
Winter Vomiting Disease On Uptick In Midwest
Highly Contagious Stomach Bug Doubles in Midwest Ahead of Holiday Season
As the holiday season approaches and families prepare for year-end celebrations, an unwelcome guest has already arrived—earlier than expected. Across the Midwest and Northeast of the United States, a highly contagious pathogen is making the rounds. Wastewater systems, often an overlooked source of health data, are telling a story that clinical data alone cannot fully capture. And what they reveal demands urgent attention.
Medical facilities across Indiana, Michigan, and Louisiana have reported an uptick in norovirus cases, a viral infection commonly known as winter vomiting disease. Infectious disease specialists are concerned, as this pathogen has been moving through communities far earlier than expected, much earlier than the usual winter surge. Wastewater monitoring programs are capturing alarming patterns of accelerating transmission, and contamination levels have risen to heights not seen in years.
A Shift in Norovirus Behavior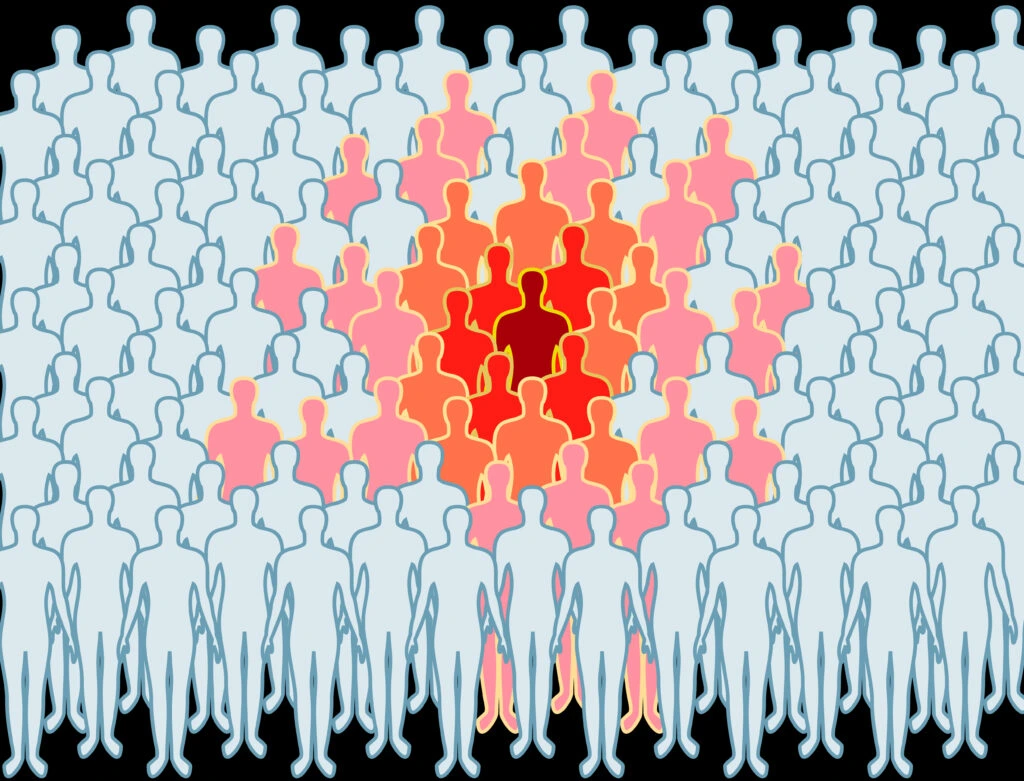
Norovirus, a leading cause of gastroenteritis in the United States, has undergone a notable shift this year. A new variant, GII.17, has become the dominant strain, responsible for three-quarters of all norovirus outbreaks in 2025. This marks a significant change from 2023 when GII.17 accounted for less than 10% of cases. For over thirty years, a different strain, GII.4, had been the primary culprit. The rise of GII.17 signals a dramatic shift in the behavior of this pathogen, and it could pose new challenges for public health.
Dr. Robert Atmar, a professor in the Department of Medicine at Baylor College of Medicine, explained the shift: “The two possibilities are that something in the virus changed to make it more transmissible, or there were changes in the population making a larger proportion susceptible,” he noted. “And probably it’s a combination of both.”
The GII.17 variant has been gaining ground in countries worldwide, and while scientists continue to debate whether it carries enhanced transmissibility or if it is exploiting a population that lacks immunity, it’s clear that communities are now facing a pathogen that many immune systems have never encountered before. The surge began in mid-October, weeks ahead of the typical winter outbreak, catching many experts off guard.
Wastewater Data Reveals Regional Hotspots
WastewaterSCAN, a partnership between Stanford University and Emory University, has been monitoring disease spread through municipal wastewater systems. Data collected through late November shows that norovirus wastewater concentrations have risen 69% nationwide since October. Amanda Bidwell, the scientific program manager for the project, confirmed that the contamination levels are now categorized as high at the national level.
Indiana, Michigan, and Louisiana are currently leading in terms of contamination readings. Connecticut and Massachusetts have similarly high levels of contamination. The advantage of wastewater surveillance is its ability to provide a snapshot of infection rates in the community, regardless of whether individuals seek medical care or get tested.
Although the levels still remain below the peak recorded last year, when outbreaks surged to their highest levels in a decade, the trajectory is concerning. Rates of norovirus cases continue to rise, and experts worry that the season has just begun. Wastewater surveillance has proved to be an invaluable early warning tool, capturing cases that would otherwise go undetected.
Cases Double Within Weeks
Testing positivity rates tell an even more compelling story. During the week of November 15, approximately 14% of norovirus tests came back positive, a striking increase from the 7% positivity rate recorded just three months earlier. By early December, at least 91 outbreaks had been reported, more than double the number typically seen during the same period in previous years. As December progresses, health experts are bracing for an even larger spike in cases.
Despite a decline in the number of outbreaks reported between August and November 2025 compared to the same period in 2024, the overall trajectory is worrying. Between August 1 and November 13, the CDC’s NoroSTAT program reported 153 outbreaks, down from 235 outbreaks last year. However, these numbers are still climbing, and the season’s true impact has yet to be fully realized.
Norovirus Symptoms Hit Fast and Hard
