
Are You Up to Date on Migraine Prevention?
New First-Line Recommendations and Practical Strategies for Clinical Practice
Migraine is one of the most common and disabling neurological disorders worldwide, affecting more than one billion people and ranking among the leading causes of years lived with disability. Despite its prevalence, migraine remains underdiagnosed and undertreated, particularly when it comes to preventive therapy. Recent advances in migraine science have transformed prevention strategies, prompting updated clinical recommendations that emphasize earlier, more effective intervention.
This continuing medical education (CME) update highlights new first-line preventive options and provides practical guidance for managing patients with frequent or disabling migraine.
When to Consider Preventive Migraine Therapy
Preventive treatment is recommended for patients who experience frequent migraine attacks or significant migraine-related disability. Current guidance suggests initiating prevention in patients who have:
-
Four or more migraine days per month
-
Two or more migraine days per month with substantial disability
-
Poor response, intolerance, or contraindications to acute treatments
-
Risk of medication-overuse headache
-
Patient preference for reducing attack frequency and severity
The goal of preventive therapy is not complete elimination of migraine, but a meaningful reduction in attack frequency, intensity, duration, and reliance on acute medications.
Evolving Understanding of Migraine Pathophysiology
Advances in migraine research have clarified the role of calcitonin gene-related peptide (CGRP), central sensitization, and altered pain processing in migraine. This improved understanding has driven the development of targeted therapies that address migraine mechanisms more specifically than traditional preventives.
As a result, prevention is no longer limited to repurposed medications originally developed for hypertension, depression, or epilepsy.
New First-Line Preventive Treatment Options
CGRP-Targeted Therapies
CGRP monoclonal antibodies are now recognized as first-line options for migraine prevention in many patients. These therapies include both injectable and oral agents designed specifically for migraine prevention.
Key advantages include:
-
Migraine-specific mechanism of action
-
Rapid onset of benefit
-
Favorable tolerability profile
-
Minimal drug–drug interactions
CGRP inhibitors are particularly beneficial for patients who have failed or cannot tolerate traditional preventive medications.
Traditional Preventive Medications Still Matter
Established preventive agents remain appropriate first-line options for many patients, particularly when cost, comorbidities, or access to newer therapies are considerations. These include:
-
Beta-blockers (e.g., propranolol, metoprolol)
-
Antiseizure medications (e.g., topiramate, valproate)
-
Antidepressants (e.g., amitriptyline, venlafaxine)
Selection should be individualized based on patient characteristics, comorbid conditions, and side-effect profiles.
OnabotulinumtoxinA for Chronic Migraine
For patients with chronic migraine (15 or more headache days per month), onabotulinumtoxinA remains an evidence-based preventive option. It is particularly useful in patients with medication overuse or those who have failed multiple oral preventives.
Practical Guidance for Clinicians
Start Low, Go Slow — but Don’t Wait Too Long
Titration remains important, especially with oral preventives. However, experts emphasize avoiding prolonged trials at subtherapeutic doses. A fair trial typically lasts 8–12 weeks at a therapeutic dose before assessing effectiveness.
Set Realistic Expectations
Patients should understand that:
-
Improvement may be gradual
-
A 50% reduction in migraine days is considered a successful response
-
Preventive therapy works best when combined with lifestyle optimization
Clear communication improves adherence and satisfaction.
Address Comorbidities and Triggers
Effective migraine management requires a holistic approach. Clinicians should screen for and address:
-
Sleep disorders
-
Anxiety and depression
-
Hormonal influences
-
Stress and lifestyle factors
Nonpharmacologic strategies such as regular sleep, hydration, exercise, and stress management remain foundational.
Reducing Medication-Overuse Headache
Frequent use of acute migraine medications can worsen headache frequency and reduce preventive effectiveness. Preventive therapy plays a critical role in breaking this cycle by decreasing reliance on rescue medications.
Early initiation of prevention can help prevent progression from episodic to chronic migraine.
Individualizing Treatment Decisions
There is no single “best” preventive therapy for all patients. Updated recommendations emphasize shared decision-making that considers:
-
Migraine frequency and severity
-
Prior treatment response
-
Comorbid medical conditions
-
Patient preferences and lifestyle
-
Insurance coverage and cost
This personalized approach improves long-term outcomes and adherence.
The Future of Migraine Prevention
The migraine prevention landscape continues to evolve, with ongoing research into new molecular targets, combination strategies, and biomarkers that may help predict treatment response. As understanding deepens, prevention is shifting from a trial-and-error process to a more targeted, patient-centered model.
Conclusion
Migraine prevention has entered a new era. Updated first-line recommendations now include migraine-specific therapies alongside traditional options, allowing clinicians to intervene earlier and more effectively. By recognizing candidates for prevention, selecting appropriate therapies, and partnering with patients, clinicians can significantly reduce migraine burden and improve quality of life.
Staying current with evolving migraine guidelines is essential—not only to reduce headache frequency, but to restore function, productivity, and well-being for patients living with this disabling neurological disease.
News in the same category


Can Metformin Protect Premature Infants After Antenatal Steroid Exposure?

Vaccines and Healthy Aging: Benefits That Go Beyond Infection Prevention

Drink Coconut Water for 7 Consecutive Days and Notice Remarkable Health Benefits

11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?

