Curcumin Shows Promise in Helping Ulcerative Colitis Patients Achieve Remission
A systematic review and meta-analysis published in the Journal of Ethnopharmacology in 2022 evaluated the potential role of curcumin as an adjunct therapy in the management of ulcerative colitis (UC). The analysis included six randomized controlled trials comprising a total of 385 patients diagnosed with UC. The findings showed that patients who received curcumin in addition to standard conventional treatment were significantly more likely to achieve clinical remission compared with those receiving control or placebo treatments. Specifically, the pooled results demonstrated a relative risk of 2.10 (95% confidence interval: 1.13–3.89), indicating more than a twofold increase in the likelihood of remission when curcumin was used as an add-on therapy.
Despite these promising results for clinical remission, the meta-analysis did not identify statistically significant benefits in several other important clinical outcomes. No clear improvements were observed in overall clinical response rates, endoscopic remission, or endoscopic improvement. These findings suggest that while curcumin may help alleviate symptoms and support remission at a clinical level, its effects on intestinal mucosal healing remain uncertain based on the currently available evidence.
The authors emphasized that several factors may substantially influence the therapeutic efficacy of curcumin in UC. These include dosage, formulation, bioavailability, route of administration (such as oral versus topical delivery), and the duration of treatment. Curcumin is known to have limited oral bioavailability due to poor absorption and rapid metabolism, a challenge that has been widely discussed in pharmacological research. Previous studies have suggested that enhanced formulations, such as curcumin combined with piperine or delivered through nanoparticle or phospholipid-based systems, may improve systemic and local anti-inflammatory effects (Hewlings & Kalman, Foods, 2017; Nelson et al., Molecules, 2017).
Importantly, the 2022 review also reported that curcumin was generally well tolerated among UC patients. Across the included trials, no severe adverse events were attributed to curcumin supplementation, supporting its favorable safety profile when used alongside conventional therapies such as aminosalicylates. This observation aligns with assessments by authoritative institutions, including the U.S. National Institutes of Health (NIH), which recognizes curcumin as a compound with a strong safety record in human studies, even at relatively high doses.
The authors concluded that while current evidence supports a beneficial role for curcumin in promoting clinical remission in ulcerative colitis, the overall strength of evidence remains moderate. They highlighted the need for larger, well-designed randomized controlled trials with standardized dosing regimens, improved formulations, and longer follow-up periods. Such studies are necessary to clarify curcumin’s impact on endoscopic outcomes, mucosal healing, and long-term disease progression. These recommendations are consistent with broader perspectives in gastroenterology research, including reviews published in The Lancet Gastroenterology & Hepatology and clinical discussions by organizations such as the European Crohn’s and Colitis Organisation (ECCO), which continue to explore complementary therapies as potential adjuncts—not replacements—to standard inflammatory bowel disease treatment.
