The new vitamin D findings forcing experts to rethink heart health
Could something as simple and inexpensive as vitamin D be a missing piece in the fight against heart attacks and strokes? For years, vitamin D has been surrounded by excitement, skepticism, and scientific debate. It’s been linked to everything from immune strength to bone density, and even lower cancer rates in early research. Yet when it comes to heart health, the story has been tangled—full of conflicting results and unanswered questions.
Now, a new clinical trial is challenging long-held assumptions and prompting doctors to take a second look at this humble nutrient. If you’ve ever wondered whether you should check your vitamin D levels or whether supplements actually make a difference, this updated look at the evidence—based on the analysis of Dr. Brad Stanfield—is essential reading.
Key Takeaways
-
Early research linked low vitamin D levels with higher rates of many chronic diseases.
-
Large, rigorous trials that followed later did not show major benefits of general vitamin D supplementation.
-
A new study—the TARGET D trial—looked at high-risk heart patients and found intriguing, unexpected findings.
-
While overall results were mixed, there was a significant drop in repeat heart attacks in the vitamin D–managed group.
-
The debate about routine vitamin D testing and supplementation is far from settled, but the conversation is shifting.
1. The Early Excitement: Vitamin D Deficiency as a Public Health Crisis
Ten to fifteen years ago, vitamin D was hailed as a breakthrough. Observational studies repeatedly showed that people with low vitamin D levels had higher rates of:
-
heart disease
-
cancer
-
infections
-
autoimmune conditions
-
type 2 diabetes
-
depression
It seemed like a miracle nutrient. As these findings spread, vitamin D testing skyrocketed. Millions of people began supplementing daily, sometimes with extremely high doses, in hopes of preventing long-term disease.
But there was a problem: correlation doesn’t prove causation. People who are sicker often stay indoors more, exercise less, and get less sunlight—factors that lower vitamin D levels. Scientists needed to know whether low vitamin D actually caused disease, or whether it was just a marker of poor health.
2. The Reality Check: Large Trials Fail to Show Big Benefits
To answer this, researchers ran large, expensive, randomized clinical trials. The most famous, the VITAL trial, followed over 25,000 adults for years. Its results were sobering:
-
Vitamin D supplementation did not significantly reduce heart attacks.
-
It did not reduce strokes.
-
It did not lower cancer rates.
After these findings, expert groups—including the Endocrine Society—scaled back their recommendations. Routine vitamin D screening for healthy adults was no longer encouraged. Most people, they said, only needed about 800 IU a day, primarily for bone health.
This was a major turning point. The “vitamin D cures everything” narrative faded almost overnight.
3. The Plot Twist: The TARGET D Trial Reopens the Discussion
The new TARGET D trial took a very different approach. Instead of studying the general population, researchers focused on people at extremely high cardiovascular risk—especially those who had recently suffered a heart attack.
They measured each participant’s vitamin D level and discovered that most were on the low side. Then they split the group:
-
Intervention group: Given personalized vitamin D doses adjusted to reach a target blood level above 40 ng/mL.
-
Control group: Received standard care with no vitamin D targeting.
Researchers followed the participants for four years, adjusting supplement doses regularly to keep levels in the desired range. This individualized approach set the study apart from past trials.
4. Mixed Results Overall—But One Finding Stands Out
When all cardiovascular events were combined—heart attack, stroke, hospitalization for heart failure, or death—the difference between the two groups wasn’t statistically significant.
However, when researchers looked specifically at repeat heart attacks, something unexpected emerged:
-
Patients whose vitamin D levels were optimized had about a 52% lower risk of having another heart attack.
-
This translated to approximately four fewer repeat heart attacks per 100 people over four years.
That might sound small, but for high-risk patients, even a modest reduction can be life-changing.
5. Why This Study Is Different: Personalized Dosing Matters
Unlike previous trials that gave a flat dose to everyone, the TARGET D study attempted to fix true deficiencies. This raises an important possibility:
Maybe vitamin D only helps the heart when people who actually need it restore their levels to the right range.
In past research, many participants already had normal vitamin D or were given doses too low to make a meaningful difference. By targeting specific blood levels, the new study offered a more precise test of vitamin D’s impact.
6. But Don’t Get Carried Away: Important Limitations
Despite the exciting findings, caution is still essential.
-
The study was not blinded, meaning participants and doctors knew who received supplementation.
-
This increases the possibility of placebo effects or behavior changes.
-
The main combined outcome did not reach statistical significance.
-
The reduction in repeat heart attacks could be due to chance, especially in subgroup analysis.
In addition, some trends in the data suggested a potential increase in heart failure and stroke rates in the vitamin D group—though these were not statistically significant. It highlights how complex the body’s hormone systems are.
More is not always better.
7. Potential Risks of Overdoing Vitamin D
Vitamin D is often seen as harmless, but high levels can carry risks. Excessive supplementation may lead to:
-
elevated calcium levels
-
kidney stones
-
abnormal heart rhythms
-
hormonal imbalance
Because vitamin D is stored in body fat and acts like a hormone, overshooting the ideal range could have unintended effects.
This is why experts advise avoiding high-dose supplements unless medically supervised.
8. What Do Experts Currently Recommend?
Medical guidelines have not changed in light of this new research. For the average adult:
-
Routine testing is not recommended.
-
Standard supplementation of 800 IU/day is considered adequate for most people.
-
Higher doses may be appropriate for those with known deficiency or certain conditions, under medical guidance.
The TARGET D trial is thought-provoking, but not definitive enough to rewrite national guidelines—at least not yet.
9. So What Should YOU Do? Individualize Your Approach
If you have a history of heart disease—especially a recent heart attack—this study may be worth discussing with your doctor. A targeted strategy, including a blood test and personalized supplementation, could be reasonable.
For everyone else, focusing on:
-
moderate sun exposure
-
a balanced diet
-
avoiding extreme doses
remains the safest and most evidence-based approach.
10. What This Means Moving Forward
As Dr. Brad Stanfield points out, vitamin D still has an air of mystery around it. It interacts with inflammation, immune health, muscle function, and even hormonal regulation. Scientists are still figuring out how all these pieces fit together.
For now, the best approach is:
-
stay informed
-
follow credible evidence
-
personalize decisions to your risk level
More research is already underway, and future trials may clarify whether vitamin D has a targeted role in cardiovascular prevention.
News in the same category