Norovirus infection strikes quickly, typically within 12 to 48 hours after exposure. Infected individuals often experience violent bouts of vomiting and diarrhea, earning the pathogen its nickname “two-bucket disease.” Nausea, stomach pain, and body aches are common symptoms. Dr. Donald Dumford, an infectious disease physician at the Cleveland Clinic, describes the clinical presentation as causing “a combination of vomiting and diarrhea, and although most cases resolve within one to three days, the misery during that period is considerable.”
Dehydration is a significant risk, particularly for vulnerable populations such as the elderly and young children. Rapid fluid loss can lead to serious complications if not managed properly. Symptoms of dehydration include dizziness, dark urine, and unusual tiredness. For children, signs of dehydration include dry mouth, reduced tears when crying, and increased fussiness or sleepiness.
The Persistent Threat of Norovirus
Each year, norovirus causes approximately 19 to 21 million illnesses in the United States, making it the leading cause of gastroenteritis. It accounts for over half of all foodborne illnesses in the country. Hospitals report about 109,000 admissions annually due to complications related to norovirus, and around 900 deaths are attributed to the infection each year.
While most healthy adults recover fully, the very young, elderly, and immunocompromised are at greater risk of severe illness and complications. Norovirus is a human-only pathogen, meaning it cannot infect animals or spread through animal contact. The virus spreads primarily through person-to-person transmission, with outbreaks commonly occurring in settings such as schools, nursing homes, and households.
Norovirus: The Perfect Pathogen
Norovirus has earned the nickname “the perfect pathogen” due to its remarkable resilience. It can survive on surfaces for weeks or even months, and alcohol-based hand sanitizers are ineffective at eliminating it. The virus has a tough protein shell, called a capsid, that resists alcohol’s action. Additionally, norovirus can survive temperatures as high as 145°F, making it exceptionally difficult to kill through standard cooking methods.
The virus’s resilience also means that it requires minimal exposure to cause infection. As few as one to ten viral particles are enough to establish an infection, and an infected person can shed billions of viral particles through their stool and vomit. A single contaminated surface or food item can spread the virus to dozens of individuals.
Multiple Transmission Routes Increase Spread
Norovirus spreads through multiple pathways, including direct contact with infected individuals, touching contaminated surfaces, and consuming contaminated food or water. Vomiting also releases aerosolized viral particles that can be inhaled or settle on surfaces, further contributing to its spread. Shellfish, particularly oysters and clams, can accumulate norovirus from contaminated water, posing a significant risk when consumed raw or undercooked.
Prevention and Control Measures
Hand sanitizers are ineffective against norovirus, so washing hands with soap and water remains the most effective means of preventing infection. Hands should be washed thoroughly for at least 20 seconds before preparing food, after using the restroom, or after handling diapers. Proper food handling and preparation, including cooking shellfish to the correct temperature, is crucial to preventing outbreaks.
No antiviral treatment exists for norovirus, so management focuses on symptom relief and hydration. Oral rehydration solutions such as Pedialyte can help replace lost fluids, and in severe cases, intravenous fluids may be necessary. While there is no vaccine currently available, Moderna is conducting a Phase 3 clinical trial for a potential mRNA-based vaccine.
Stay Home and Protect Others
Isolation remains a key prevention measure. Individuals infected with norovirus should remain home for at least 48 hours after symptoms resolve to prevent spreading the virus to others. Those who feel unwell should avoid preparing food for others during this time.
With wastewater contamination levels continuing to rise and holiday gatherings approaching, awareness is crucial. Norovirus may not capture the same attention as other viral threats, but its toll is significant, particularly as the winter season begins earlier than usual this year.
Sources:
-
Centers for Disease Control and Prevention (CDC). "Norovirus and Gastroenteritis." CDC Website, 2024.
-
Stanford University. "Wastewater Monitoring and Disease Surveillance." Stanford News, 2024.
-
Dumford, D., et al. "Norovirus Infections: The Impact on Public Health." Cleveland Clinic Journal of Medicine, 2024.
News in the same category

