Why Are Cancer Rates Among Young Women Skyrocketing? The Alarming Truth Revealed!
Cancer Incidence Rates Among Young Women Surge, While Mortality Continues to Decline: A Detailed Look at the Rising Crisis
Cancer incidence rates continue to rise across many common types of cancers, and the most concerning rise is observed among women. From 2002 to 2021, the cancer incidence rate for women under the age of 50 surged dramatically, rising from 51% higher than men in 2002 to an alarming 82% higher in 2021. This development is especially troubling as it reflects broader trends in cancer prevalence that are having a disproportionate impact on younger women.
While the overall cancer incidence continues to climb, there is a positive trend in cancer mortality rates, which have been declining steadily. Over the last three decades, the cancer mortality rate in the United States has dropped by 34%. This has been attributed to major advancements in cancer treatment, smoking cessation, and the widespread implementation of early detection techniques. As a result, approximately 4.5 million lives have been spared from cancer-related deaths since the peak of the mortality rate. Most of these gains are linked to steady declines in the mortality rates of the four most common cancer types: breast cancer, colorectal cancer, lung cancer, and prostate cancer. Despite this progress, cancer remains the second leading cause of death in the United States and the leading cause of death for people under 85 years old.
In addition to rising cancer incidence and mortality rates, alarming racial disparities in cancer outcomes persist. According to recent data, American Indian and Alaska Native (AIAN) populations are 2 to 3 times more likely to die from cancers such as cervical, kidney, liver, and stomach cancers when compared to their White counterparts. Black individuals are also at a higher risk, with a twofold increase in the likelihood of dying from prostate, stomach, and uterine cancers compared to White people. These disparities highlight the urgent need to address systemic inequities in healthcare and cancer care.
These findings are based on the "Cancer Statistics, 2025" report, published by the American Cancer Society (ACS) in its flagship journal CA: A Cancer Journal for Clinicians. The report, along with its companion report, Cancer Facts & Figures 2025, serves as a trusted resource for global cancer statistics. It includes contributions from prominent ACS researchers including Rebecca Siegel, MPH, Tyler B. Kratzer, MPH, Angela Giaquinto, MSPH, Hyuna Sung, PhD, and Ahmedin Jemal, DVM, PhD.
Rising Cancer Burden for Women Under 65
In recent years, the cancer burden has notably increased among women under the age of 65. The risk of developing cancer varies significantly by age and sex, with middle-aged women now having a slightly higher risk of developing cancer than their male counterparts. Notably, women under 50 are almost twice as likely to develop cancer compared to young men, and this gap has been widening since the early 2000s. For individuals aged 50 to 64, men have historically had a higher likelihood of being diagnosed with cancer than women in the same age group.
The largest recorded difference in cancer incidence between men and women occurred in 2007, with a 21% gap. However, from 2011 onward, the cancer incidence rate for women began to increase gradually, eventually equaling that of men in 2021. A particularly striking milestone occurred in 2021 when lung cancer among women surpassed that of men for the first time for adults under the age of 65, marking a new chapter in the ongoing shift of cancer trends.
For women under the age of 50, the higher cancer incidence rate has largely been attributed to breast cancer, which continues to be a major factor. Between 1998 and 2021, the incidence rates for men under 50 remained relatively stable, whereas the rates for women increased, further widening the gap in cancer risk between males and females. By 2021, the cancer incidence rate for women had become 82% higher than that for men, largely driven by increasing rates of breast cancer and thyroid cancer in women, although the latter has shown a slight decline in recent years.
Persistent Disparities in Cancer Incidence and Mortality Across Racial Groups
Disparities in both cancer incidence and death rates among racial groups continue to persist. While cancer mortality rates often provide a clearer picture of progress in cancer treatment and care, they are also significantly influenced by various factors such as healthcare access, early detection practices, and advancements in treatment.
Racial and ethnic disparities are largely driven by historical and ongoing discrimination, which limits economic mobility and access to quality healthcare for many racial minorities. These disparities are compounded by socio-economic factors, with poverty ranking among the leading causes of death alongside smoking-related illnesses. In 2022, a significant portion of people living below the federal poverty level (defined as $27,750 for a family of four) were from minority groups: 25% of American Indian/Alaskan Native (AIAN) people, 17% of Black and Hispanic people, and 9% of White and Asian people.
The overall cancer incidence and mortality rates for different racial and ethnic groups vary widely. AIAN populations have the highest combined cancer incidence and mortality rates, both for men and women, followed by Black men, who face the highest cancer mortality rates among all racial groups. Black women also experience the highest mortality rate for breast cancer, and for uterine cancer, Black women are 2 to 3 times more likely to die than any other racial group. Furthermore, AIAN women face the highest mortality rates for cervical cancer, while colorectal cancer and lung cancer mortality are also disproportionately higher in AIAN populations.
Efforts to reduce these disparities are ongoing, with increased investments aimed at expanding access to high-quality cancer care in underserved communities, particularly those in AIAN and Black populations. These efforts could significantly accelerate progress in cancer treatment and outcomes.
Advances in Survival Rates and Treatment
In recent decades, the five-year relative survival rate for most cancers has improved significantly, with the most notable improvements in cancers of the thyroid, prostate, testis, and melanoma. The five-year survival rate for these cancers is as high as 98% for thyroid cancer, 97% for prostate cancer, 95% for testicular cancer, and 94% for melanoma. These improvements are largely attributed to earlier detection through cancer screening and incidental detection via imaging for cancers of the breast, prostate, thyroid, and kidney.
However, despite these advances, certain cancers remain difficult to treat, and their survival rates remain low. Pancreatic cancer, for example, has seen a sharp increase in its death rate, largely due to increased incidence linked to rising obesity rates in the U.S., a known risk factor for pancreatic cancer. The survival rate for pancreatic cancer remains dismal, with only a 5-year relative survival rate of about 8%.
Similarly, uterine (endometrial) cancer, which is the fifth most common cause of cancer death among women, has seen little progress in treatment over the past several decades. The survival rate for uterine cancer has actually declined in recent years, and there are no standard screening tests for early detection, despite the fact that many cases are diagnosed at an early stage.
Conclusion and Future Outlook
Despite the progress made in cancer treatment and mortality reduction, the growing cancer incidence rate among younger women is a troubling trend that requires urgent attention. Early detection, continued investment in cancer research, and addressing disparities in healthcare access are critical to combating these challenges. As researchers continue to develop more effective treatments, the hope is that future advances in cancer therapy will continue to improve survival rates and reduce disparities in outcomes based on race and socio-economic status.
This data was collected and analyzed by the American Cancer Society (ACS) using information from cancer registries and national health statistics. As research continues, especially in the wake of the COVID-19 pandemic, scientists expect to uncover further impacts of delayed diagnoses and treatment. However, it will take time to fully assess how these factors have influenced cancer outcomes.
Sources:
News in the same category


