace, 17, Dies After Saving Siblings from Drowning in Texas Floods

Why You Should Never Ever K--ill A House Centipede If You Find One Inside Of Your Home
‘Granny Pods’ Let Aging Parents Stay Close by in Your Backyard

Airport baggage handler issues warning to anyone who ties a ribbon on their suitcase
What Does it Symbolize When a Person Who Passed Away Shows up in Your Dream?
Optical illusion reveals whether you’re an introvert or extrovert

Trapped in Silence: Boy Awakens After 12-Year Coma With Terrifying Secret
Imagine suddenly being trapped inside your own body—fully conscious, aware of your surroundings, but completely unable to move, speak, or communicate in any way. For Martin Pistorius, this unimaginable scenario was reality for more than a decade. His st

Urgent warning issued to all iPhone users following release of iOS 18.6

Experts Warn of Imminent 'Cosmic Hell' That Could Wipe Out Mankind, Exact Time Revealed
Though the ending is billions of years away, the emerging evidence is shifting scientific consensus on cosmic fate. Understanding dark energy—the force shaping expansion—is one of the greatest unsolved mysteries in physics.

Ancient tablet has been completely translated and has some terrifying predictions for humanity
Astronaut Waves And Turns His Camera To Disprove The Flat Earth Theory For Good
Your iPhone’s Volume Buttons Are Loaded with Hidden Features

Astronaut shares the profound ‘big lie’ he realized after seeing the Earth from space
News Post

Earth Plunged Into Darkness For Six Minutes In Rare Event Not Seen In A Century

The Hidden Meaning Behind Leg-crossing — It’s More Than Just Comfort

Scientists Warn: Universe’s ‘Self-Destruct Button’ Could Trigger Without Warning

WORLD'S FIRST DATE SOFT DRINK
We weren’t the only humans just the last ones left to tell the tale

Japanese “Baba Vanga” Meme Resurfaces After July 2025 Tsunami Triggers Alerts

Top Signs of Iron Deficiency and How To Increase Iron Levels In Your Blood

Doctors Suspected Baby Had Mouth Tumor—The Shocking Truth Left Them Speechless

Why Some People Never Break A Bone—3 Wild Theories Explained
JAW DROPPING SIMULATION SHOWS WHAT HAPPENS TO YOUR BODY WHILE FASTING FOR 36 HOURS TO ACHIEVE 'FULL RESET'
Why you should always put a coin in the freezer before you leave home

6 Health Benefits of Sleeping In a Cold Room and How to Make it Cooler- And Why You May Not Want to Use a Fan
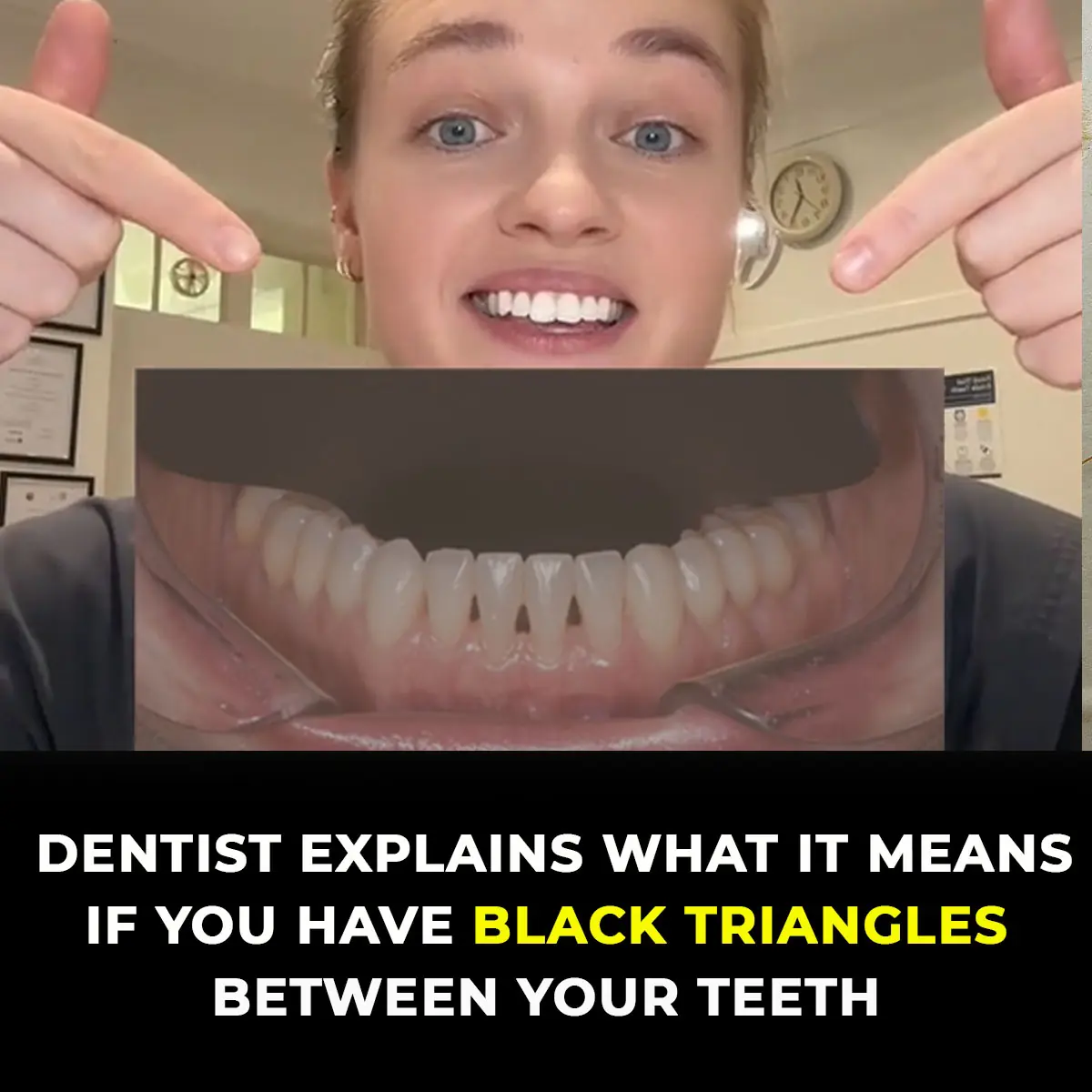
Dentists Explain What Those Black Triangles Are Between Your Teeth

Heroic Teen Malaya Grace, 17, Dies After Saving Siblings from Drowning in Texas Floods

Silent Walking’ Is The Latest Trend Gen Z Are Obsessed With

Why You Should Never Ever K--ill A House Centipede If You Find One Inside Of Your Home
‘Granny Pods’ Let Aging Parents Stay Close by in Your Backyard

Airport baggage handler issues warning to anyone who ties a ribbon on their suitcase
This optical illusion may help identify autistic traits in seconds
