
These red patches flare up every night, but my doc can’t see me until next month. Any idea what’s happening?

Experiencing red patches on your skin that flare up night after night can be both unsettling and exhausting—especially when your doctor’s appointment is still weeks away. These recurring flare-ups don’t just affect your skin; they can interrupt your sleep, increase stress, and leave you constantly wondering what’s going wrong. The uncertainty alone can make the situation feel worse than the symptoms themselves.
While waiting to see a healthcare professional, learning more about potential causes and gentle ways to calm your skin can give you a sense of control. Nighttime skin reactions are often influenced by a combination of internal processes and external triggers. This article explores why symptoms may worsen after dark, what conditions could be responsible, what patterns to watch for, and how to soothe your skin safely until you receive medical advice.
1. Why Your Skin Reacts More Strongly at Night
Your skin naturally behaves differently at night due to the body’s circadian rhythm. During evening hours, levels of cortisol—a hormone with anti-inflammatory effects—drop significantly. With less cortisol circulating, your skin may become more reactive to irritation, allergens, or existing inflammation.
At the same time, the skin’s protective barrier tends to weaken overnight, leading to increased moisture loss. This process, known as transepidermal water loss, can leave skin drier, itchier, and more vulnerable. As a result, conditions like eczema and dermatitis often feel far more intense once you lie down to sleep.
2. Could It Be Eczema? Common Symptoms to Watch For
Eczema, also called atopic dermatitis, is one of the most common causes of nighttime skin flare-ups. It typically appears as red, inflamed patches that itch intensely—often more so in the evening. The skin may feel rough, dry, or scaly, and in some cases, it can ooze or form crusts.
Although eczema is frequently associated with childhood, many people develop it later in life. Genetics, environmental exposures, immune responses, and a weakened skin barrier all play a role. If your symptoms follow a recurring nighttime pattern with significant itching, eczema is a strong possibility.
3. Nighttime Triggers: Heat, Sweat, and Bedding Choices
Your sleeping environment can have a major impact on your skin. Excess heat and sweat are common triggers for irritation, particularly if you’re using thick blankets or sleeping in a warm room. Sweat trapped against the skin can worsen inflammation and itching.
Switching to lightweight, breathable bedding made from cotton or bamboo may help. Keeping your bedroom cool—ideally between 60 and 67°F (15–19°C)—can reduce sweating and make both your skin and sleep more comfortable.
4. How Stress, Anxiety, and Poor Sleep Affect Your Skin
Emotional stress doesn’t stay in your head—it shows up on your skin. Stress activates inflammatory pathways in the body, which can intensify redness, itching, and flare-ups. Anxiety can also make you more aware of itching, creating a cycle that’s hard to break.
Poor sleep further compounds the problem by limiting your body’s ability to repair the skin overnight. Gentle stress-management techniques such as deep breathing, journaling, or light stretching before bed can help calm your nervous system and support skin recovery.
5. Hidden Irritants in Detergents and Fragrances
Many everyday household products contain ingredients that irritate sensitive skin. Laundry detergents, fabric softeners, and scented sprays may leave residue on clothing and bedding, causing prolonged contact with irritants during sleep.
Choosing fragrance-free, hypoallergenic products can make a noticeable difference. Double-rinsing laundry and avoiding dryer sheets may also reduce irritation. If you recently switched products, that change alone could explain new nighttime symptoms.
6. Daily Habits That May Be Making Symptoms Worse
Hot showers and harsh soaps can strip your skin of its natural oils, weakening its protective barrier. While a hot shower may feel relaxing, it often worsens dryness and inflammation afterward.
Opt for lukewarm water and gentle, soap-free cleansers instead. Applying a thick, fragrance-free moisturizer within minutes of bathing helps seal in moisture and protect your skin throughout the night.
7. Food Sensitivities and Allergies
For some people, skin flare-ups are linked to food sensitivities or allergies. Certain foods—such as dairy, gluten, shellfish, nuts, or eggs—can trigger immune responses that appear as skin inflammation hours later.
Keeping a food and symptom diary may help identify patterns. Any elimination diet should be done cautiously and ideally with guidance from a healthcare professional to avoid nutritional deficiencies.
8. Viral TikTok Eczema Hacks: Helpful or Harmful?
Social media is full of “quick fixes” for eczema and skin irritation, but not all of them are safe. Remedies like oatmeal baths or aloe vera can be soothing for some individuals, while others—such as applying acidic substances directly to the skin—may cause burns or worsen inflammation.
It’s important to approach viral trends with skepticism. What works for one person may seriously irritate another, especially if your skin barrier is already compromised.
9. Over-the-Counter Treatments: Temporary Relief
Drugstore creams and ointments can help manage symptoms in the short term. Mild hydrocortisone creams may reduce redness and itching, while thick emollients can ease dryness.
However, these treatments address symptoms rather than the root cause. Long-term or frequent use of steroid creams should be avoided without medical supervision, as they can thin the skin over time.
10. When It’s Not Eczema: Other Possible Conditions
If your symptoms don’t quite match eczema, other conditions may be responsible. Psoriasis often causes thick, scaly plaques with clear borders. Rosacea typically affects the face and includes persistent redness and visible blood vessels.
Contact dermatitis is another possibility, occurring when your skin reacts to something it touches—such as metals, skincare products, or fabrics. A proper diagnosis is essential for effective treatment.
11. What to Track Before Your Doctor’s Appointment
Documenting your symptoms can make your appointment far more productive. Keep notes on when flare-ups occur, how long they last, and what seems to trigger or relieve them. Include details about foods, stress levels, sleep quality, and skincare products.
Taking photos during flare-ups can provide valuable visual evidence, especially if symptoms improve before your appointment.
12. Gentle At-Home Routines to Get You Through the Month
While you wait to see your doctor, consistency is key. Moisturize regularly with thick, fragrance-free creams. Using a humidifier at night can help prevent dry air from worsening irritation, especially during colder seasons.
Choose loose, breathable clothing and avoid scratching as much as possible to prevent skin damage. Ingredients like chamomile, calendula, or colloidal oatmeal may offer calming effects. These simple routines won’t replace medical care, but they can significantly reduce discomfort and help protect your skin in the meantime.
News in the same category