Urgent Warning: 21 Poisonings Linked to Deadly Death Cap Mushrooms in California – Here's What You Need to Know!
62,000 African Penguins Have Died From Starvation in South Africa: A Call for Urgent Conservation Action

Why Your Calf Muscles Are Your 'Second Heart' and How to Keep Them Strong for Better Circulation!

Norway Launches the Aurora Train: A Unique Night Journey to Witness the Northern Lights
What Yellow Stuff In Your Eyes When You Wake Up Actually Is
Exploring the Abyss: The Mesmerizing Depths of the Ocean Beyond 200 Meters
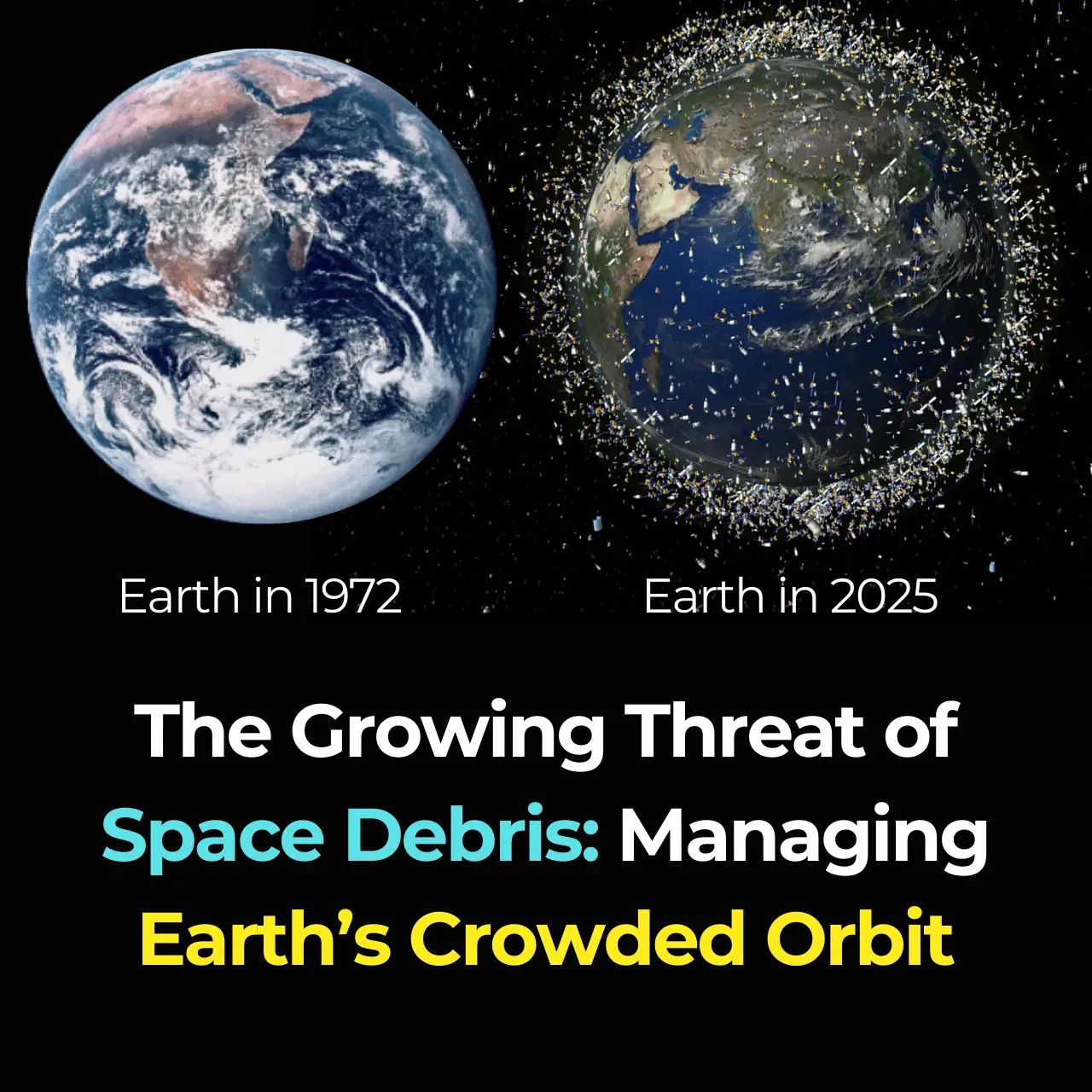
The Growing Threat of Space Debris: Managing Earth’s Crowded Orbit