In summary, curcumin appears to be a safe and potentially effective adjunct therapy for improving clinical remission in ulcerative colitis. However, further rigorous investigation is essential to define its optimal use and establish its role in comprehensive, evidence-based UC management strategies.
Building on these findings, growing interest in curcumin also reflects a broader shift toward integrating evidence-based complementary therapies into conventional ulcerative colitis management. Chronic inflammation in UC is driven by complex immune dysregulation involving pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and nuclear factor kappa B (NF-κB). Experimental and clinical research has shown that curcumin can modulate several of these inflammatory pathways, which may help explain its observed effects on symptom control and remission induction. Reviews published in journals such as Nature Reviews Gastroenterology & Hepatology have highlighted curcumin’s capacity to inhibit NF-κB activation and reduce oxidative stress, both of which are key contributors to intestinal inflammation and epithelial damage in UC.
Moreover, patient interest in curcumin is often driven by concerns about the long-term safety of conventional medications, including corticosteroids and immunosuppressants. While these drugs remain essential for disease control, long-term use can be associated with adverse effects. In this context, curcumin’s favorable safety profile makes it an attractive adjunctive option rather than a substitute for standard therapy. Clinical guidance from organizations such as the Mayo Clinic and Cleveland Clinic has increasingly acknowledged that certain dietary supplements may have a supportive role when used under medical supervision, particularly in patients with mild to moderate disease.
Another important consideration is treatment personalization. Ulcerative colitis is a heterogeneous condition, and patient responses to both pharmacological and complementary therapies vary widely. The lack of consistent endoscopic benefits observed in current trials may reflect differences in disease severity, baseline inflammation, or treatment duration among study participants. Longer trials with stratification by disease activity and standardized outcome measures could help identify subgroups of patients who are most likely to benefit from curcumin-based interventions.
In the long term, future research may also explore the synergistic effects of curcumin with other therapies, including probiotics, dietary interventions, or biologic agents. As interest in gut microbiota modulation grows, emerging evidence suggests that curcumin may influence microbial composition and intestinal barrier function, offering another potential mechanism of benefit. Such hypotheses are currently under investigation in translational studies and early-phase clinical trials reported by institutions such as Harvard Medical School and research networks affiliated with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Overall, while curcumin cannot yet be considered a standalone or definitive treatment for ulcerative colitis, accumulating evidence supports its role as a promising adjunct to standard care. Continued high-quality research will be essential to establish clear clinical guidelines, optimize formulations and dosing strategies, and determine whether curcumin can contribute meaningfully to sustained remission, mucosal healing, and improved quality of life for patients living with UC.
News in the same category