Chronic Gastritis: Causes, Symptoms, and Treatment Options
Lung Cancer: 8 Common Symptoms Often Misdiagnosed
Type 2 Diabetes: Early Symptoms and Effective Ways to Control It
A Potentially Fatal New Covid-related Syndrome Has Emerged

The FIRST Sign of VITAMIN B12 DEFICIENCY Is…

Your Body Is Lacking Magnesium If…
Two handfuls of peanuts daily boost memory in 4 months
Fatty Liver Disease: What Doctors Want You to Know Early
Silent Kidney Disease: Symptoms, Causes, and Prevention Tips
10 Warning Signs of Heart Disease Most People Ignore

Doctors reveal that eating beets causes...
People with heart problems should avoid these 4 things to reduce stimulation to the heart
12 Bizarre Symptoms of Vitamin D Deficiency You Need to Know

Natural Remedies and Prevention Strategies for Bunions: What Really Works

Natural Scar Remedies: How Scars Form and the Most Effective Evidence-Based Treatments to Help Them Fade
Eight Digestive Red Flags You Should Never Ignore: Causes, Risks, and When to Seek Medical Care

A Complete Guide to Bulging Veins: Causes, Complications, and Care

The Myth of “Safe” Smoking Debunked: How Minimal Tobacco Use Still Damages the Body
News Post

His whole body was itchy, he thought it was an allergy but then he was diagnosed
Chronic Gastritis: Causes, Symptoms, and Treatment Options
Lung Cancer: 8 Common Symptoms Often Misdiagnosed
Type 2 Diabetes: Early Symptoms and Effective Ways to Control It
A Potentially Fatal New Covid-related Syndrome Has Emerged
Stroke in Young Adults: Why It’s Becoming More Common