What Your Favorite Ice Cream Flavor Says About You
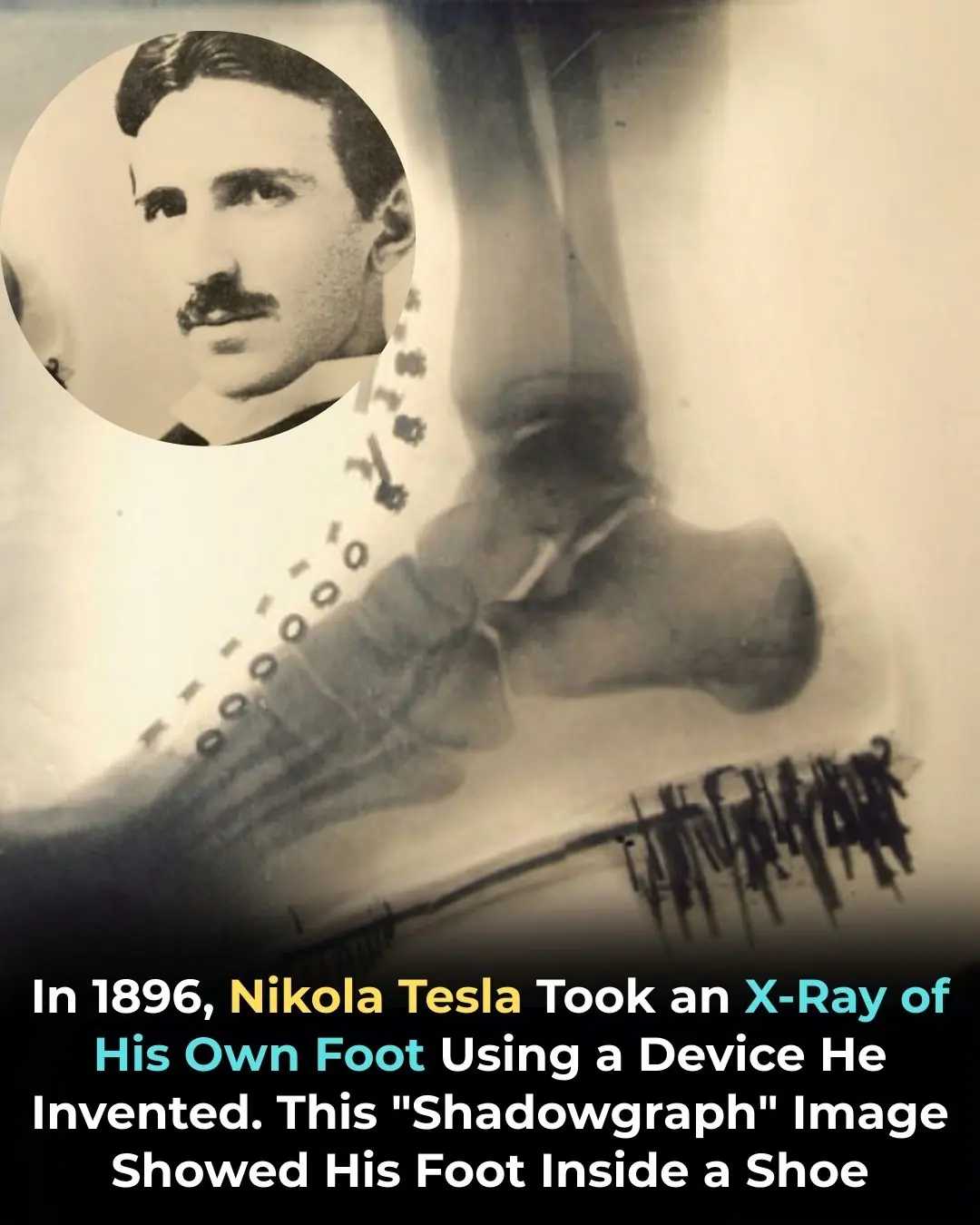
Nikola Tesla X-Rayed His Own Foot in 1896 — Pioneering the Future of Medical Imaging