Understanding Ringworm: Causes, Symptoms, Transmission, and the Importance of Medical Evaluation
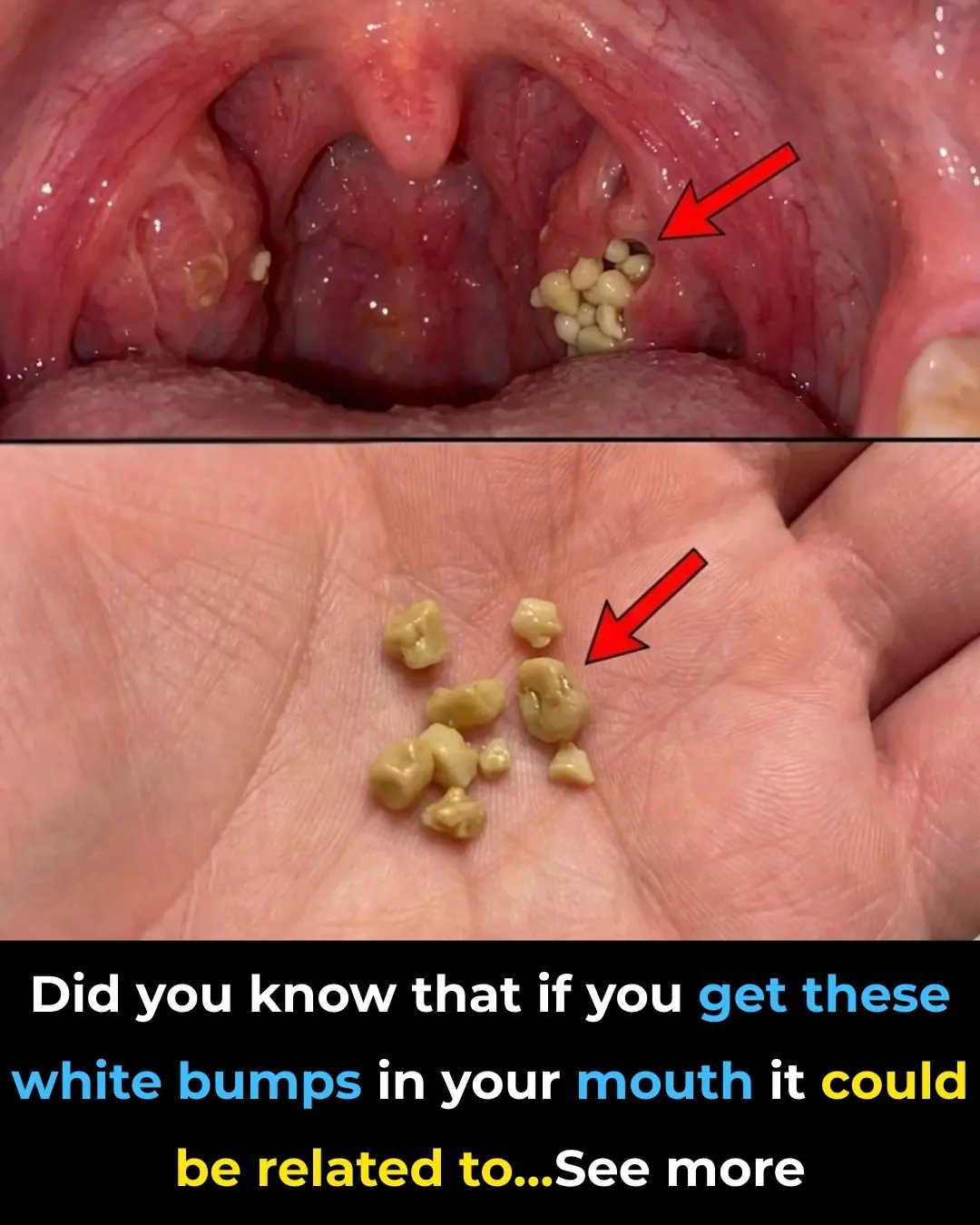
Tonsil Stones: Discover what they are, how they appear, and how to get rid of them forever.