The 11 Surprising Baking Soda Uses Backed by Real Science
The Unexpected Link Between Morning Blood Flow and a Stronger, Healthier Heart
Cleanse Your Kidneys of Toxins With 2 Effective 1-Ingredient Drinks
What really happens to your body when you take LOSARTAN

#1 Best Way to Lower Blood Pressure Naturally and Fast
Coconut Water Found To Lower Blood Pressure By As Much As 71% In Study Participants

The Secret to Perfectly Juicy Sausages Every Time
12 Early Warning Signs of Dementia You Shouldn’t Ignore
15 visible signs of low thyroid you can see – don’t ignore #7!

The 4 hidden causes of persistent phlegm in your throat (& how to fix it naturally)
How to shrink thyroid nodules naturally with 2 key minerals

10 supplement combinations you should never take together

Common pain meds trick doctors into heart failure misdiagnosis

The Military Sleep Method

Eating boiled eggs regularly: “good for the liver” or “harmful”? Doctor explains 3 key points to remember

Heart surgeon warns people should remove this one thing from their life after turning 40
Top 6 Neuropathy Remedies (Peripheral Neuropathy Home Remedies)
10 daily habits that are silently destroying your kidneys
News Post

Doctors Reveal: What Really Happens to Your Body When You Eat Soaked Almonds — The Surprising Effects

7 Days, 2 Ingredients, Big Results: What Really Happens When You Take Garlic and Honey on an Empty Stomach

Thyme Tea for Circulation and Joint Health: Benefits, Recipe, and How to Use It

Burn a single clove of garlic for 15 minutes—and witness the surprising shift in flavor, energy, and hidden benefits it awakens

Could your morning orange juice be supporting your heart more than you think?
The 11 Surprising Baking Soda Uses Backed by Real Science
The Unexpected Link Between Morning Blood Flow and a Stronger, Healthier Heart
Cleanse Your Kidneys of Toxins With 2 Effective 1-Ingredient Drinks