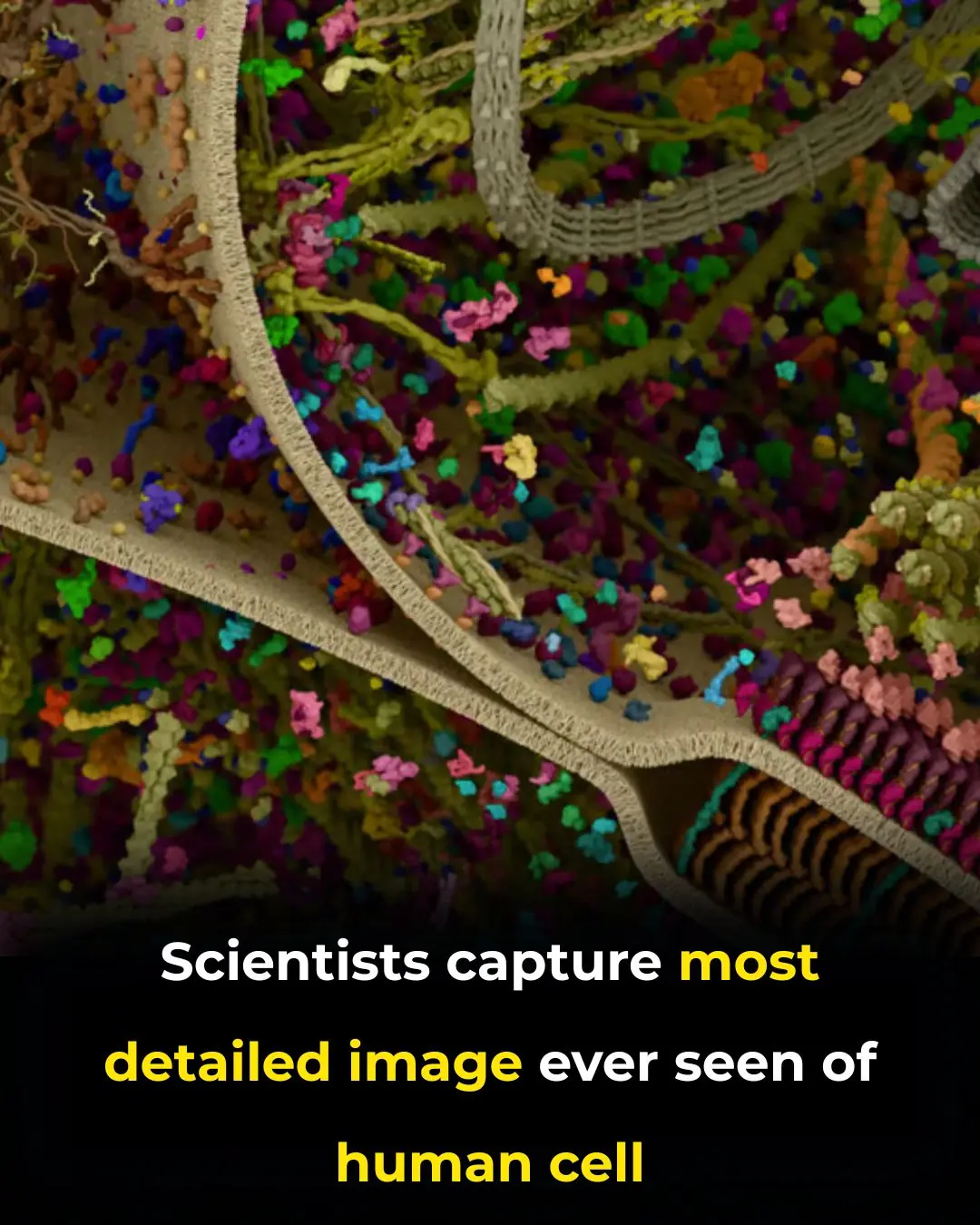
Revolutionary Breakthrough: Scientists Capture the Most Detailed 3D Image of a Human Cell
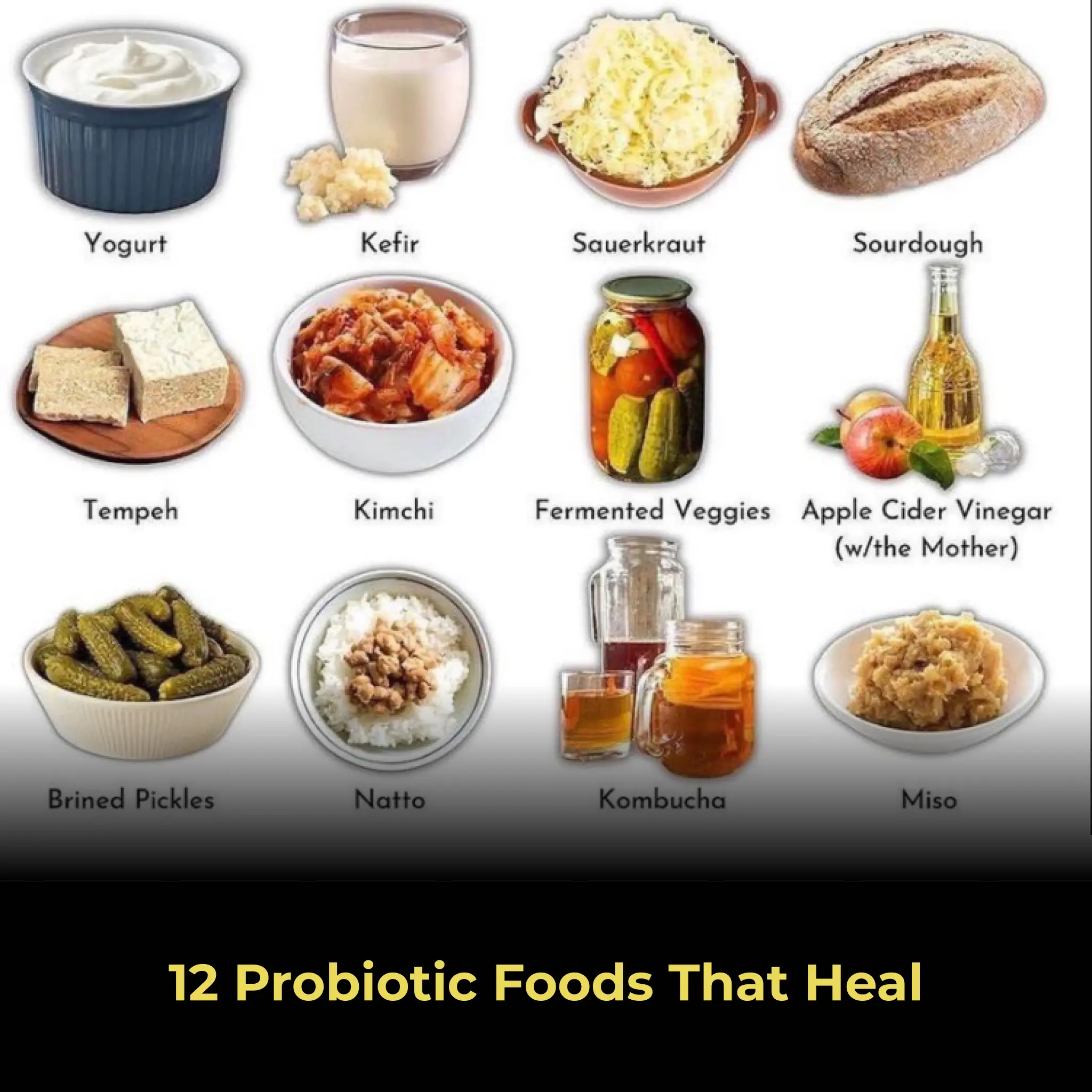
12 Probiotic Foods That Heal