Understanding Menstrual Cramps: Causes, Symptoms, and When to Seek Medical Help

🧪 The Breakthrough Procedure

🔬 How Vaccines May Boost Broader Immunity

🔬 How mRNA Cancer Therapy Works

🧪 Historical Context: Sugar vs. Fat in Nutrition Science

🧪 The Breakthrough in Switzerland

Pineapple and Cucumber: A Natural Gut Health Remedy

Lyme disease: causes, natural treatment, and how to effectively prevent it

Understanding Vitiligo: Causes, Diagnosis, and the Importance of Medical Evaluation

Understanding Ovulation: Key Signs Your Body Sends and Why They Matter

Why Do Men Lose Their Hair? The Story Behind Every Follicle
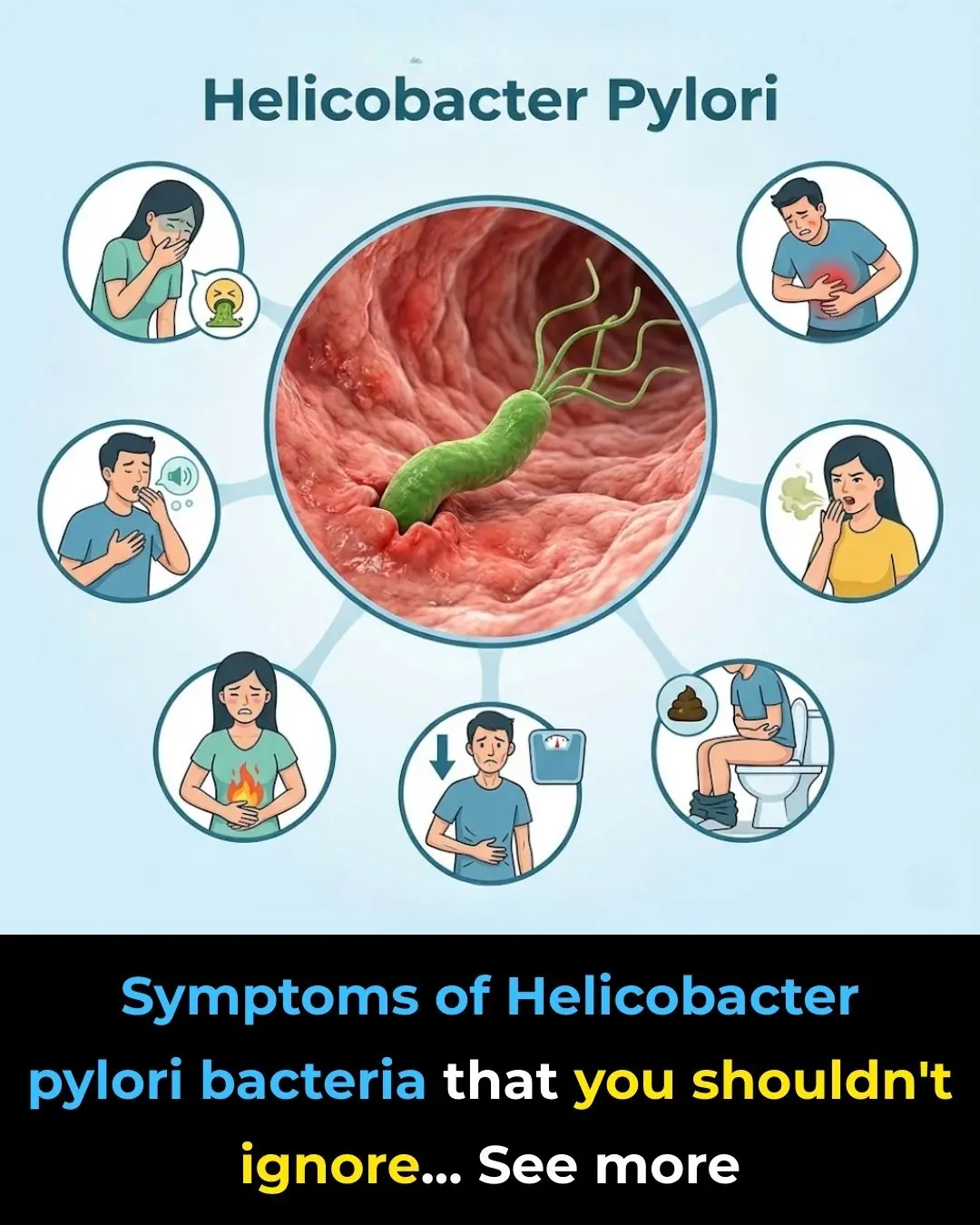
Muña vs. Gastritis: Peruvian scientist demonstrates its power against the Helicobacter pylori bacteria

Early Menopause: Recognizing the Signs, Understanding the Risks, and Steps You Can Take

"What Are These Spots in the Image? 🤔"