The Science Behind Cats’ Calming Influence on Stress and Heart Health
12 Phrases That Reveal Someone Is Struggling More Than They Want To Admit
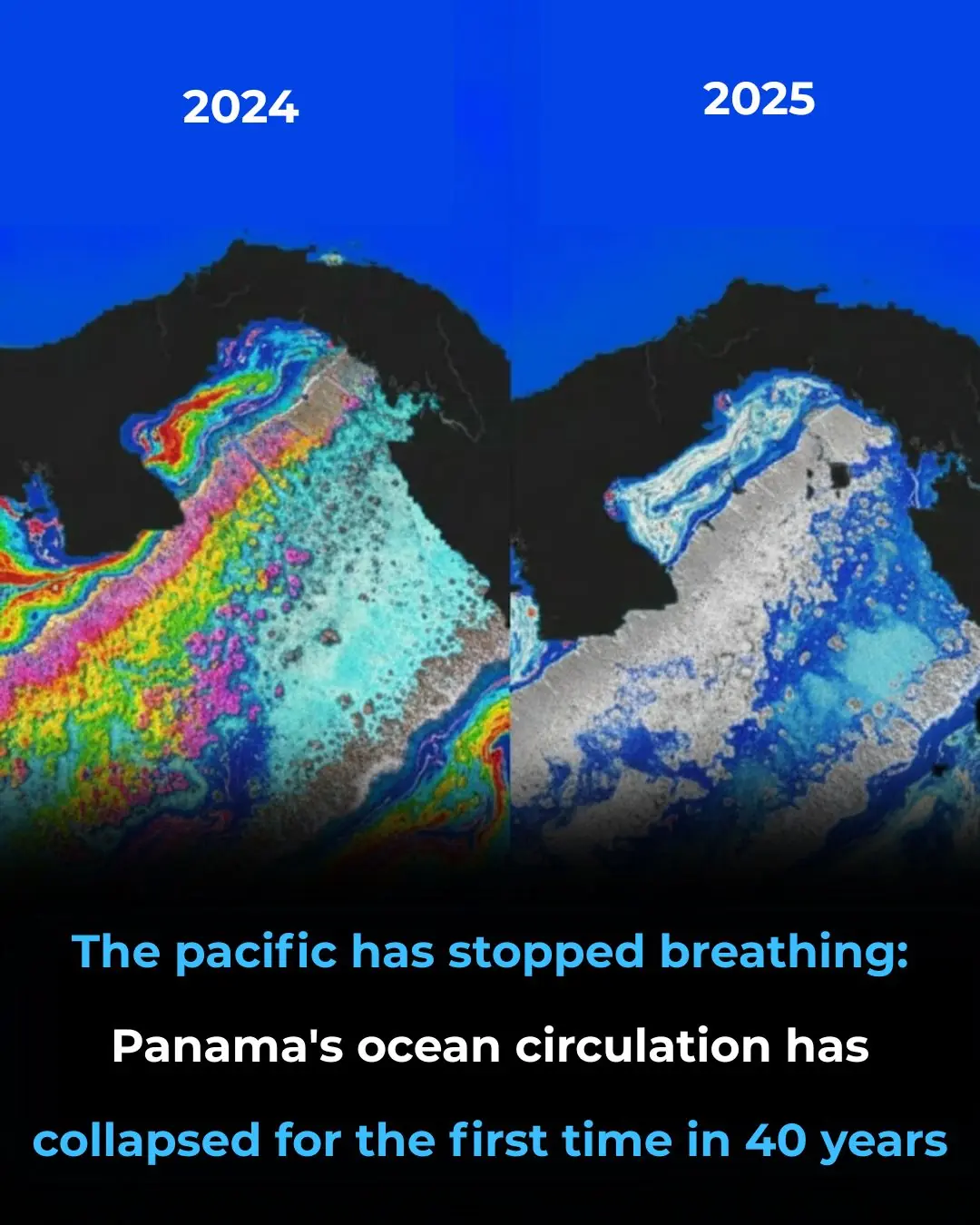
For the first time in 40 years, Panama’s Ocean lifeline has vanished

The Meaning Behind the WC Toilet Sign

How to cook fish soup with vegetables, delicious and sweet in summer
What really happens to your body when you take LOSARTAN

The rice cooker has a special part, easy to clean and saves millions of dong every month.

