Surgeons Face the Highest Mortality Risk Compared to Other Physicians, Study Finds
From elevated cancer rates to stress-induced cardiovascular disease, the profession carries health costs that demand greater awareness and intervention.
New evidence suggests that the shingles shot may not only prevent a painful rash but also cut dementia risk, offering fresh hope for millions worldwide.
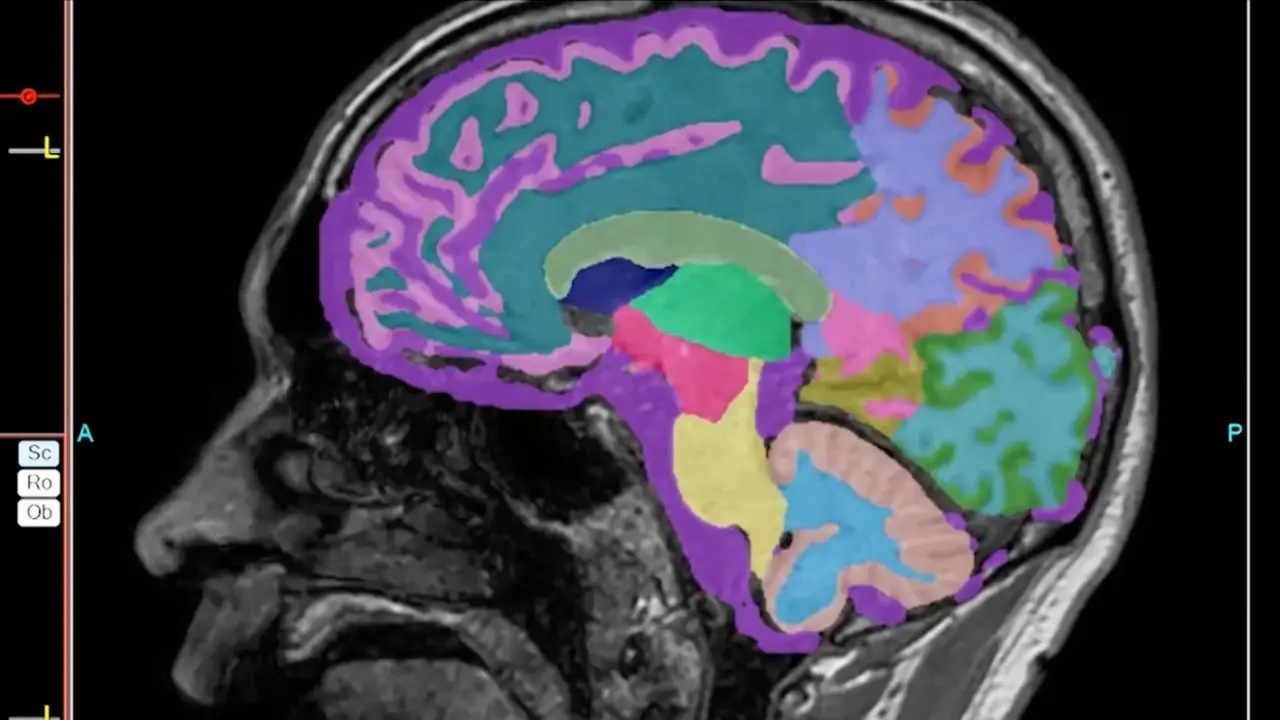
An unusual public health policy in Wales has provided researchers with one of the clearest indications yet that vaccines can play a direct role in lowering dementia rates. A major study led by Stanford Medicine found that older adults who received the shingles vaccine were about 20% less likely to develop dementia over the following seven years compared to their unvaccinated peers.
Published in Nature on April 2, the study reinforces a growing theory: viruses that affect the nervous system may accelerate dementia risk. If this link continues to hold up, the path toward a preventive measure for dementia could be much closer than previously imagined.