Yellowed, burnt-on stainless steel pots will shine like new after soaking them in this water

4 types of hip pain that signal multiple cancers: Women need to be especially vigilant
To preserve tofu, don't put it directly in the refrigerator. Remember these two tips and your tofu will stay fresh for 10 days.

Don't throw away fruit netting; use it for these 12 things and save a considerable amount of money.

This liquid helps clean mold stains on walls and ceilings; it's easy to find but not many people know about it.
So good! Thanks nana!
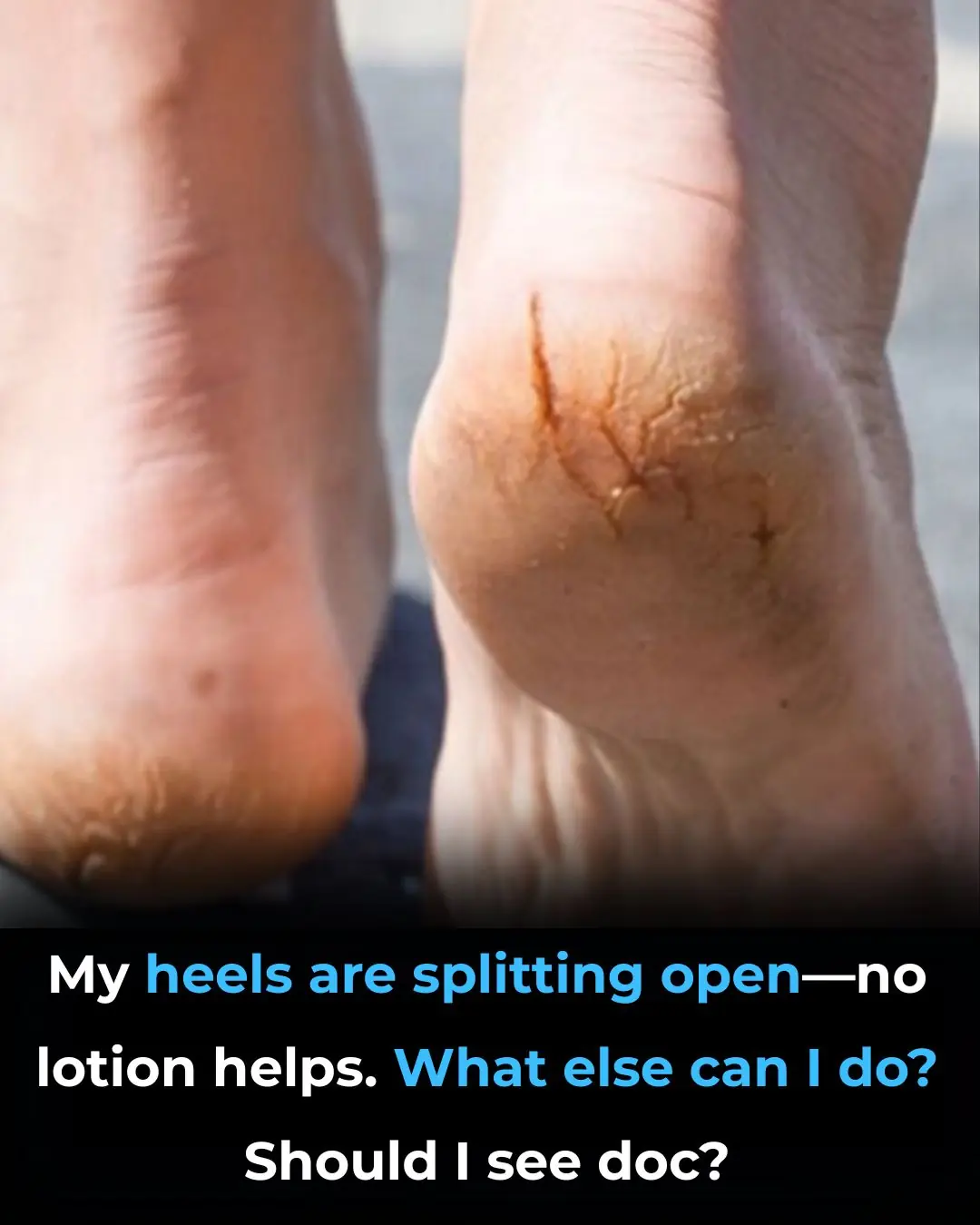
My heels are splitting open—no lotion helps. What else can I do? Should I see doc?
My aunt swears by this trick to reduce the look of thinning eyebrows that takes almost 0 work. Here's how it works

