While meningiomas remain uncommon, this research suggests that some forms of hormonal contraception — particularly long-term injectable Depo-Provera — may raise the risk more than previously understood.
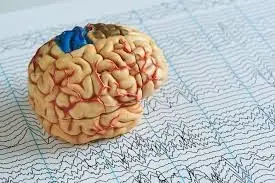
A new large-scale study of more than 10 million women in the U.S. has raised concerns about a widely used contraceptive injection. Researchers found that long-term use of depot medroxyprogesterone acetate (commonly known as Depo-Provera) may significantly increase the risk of developing meningioma, a type of brain tumor.
While meningiomas are rare, the findings highlight an important risk factor that women and their healthcare providers may want to consider when discussing contraceptive options.
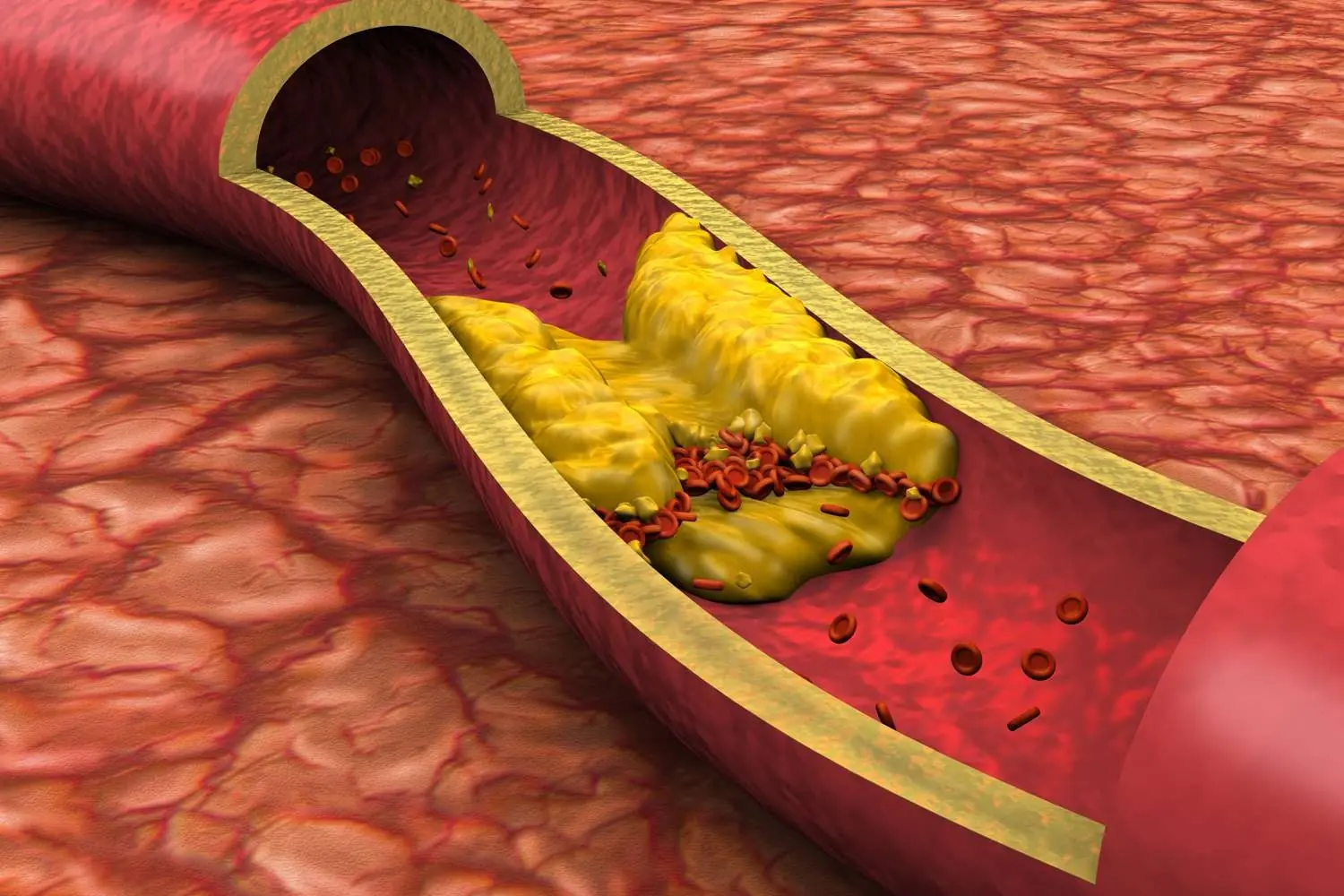
Meningiomas are the most common primary brain tumor, typically arising from the membranes that cover the brain and spinal cord. Although they are often benign, their location can still cause serious health problems. According to the new analysis led by Dr. Varun Kshettry of the Cleveland Clinic, women who used depot medroxyprogesterone acetate faced a relative risk (RR) of 2.43 (95% CI 1.77-3.33) compared with women who did not use hormonal contraceptives.
