
Vaccines and Healthy Aging: Benefits That Go Beyond Infection Prevention

Vaccination has long been recognized as one of the most effective tools in modern medicine for preventing infectious diseases. For older adults, vaccines against influenza, pneumococcal disease, shingles, COVID-19, and respiratory syncytial virus (RSV) are routinely recommended to reduce the risk of severe illness and death. However, growing evidence suggests that the benefits of vaccination in older populations extend well beyond protection from infection alone.
Recent studies indicate that recommended vaccines for older adults are associated with lower rates of hospitalization, reduced complications from chronic disease, and improved overall health outcomes. These findings are reshaping how experts view vaccination—not merely as a defensive measure against specific pathogens, but as a broader strategy to promote healthy aging.
Beyond Infection: A Broader Protective Effect
Traditionally, the success of vaccines has been measured by their ability to prevent illness or reduce disease severity. While this remains a core benefit, researchers are increasingly observing “off-target” or indirect effects of vaccination, particularly in older adults.
Multiple observational studies have shown that vaccinated older individuals experience fewer hospital admissions, not only for infections but also for cardiovascular events, respiratory complications, and functional decline. For example, influenza vaccination has been linked to a lower risk of heart attacks and strokes, especially during flu season. Similarly, pneumococcal vaccination has been associated with reduced rates of pneumonia-related complications and long-term disability.
These findings suggest that vaccines may help stabilize health in older adults by preventing the cascade of complications that often follow infections in this age group.
Why Vaccines Matter More With Age
As people age, their immune systems undergo gradual decline, a process known as immunosenescence. This makes older adults more vulnerable to infections and less able to recover quickly once illness occurs. Even mild infections can trigger serious consequences, such as worsening heart disease, diabetes complications, or loss of independence.
Vaccines help reduce this vulnerability by lowering the risk of infection and dampening the inflammatory response that can destabilize chronic conditions. By preventing infections that often act as “stress tests” for the aging body, vaccination helps preserve physical function, cognitive health, and overall resilience.
Reducing Hospitalization and Healthcare Burden
Hospitalization can be particularly harmful for older adults. Extended hospital stays are associated with muscle loss, delirium, falls, and long-term functional decline. Studies now show that vaccinated older adults are less likely to require hospitalization, even when infections do occur.
This reduction in hospital admissions not only benefits individuals but also eases pressure on healthcare systems. Fewer hospitalizations mean lower healthcare costs, reduced strain on caregivers, and improved quality of life for older patients who can remain active and independent in their communities.
Vaccination and Chronic Disease Management
Another important finding from recent research is the relationship between vaccination and better outcomes in people with chronic diseases. Older adults often live with conditions such as heart disease, chronic lung disease, kidney disease, or diabetes. Infections can significantly worsen these conditions, leading to rapid deterioration.
Vaccination helps interrupt this cycle. By preventing infections that exacerbate chronic illness, vaccines indirectly support long-term disease management. Some researchers suggest that consistent vaccination may help slow functional decline and reduce the risk of disability in older age.
Supporting the Concept of Healthy Aging
Healthy aging is not just about living longer—it is about maintaining physical, mental, and social well-being for as long as possible. Vaccination plays a key role in this goal by protecting older adults from illnesses that can permanently alter their quality of life.
Preventing shingles, for example, reduces the risk of chronic nerve pain that can persist for years. Preventing severe respiratory infections lowers the likelihood of long-term breathing problems or reduced mobility. These outcomes directly support independence, autonomy, and healthy aging.
Addressing Vaccine Hesitancy in Older Adults
Despite strong evidence of benefit, vaccine uptake among older adults remains uneven. Concerns about side effects, doubts about effectiveness, and misinformation continue to influence decision-making. Experts emphasize that clear communication about the broader benefits of vaccination—beyond infection prevention—may help improve acceptance.
Healthcare providers play a critical role in discussing how vaccines support overall health, reduce hospitalizations, and protect independence. Framing vaccination as part of a comprehensive healthy-aging strategy may resonate more strongly than focusing solely on disease prevention.
A Shift in Perspective
The growing body of evidence reinforces the idea that vaccines are not just tools to fight infections, but essential components of preventive care for older adults. By reducing hospitalizations, protecting against complications, and supporting chronic disease stability, vaccination contributes to longer, healthier, and more independent lives.
As researchers continue to explore the full impact of vaccines on aging, one message is becoming clear: staying up to date with recommended vaccines is one of the simplest and most effective ways to invest in health later in life—not just to avoid illness, but to age well.
News in the same category


11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?

Surprise Finding: How the Immune System May Prevent Us From Burning Fat
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

The Best Time to Drink Pomegranate Juice for Blood Pressure and Muscle Recovery
Why Your Cat Chooses to Sleep With You

10 Conditions Ginger Can Help Manage Naturally

How Often Do You Poop? New Research Shows Bowel Movement Frequency Linked to Overall Health

What Happens to Your Blood Pressure When You Drink Beetroot Juice Every Day

Signs and Symptoms of Oral Cancer

Obesity Is a Disease: Understanding Its Biology and Cardiovascular Impact

Exercise Linked to Better Outcomes in Patients With Hypertension

Adding Yoga to Opioid Use Disorder Care May Speed Recovery From Opioid Withdrawal