Surprise Finding: How the Immune System May Prevent Us From Burning Fat
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

The Best Time to Drink Pomegranate Juice for Blood Pressure and Muscle Recovery
Why Your Cat Chooses to Sleep With You

10 Conditions Ginger Can Help Manage Naturally

How Often Do You Poop? New Research Shows Bowel Movement Frequency Linked to Overall Health

What Happens to Your Blood Pressure When You Drink Beetroot Juice Every Day

Signs and Symptoms of Oral Cancer

Obesity Is a Disease: Understanding Its Biology and Cardiovascular Impact

Exercise Linked to Better Outcomes in Patients With Hypertension

Adding Yoga to Opioid Use Disorder Care May Speed Recovery From Opioid Withdrawal
News Post

Radiation and Targeted Cancer Therapy Combination Shows Low Risk of Serious Side Effects

Can Metformin Protect Premature Infants After Antenatal Steroid Exposure?

Choosing Compassion Over Cameras: A Young Man Saves a Shark by Removing a Fishhook

Abandoned at One Year Old: The Heartbreaking Reality Behind a Chihuahua Left at a Shelter

Pets Are Not Disposable: A Lifelong Commitment, Not a Temporary Choice

The 400-Year-Old Greenland Shark: One of the Oldest Living Vertebrates on Earth

Vaccines and Healthy Aging: Benefits That Go Beyond Infection Prevention
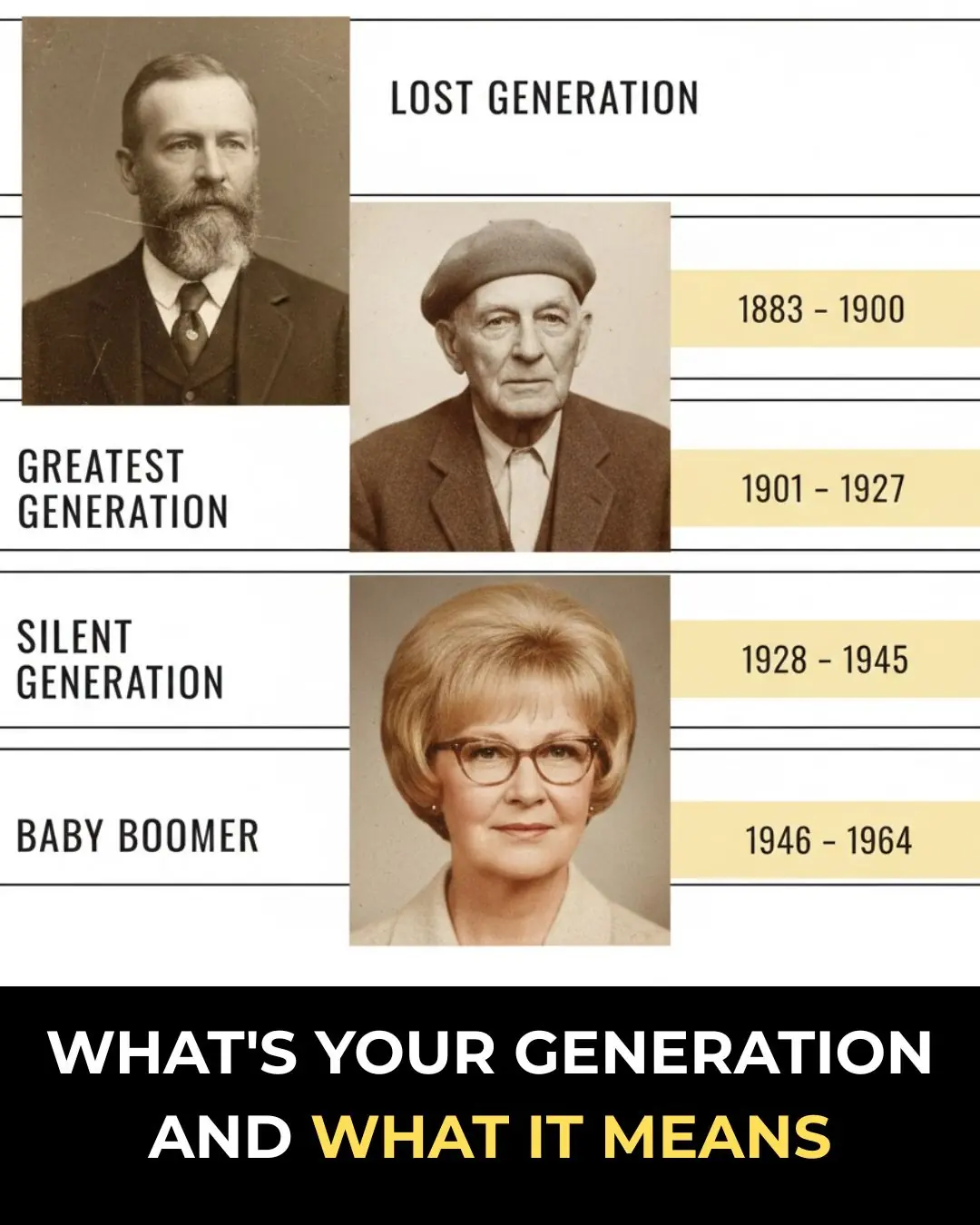
What’s Your Generation and What It Means

Drink Coconut Water for 7 Consecutive Days and Notice Remarkable Health Benefits

11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?

Surprise Finding: How the Immune System May Prevent Us From Burning Fat
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

Bula Choudhury: A Masterclass in Resilience and the Quiet Pursuit of Greatness 🌊✨

Targeted Violence in Khulna: A Growing Crisis for Law and Order ⚠️🇧🇩

When One Moment Changes Everything: A Story of Love, Trust, and Betrayal 🎶⚡💔