The FIRST Sign of VITAMIN B12 DEFICIENCY Is…

Your Body Is Lacking Magnesium If…
Two handfuls of peanuts daily boost memory in 4 months
Fatty Liver Disease: What Doctors Want You to Know Early
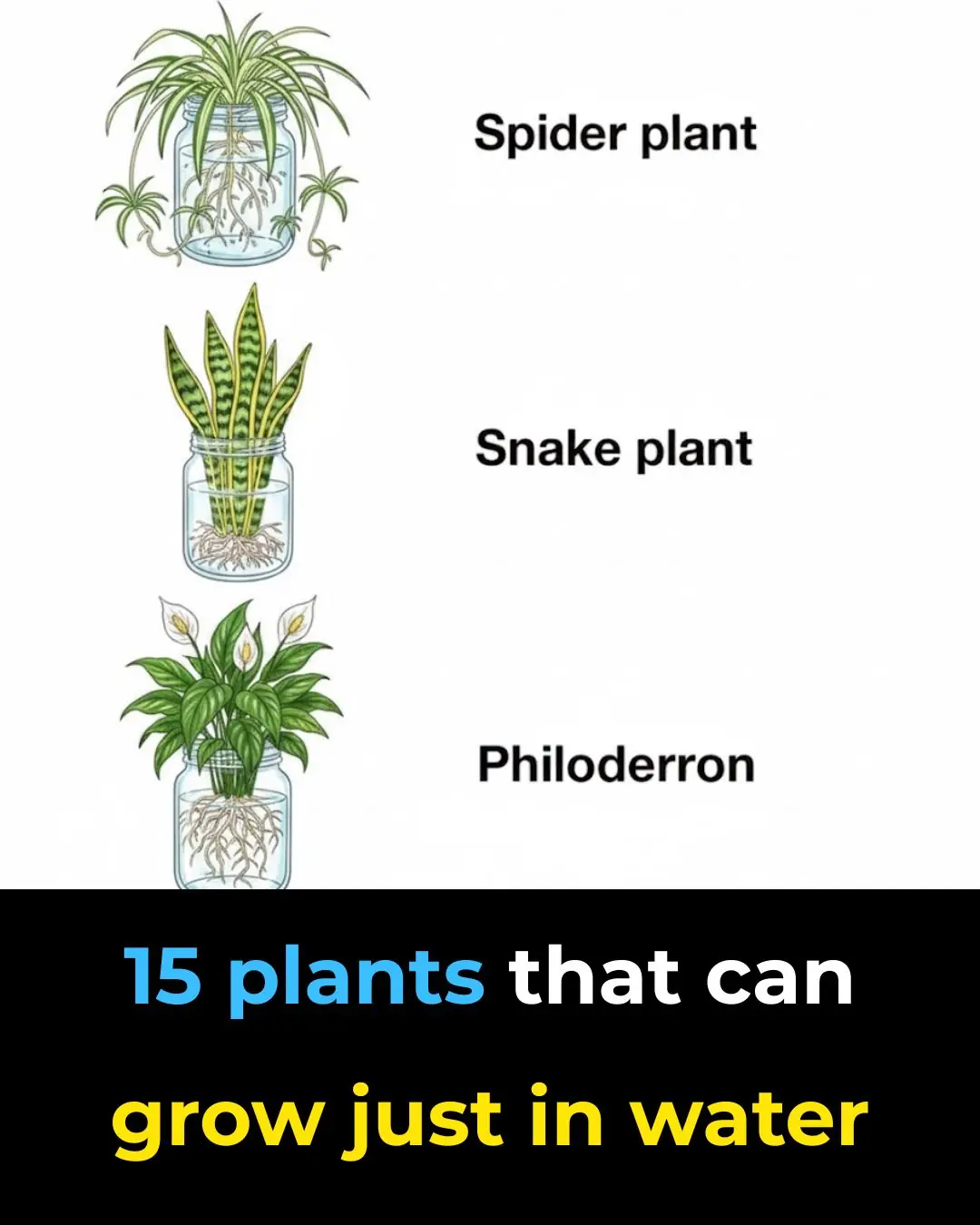
15 Plants That Can Grow Easily in Water — A Beautiful, Soil-Free Way to Green Your Home

Most people get this wrong and toss out the can. Here’s the right way to read ‘Best By’ or ‘Best Before’ dates
I Had No Idea! The Remarkable Story of the Stone Breaker Plant

Stop throwing out old hoses — 10 brilliant hacks to use them around the house

This Method Is So Brilliant — I Wish I’d Thought of It Sooner!
Silent Kidney Disease: Symptoms, Causes, and Prevention Tips

When boiling duck, don't add ginger and cold water: Add this and the meat will lose all its stench, and you won't get tired of eating it.

How to make steamed chicken with lemongrass, golden brown chicken, soft and delicious, irresistible