Sunlight at Work Beats Artificial Light for Glucose Control in Type 2 Diabetes

Bariatric Surgery or GLP-1 Receptor Agonists? Long-Term Effects on Fat Loss and Body Composition

If You Have Fig Leaves, You Have Gold—and You Didn’t Even Know It
News Post

Choosing Compassion Over Cameras: A Young Man Saves a Shark by Removing a Fishhook

Abandoned at One Year Old: The Heartbreaking Reality Behind a Chihuahua Left at a Shelter

Pets Are Not Disposable: A Lifelong Commitment, Not a Temporary Choice

The 400-Year-Old Greenland Shark: One of the Oldest Living Vertebrates on Earth
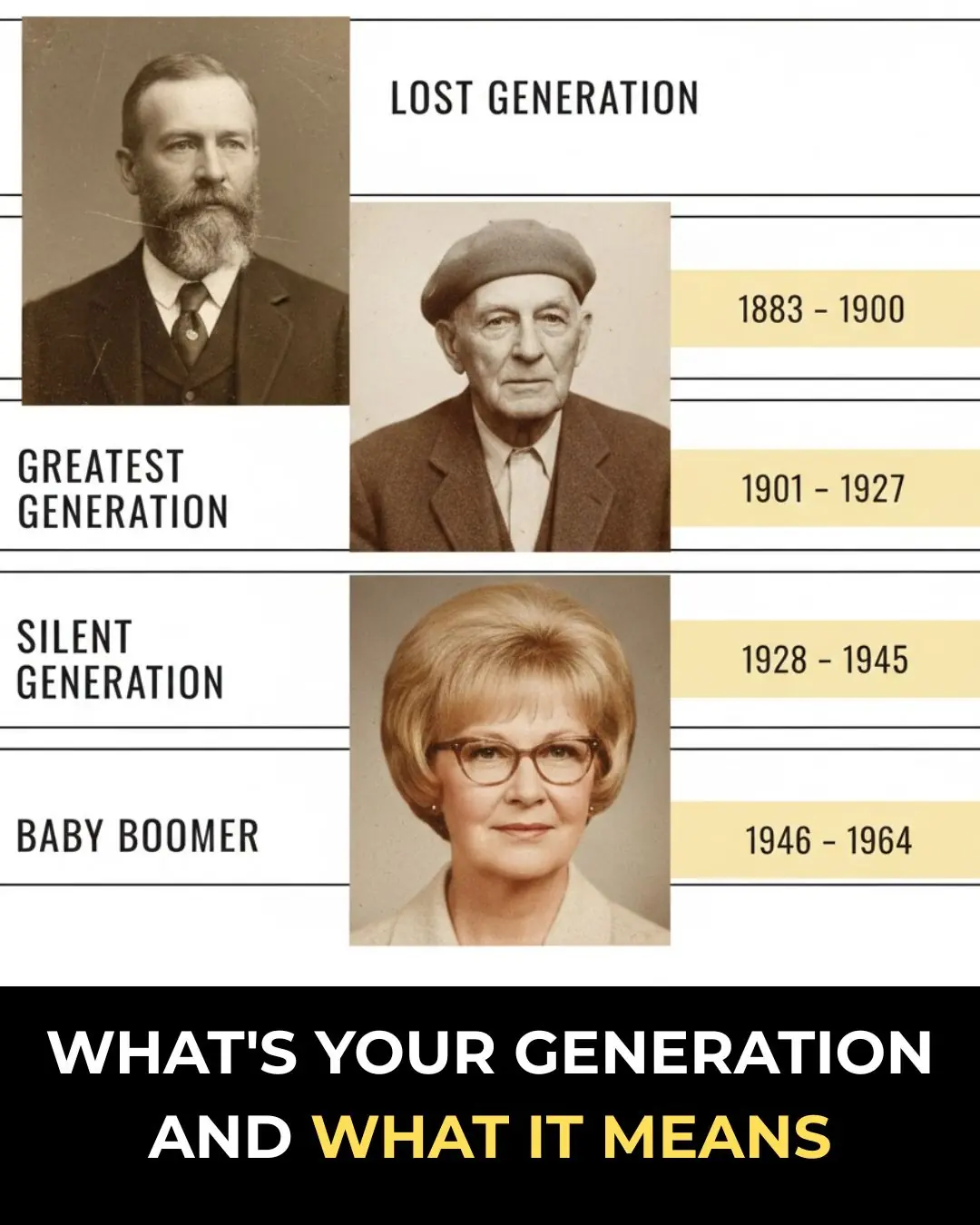
What’s Your Generation and What It Means

Drink Coconut Water for 7 Consecutive Days and Notice Remarkable Health Benefits

11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?

Surprise Finding: How the Immune System May Prevent Us From Burning Fat
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

Bula Choudhury: A Masterclass in Resilience and the Quiet Pursuit of Greatness 🌊✨

Targeted Violence in Khulna: A Growing Crisis for Law and Order ⚠️🇧🇩

When One Moment Changes Everything: A Story of Love, Trust, and Betrayal 🎶⚡💔

Mukesh Ambani’s Vision: Powering India’s Olympic Dream for 2036 🇮🇳✨🏟️

Love’s Second Chance: Jayaprakash and Rashmi’s Heartwarming Reunion 💛✨

🚫 5 Dangerous Items You Should NEVER Store Under Your Kitchen Sink (One Could Poison Your Family)