Genital Herpes vs Folliculitis: Understanding the Difference 👩🏻⚕️
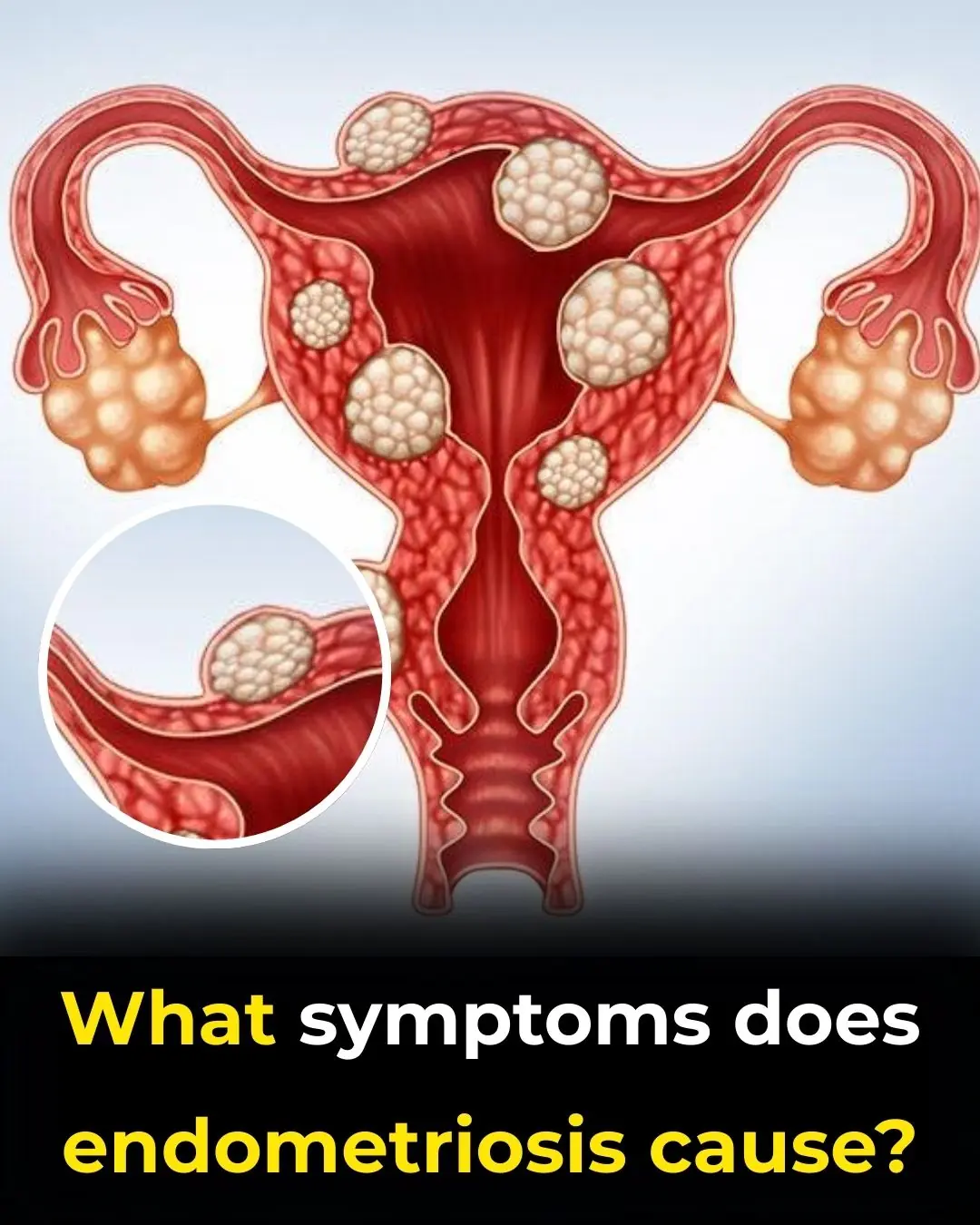
Understanding Endometriosis: Symptoms, Diagnosis, and the Importance of Early Detection with Dr. Pau Zúñiga
News Post
A study shows that oxytocin, the ‘love hormone,’ can help regenerate the heart after injury.

At my family’s public gala, my brother’s fiancée snatched my inherited pearl necklace and sneered

A Powerful Woman Pushes a Child into a Puddle — But the Birthmark on His Hand Leaves Her Stunned…
Health Benefits of Coffee
The Lack of This Mineral Is Causing Age Spots: Discover the Solution
Warning For Pink Slime Found in Your Bathroom

Understanding Ringworm: Causes, Symptoms, Transmission, and the Importance of Medical Evaluation