Connecting Consumers to Farmers: The Trend of Personalized Food Packaging in Japan
Experience the Journey of a Lifetime: Ride Across America for Just $213 with Amtrak

12 Common Household Items That Are Slowly Killing Us

Magpie The Spiritual Meaning of an Unusual Encounter
Humanity’s Farthest Traveler Still Hasn’t Reached One Light-Year
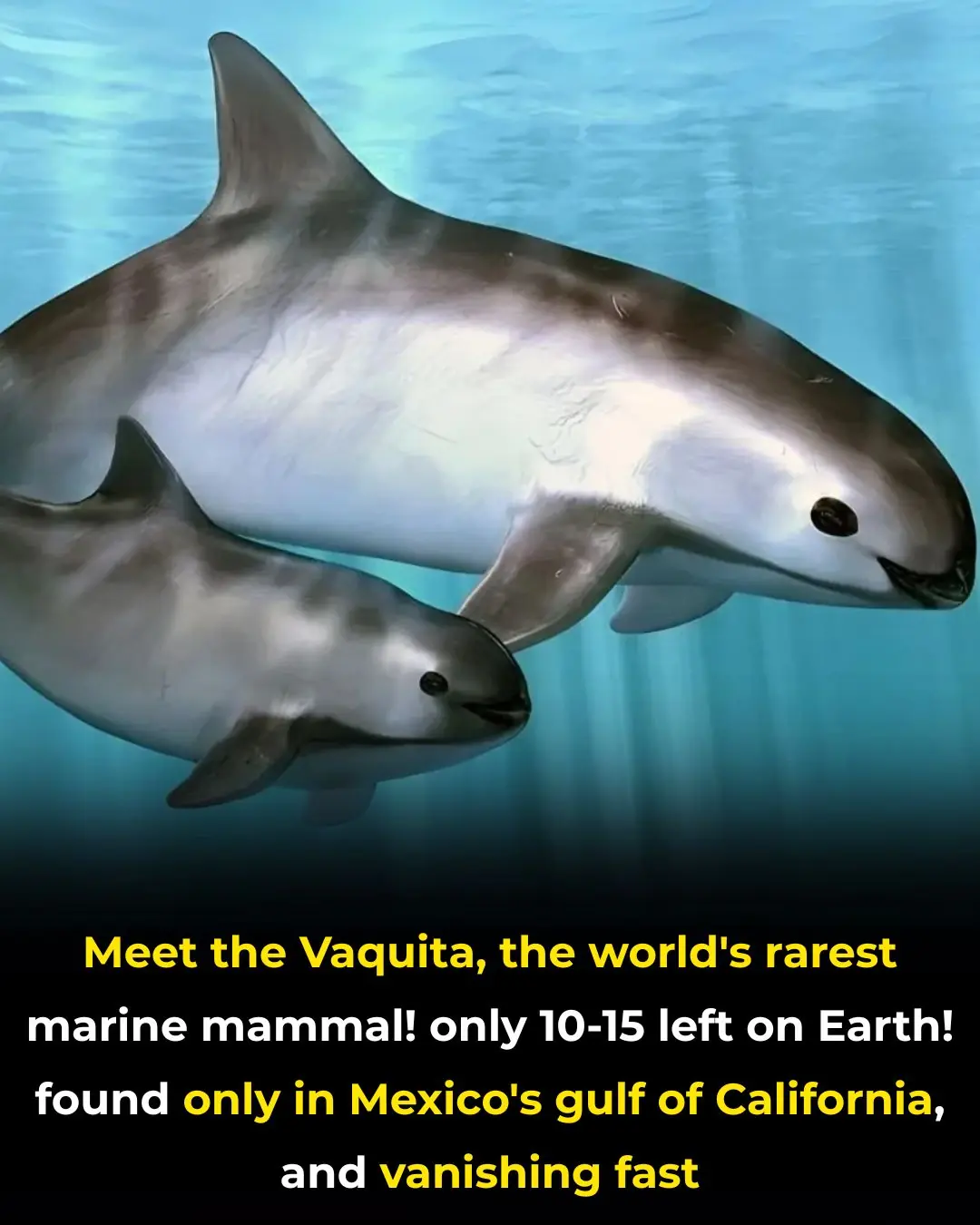
The Vaquita: Earth's Most Endangered Marine Mammal Fights for Survival

AI Drones Are Rebuilding Australia’s Forests, One Seed Pod at a Time