These purple veins appeared out of nowhere, and my doctor appointment is still weeks away. Should I worry?

Brown flat spots keep showing up on the back of my hands. Doctor appt is forever away. What should I do?

Mopping the floor with this ingredient will make it sparkling clean, like new, and dust-free for a whole week.
Is it safe to eat rice that has been left in a rice cooker overnight
When thawing pork, do not soak it in water.
My bathroom sink has been draining slower by the day, and plumbers are fully booked until after Christmas. What can I try first?

How to easily and neatly remove the black vein from the back of a shrimp?

What Happens To Your Blood Pressure When You Eat Bananas

How to preserve chili peppers for several months so they stay fresh, plump, and flavorful, without drying out.

Add some menthol oil to garlic: Hang it in a window or corner of the house for amazing benefits
News Post
Early Signs of Multiple Sclerosis

11 Benefits of Going Caffeine-Free

5 Early Signs of Cervical Cancer That Are Often Ignored: 90% of Women Overlook Them

The Cheap Drink That Can Help Prevent Stroke, Reduce Blood Fat, and Fight Cancer

Bone-chilling 2025 predictions from both Nostradamus and Baba Vanga

2 quick and easy ways to wash yellowed pillow inserts, making them sparkling white like new in no time

Yellowed, burnt-on stainless steel pots will shine like new after soaking them in this water

8 Signs You’re Eating Too Much Sugar

4 types of hip pain that signal multiple cancers: Women need to be especially vigilant

Accidental discovery of bone-eroding cancer after a fall: It turns out the body had been crying for help for a long time but was ignored
10 Eye Symptoms to Watch Out For

Does Eating Bananas Before Bed Have Any Benefits?
Can’t Fall Back Asleep After Waking Up to Use the Bathroom? Try These 5 Hacks

What Is Preventive Botox (or ‘Baby Botox’) — and Is It Safe?

I stayed silent when my husband called me his “youthful mistake” in front of everyone and laughed. But when he woke up in the apartment and saw the message on the mirror… He froze in shock!

I won $50 million in the lottery. I ran with our little son to my husband’s office to give him the news. When I arrived, I heard intimate sounds from him… So then, I did something.

After my husband’s funeral, my son drove me to a remote road and said: ‘This is where you get off. The house and business are mine now.’

AT 3 AM, I ASKED MY CHILDREN TO TAKE ME TO THE HOSPITAL. I COULD BARELY STAND. THEY YAWNED AND SAID: ‘MOM, CALL AN UBER. WE HAVE WORK TOMORROW.’