The Helmet That Started Breathing at Night
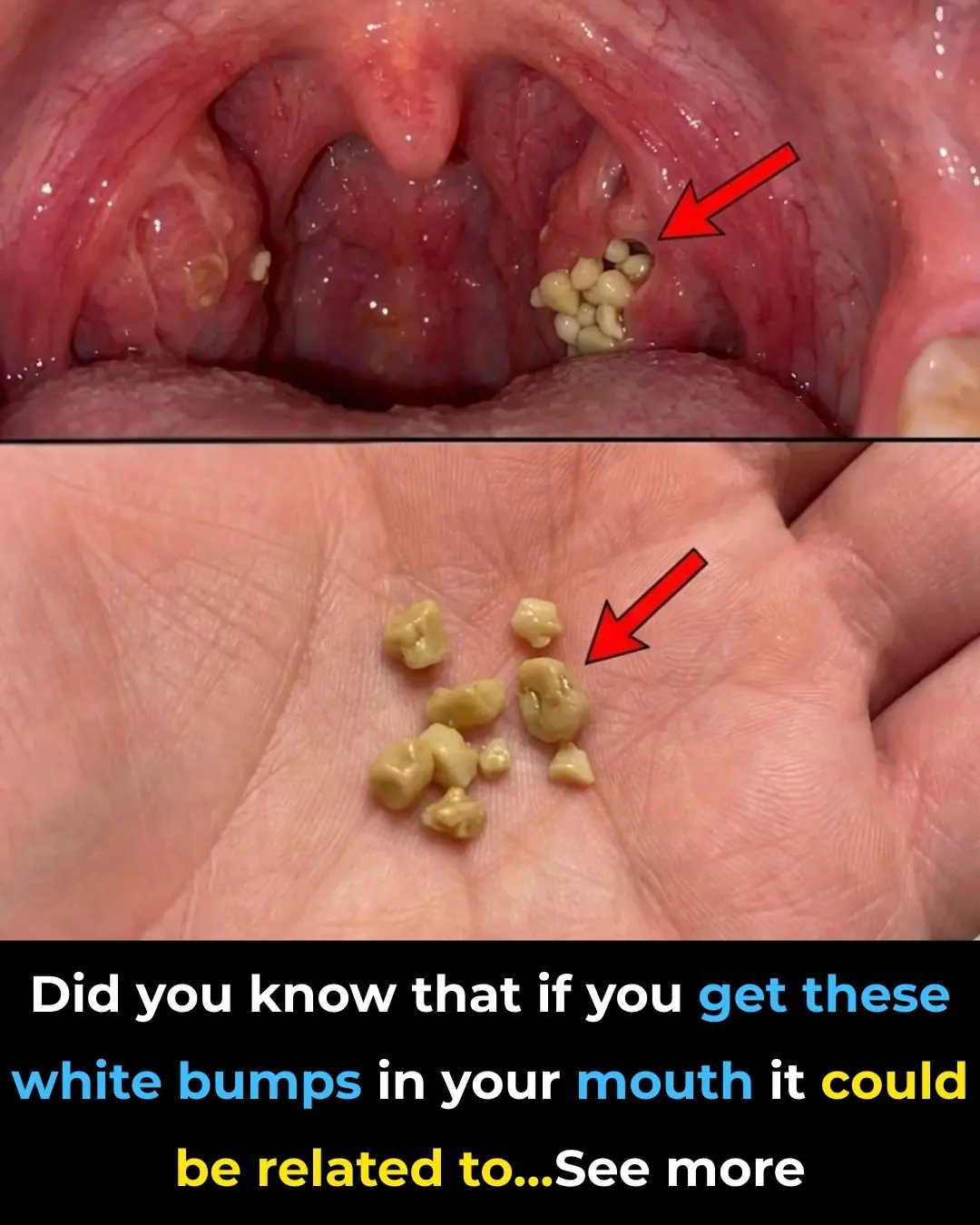
Tonsil Stones: Discover what they are, how they appear, and how to get rid of them forever.

Understanding Menstrual Cramps: Causes, Symptoms, and When to Seek Medical Help

Black CEO Removed from VIP Seat for White Passenger – 5 Minutes Later The Entire Crew Gets Fired
Morgan Freeman Slams Unauthorized AI Voice Use, Says His Lawyers Are “Busy”

Beloved Florida pastry chef, 71, killed in freak accident with bread-making machine

He Left His Wedding to Save a Country

He Erased His Wife from the Billionaire Gala—Until the Entire Room Rose When She Walked In

Meghan Markle and Prince Harry reunite with Hollywood PR firm after 11th publicist quit

🥊 What Mary Kom Said

🕊️ The Incident