News Post

Top 13 Vitamins for High Blood Pressure – Reduce Naturally!

70-year-olds look 40! 🍀 The Japanese wrinkle remedy you need to try

Revolutionary Stem Cell Injection Restores Natural Hearing: A Breakthrough That Could Change the Future of Medicine

Urgent Warning: 21 Poisonings Linked to Deadly Death Cap Mushrooms in California – Here's What You Need to Know!
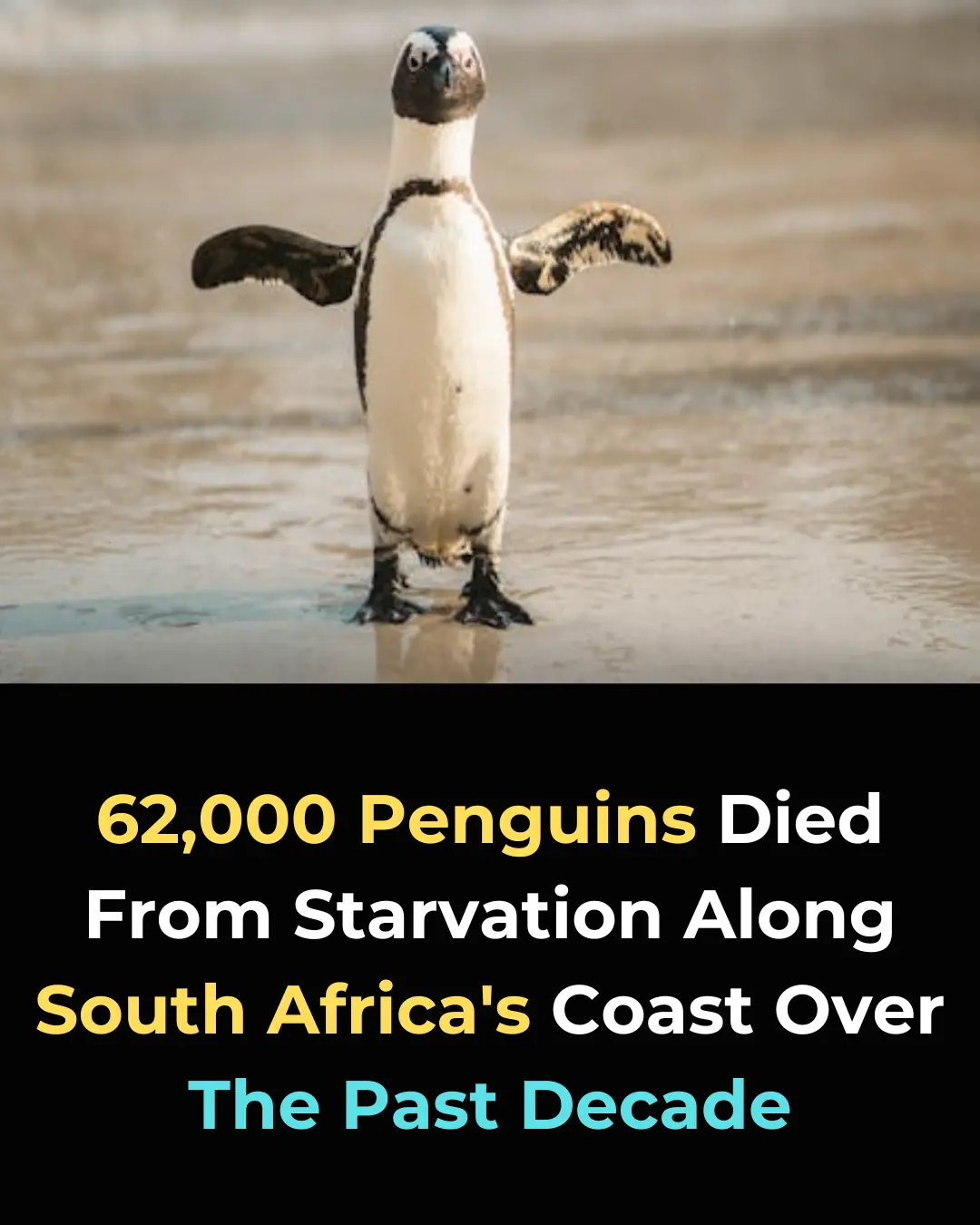
62,000 African Penguins Have Died From Starvation in South Africa: A Call for Urgent Conservation Action