A Virus That Never Really Leaves
Shingles, triggered by the varicella-zoster virus — the same culprit behind childhood chickenpox — remains hidden in the body for decades. After lying dormant in nerve cells, the virus can reactivate later in life, especially when immunity weakens, causing painful rashes and complications. Now, evidence suggests that these viral reactivations might also contribute to long-term neurological decline.
Globally, dementia affects more than 55 million people, with 10 million new cases emerging each year. Despite decades of research centered on the buildup of plaques and tangles in the brain, breakthroughs in prevention have been elusive. The possibility that infections — particularly viral ones — play a hidden role in dementia progression is now attracting significant attention.
Tackling Bias With a “Natural Experiment”
Previous studies had hinted at a link between shingles vaccination and reduced dementia rates, but skeptics pointed out a major flaw: people who seek vaccinations are often more health-conscious in general. Healthier diets, more exercise, and better overall habits can all reduce dementia risk, muddying the picture.
Enter an unusual rollout policy in Wales. Starting in 2013, only those who turned 79 during a specific eligibility window were offered the live-attenuated shingles vaccine. Those who were 80 at the time missed their chance permanently. This quirky age-based rule created a near-randomized natural experiment, allowing researchers to compare two nearly identical groups divided only by a cutoff date.
The study examined the health records of over 280,000 adults aged 71 to 88 with no dementia diagnosis at baseline. By tracking outcomes for those who were eligible versus ineligible, researchers effectively sidestepped the usual biases of lifestyle and behavior.
Dementia Rates Fell Dramatically
The results were striking. Among older adults monitored over seven years, those vaccinated against shingles were not only 37% less likely to develop shingles itself but also had a 20% lower risk of dementia. By 2020, roughly one in eight older adults had developed dementia, yet those who received the vaccine fared significantly better.
“The protective signal was consistent and unmistakable,” said Pascal Geldsetzer, MD, PhD, the study’s senior author. Importantly, researchers scoured the data for confounding variables — such as education level, other preventive care, or chronic health conditions — and found no meaningful differences. The vaccine itself remained the only clear factor.
Women Showed Stronger Protection
Another fascinating insight emerged: the vaccine’s dementia protection was more pronounced in women. Scientists believe this could be linked to differences in immune response, as women often mount stronger antibody defenses, or to the fact that shingles is generally more common among women than men.
What This Means for the Future
Whether the vaccine guards against dementia by bolstering immune resilience, preventing viral reactivation, or through another unknown mechanism is still unclear. Researchers are now eager to study newer, protein-based shingles vaccines, which are even more effective against the virus.
Encouragingly, similar protective effects have been observed in health data from England, Australia, New Zealand, and Canada, suggesting that the Welsh findings are not a fluke. Geldsetzer and colleagues are now pushing for a large-scale randomized controlled trial, which could definitively confirm the vaccine’s role in dementia prevention.
“It’s rare in medicine to see such a strong, clear, and reproducible signal,” Geldsetzer said. “If we act on it, we could change the trajectory of dementia prevention for millions.”
From elevated cancer rates to stress-induced cardiovascular disease, the profession carries health costs that demand greater awareness and intervention.






Catching these subtle, non-motor clues may help identify Parkinson’s long before the motor stage, opening the door to interventions that could delay its full expression.

While debate continues over its official recognition, the research shines a spotlight on the neurological toll of modern labor demands and could pave the way for tailored treatments in the future.

The study authors emphasize that these findings mark only the beginning.







Avoiding purine-heavy foods like organ meats, processed meats, certain fish, and yeast-based products can help reduce flare-ups and maintain joint health.
From constant-use devices like refrigerators to high-powered kitchen tools, every household has hidden electricity traps.
From elevated cancer rates to stress-induced cardiovascular disease, the profession carries health costs that demand greater awareness and intervention.


Homemade carrot oil is a simple, nutrient-packed solution for brighter, firmer, and deeply hydrated skin. Whether you choose the slow, nutrient-preserving sun infusion or the quick simmering method, this golden oil can rejuvenate your skin from the inside