The risk was particularly pronounced in women who had been exposed to the injectable contraceptive for more than four years or who started using it after age 31. Oral medroxyprogesterone acetate also carried some risk, but to a much smaller extent (RR 1.18, 95% CI 1.10-1.27). By contrast, other contraceptives — such as combined oral contraceptives, intrauterine devices (IUDs), progestin-only pills, and subdermal implants — showed no increased risk of meningioma.
Dr. Kshettry emphasized that the results could be especially valuable during risk-benefit conversations for women who may already be at higher risk of brain tumors. This includes individuals with a family history of meningioma, prior cranial radiation, or certain genetic conditions such as neurofibromatosis type II.
Why Hormones May Play a Role
Experts believe that hormones, particularly progesterone, could be key in understanding why meningiomas appear more frequently in women. Over 60% of meningiomas express progesterone receptors, and tumor size often grows during periods of higher hormone levels such as pregnancy or childbearing years. As Dr. Gilles Reuter of the Centre Hospitalier Universitaire de Liège and Dr. Britta Wandschneider of University College London explained, the data points to a “biological relationship” between sex hormones and tumor development.
The Scope of the Study
The research team examined data from the U.S. TriNetX database, covering 10,425,438 women across 68 healthcare organizations between 2004 and 2024. Importantly, only women with no prior history of meningioma were included, and groups were carefully matched for age, race, health history, and other factors.
Among women using depot medroxyprogesterone acetate, the incidence of meningioma was 7.39 per 100,000 patient-years, compared with 3.05 per 100,000 patient-years in matched controls. This translates to an attributable risk of 59%. The number needed to harm (NNH) was calculated at 1,152 women for depot medroxyprogesterone acetate — meaning one additional case of meningioma could be expected for every 1,152 women using this contraceptive. For oral medroxyprogesterone acetate, the NNH was 3,020 women.
Interestingly, the study also found a decreased risk of meningioma among women using combined oral contraceptives (RR 0.74), IUDs (RR 0.87), and the 52 mg levonorgestrel-releasing IUD (RR 0.79), suggesting that not all hormonal methods carry the same risk.
What This Means for Women
Although the findings are significant, researchers caution that the study is observational and based on insurance coding data, which may not capture every factor influencing brain tumor development. Still, the evidence adds weight to earlier research, including a 2024 French study that also found a potential link between injectable medroxyprogesterone acetate and increased tumor risk.
For women, the key takeaway is not panic, but informed decision-making. If you are currently using or considering depot medroxyprogesterone acetate, it may be worth having a discussion with your doctor about your individual risk factors and whether another contraceptive option may be a safer choice for you.
While meningiomas remain uncommon, this research suggests that some forms of hormonal contraception — particularly long-term injectable Depo-Provera — may raise the risk more than previously understood. Open conversations between women and healthcare providers are essential to balance effectiveness, convenience, and potential long-term health risks.