Why Your Calf Muscles Are Your 'Second Heart' and How to Keep Them Strong for Better Circulation!

Norway Launches the Aurora Train: A Unique Night Journey to Witness the Northern Lights

Shocking: Savannah Miller, 24, Forgot Her Tampon Inside Her for a Month

What Makes a Man Leaves His Wife For Another Woman

10 Clever Dryer Sheet Hacks That Will Transform Your Home
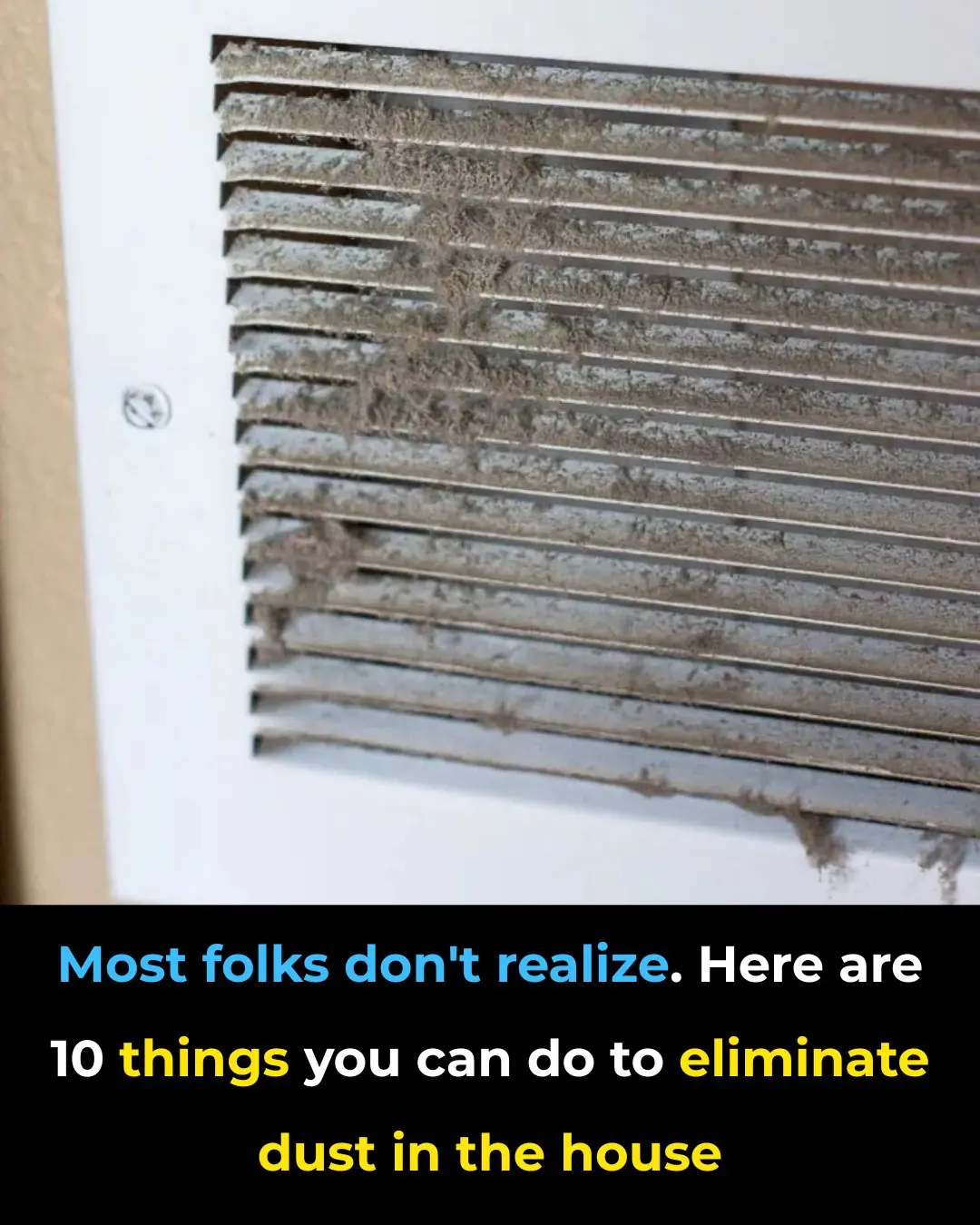
10 Smart Ways to Reduce Household Dust — Most People Don’t Realize These Work So Well