Turn on the electric fan on a hot summer day: Spray this and the room will be as cool as air conditioning.

#1 Best Way to Lower Blood Pressure Naturally and Fast
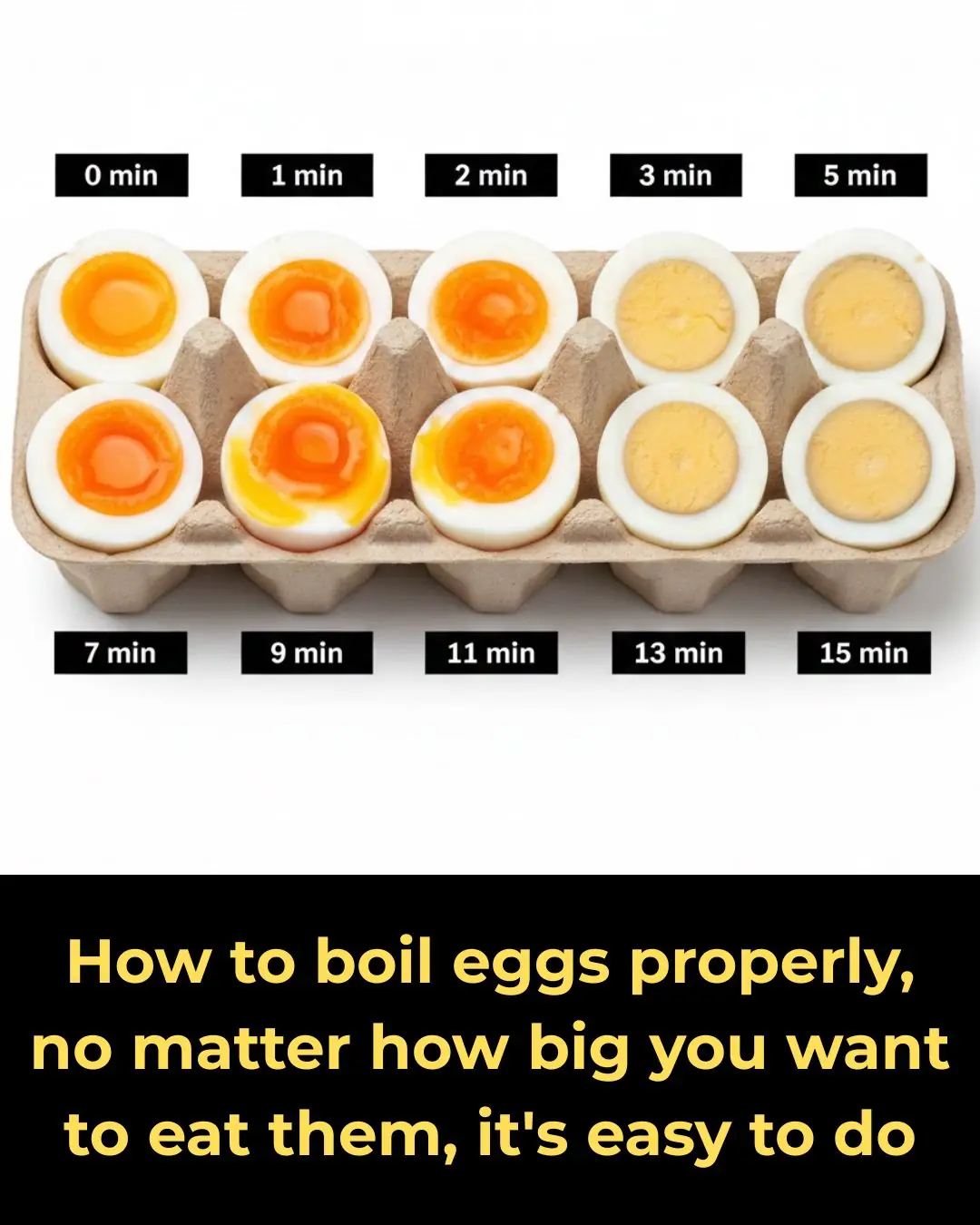
How to boil eggs properly, no matter how big you want to eat them, it's easy to do

Going to the market to buy squash: Should you choose dark or light green skin?