11 Best Smelling Houseplants to Make Your Home Smell Amazing
I had no clue about this — until I learned the right way to store cooked rice

My Nana taught me this hack to remove oven grease in 4 minutes with zero scrubbing — here’s how it works

Lady dumps baking soda down her sink. Here’s the genius reason why

Struggling with stubborn toilet water rings? Here’s how to get rid of them for good

Say Goodbye to Bare Branches: Easy Hacks to Bring Your Christmas Cactus Back to Blooming
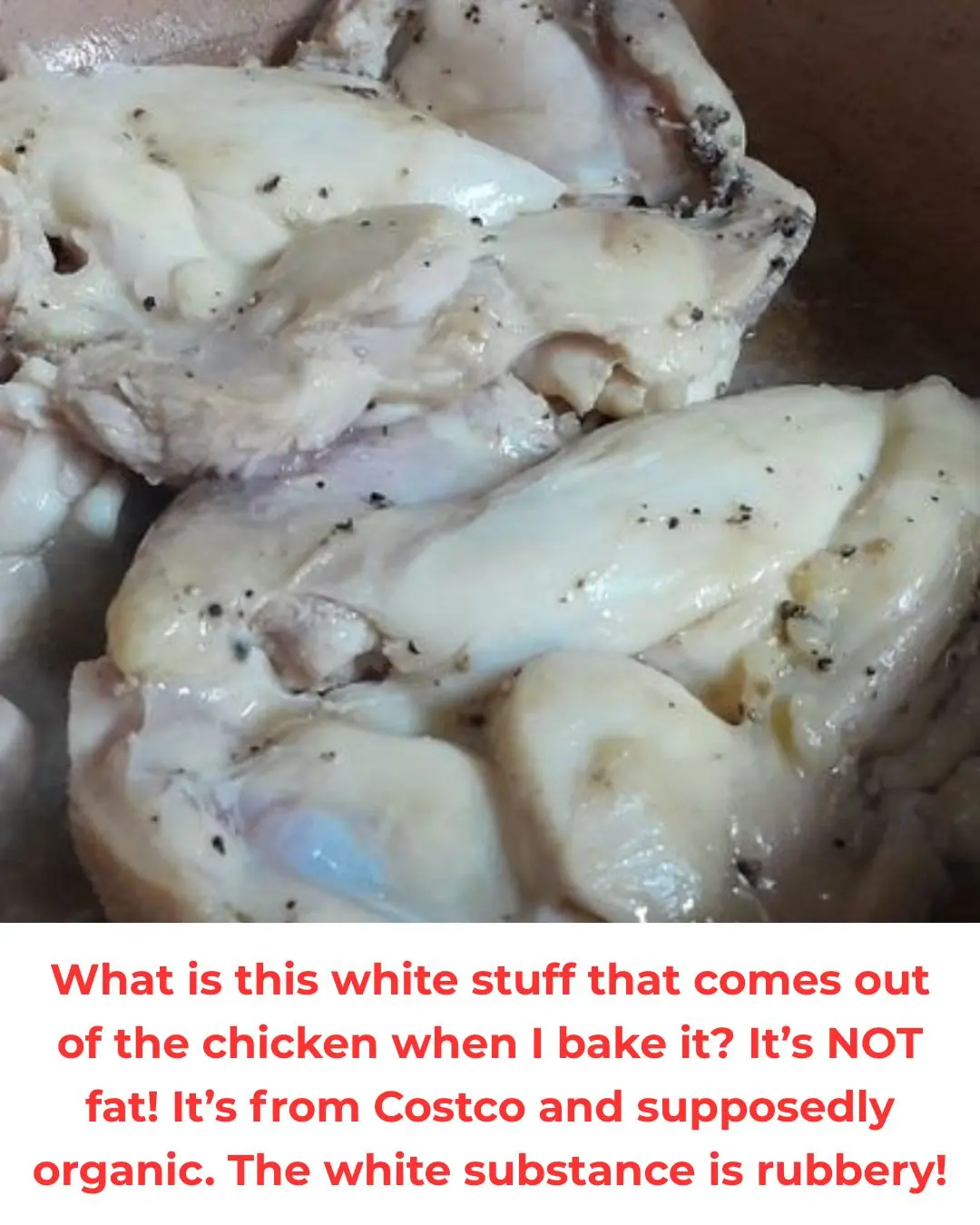
Why Your Cooked Chicken Might Have a White, Gooey Substance