One little-known nutrient that could ease fibromyalgia, chronic pain & nerve damage



Have you ever wondered whether the pain of fibromyalgia might not actually come from the muscles or joints at all, but instead from damaged or dysfunctional nerves? If that’s the case, could fibromyalgia be treated in a similar way to other forms of neuropathic pain? Today, we’ll explore a growing body of evidence suggesting that, for a subset of people, fibromyalgia pain may be driven by a condition known as small fiber neuropathy (SFN).
Fibromyalgia is often described as a rheumatic or musculoskeletal condition, characterized by widespread pain, stiffness, and fatigue. However, this traditional view may not tell the whole story. Emerging research suggests that fibromyalgia pain may originate within the nervous system itself—specifically the brain, spinal cord, and peripheral nerves. Understanding this neurological perspective opens the door to new treatment strategies, including the use of a lesser-known but promising nutrient called agmatine.
(This discussion draws on the work and clinical insights of nutritional therapist Elliot Overton.)
Key Takeaways
-
Fibromyalgia pain may be linked to small fiber neuropathy in a significant subset of patients.
-
Small fiber neuropathy affects pain- and temperature-sensing nerves, leading to symptoms such as burning pain, touch sensitivity, numbness, and tingling.
-
SFN can also disrupt autonomic nervous system functions, influencing sweating, digestion, bladder control, and heart rhythm.
-
Common causes include diabetes, autoimmune disease, infections, alcohol exposure, medications, celiac disease, and deficiencies in nutrients such as vitamin B12 and thiamine.
-
Multiple studies suggest that 30–40% of people diagnosed with fibromyalgia show objective signs of small fiber neuropathy.
-
Pain signaling relies heavily on glutamate and NMDA receptors within the spinal cord and brain.
-
Agmatine, a compound derived from arginine, may help reduce neuropathic pain by modulating these pathways.
Understanding Small Fiber Neuropathy
So what exactly is small fiber neuropathy? SFN is a form of nerve damage that affects small, unmyelinated nerve fibers, which are responsible for transmitting sensations such as pain, temperature, and light touch. Unlike large-fiber neuropathies, SFN often doesn’t show up on standard nerve conduction studies, making it easy to overlook.
When these small fibers are damaged or dysfunctional, a wide range of symptoms can appear, including:
-
Extreme sensitivity to touch (allodynia): Even gentle contact may feel painful
-
Burning or stinging pain: Often persistent and difficult to ignore
-
Numbness and tingling: Frequently described as “pins and needles”
-
Chronic, unexplained aches: Pain that seems disproportionate to physical findings
Beyond pain and sensory symptoms, SFN can also affect the autonomic nervous system, leading to issues such as:
-
Abnormal sweating (too much or too little)
-
Digestive problems, including constipation or diarrhea
-
Bladder dysfunction
-
Cardiovascular symptoms such as rapid heart rate or irregular rhythms
Common underlying causes of small fiber neuropathy include:
-
Diabetes and insulin resistance
-
Autoimmune disorders
-
Viral or bacterial infections
-
Chronic alcohol use
-
Medication toxicity
-
Celiac disease
-
Vitamin B12 deficiency
-
Thiamine (vitamin B1) deficiency
The Connection Between Fibromyalgia and Neuropathy
Over the past decade, researchers have increasingly identified signs of small fiber neuropathy in people diagnosed with fibromyalgia. Some studies suggest that up to 30% of fibromyalgia patients meet diagnostic criteria for SFN. In one notable study using skin biopsies, 41% of fibromyalgia patients showed evidence of small fiber nerve damage.
Similar findings have been observed in conditions such as complex regional pain syndrome and other chronic, widespread pain disorders. This challenges the idea that fibromyalgia is purely a musculoskeletal condition and instead points toward a disorder of pain processing and nerve signaling.
How Pain Signals Become Amplified
Pain signals begin in peripheral nerves, travel to the spinal cord, and are then transmitted to the brain, where they are interpreted as pain. When this signaling system becomes dysregulated, pain can persist even in the absence of ongoing tissue damage.
A key chemical messenger in this process is glutamate, which activates NMDA receptors in the spinal cord and brain. When these receptors are overstimulated, pain signals are amplified—a process known as pronociception.
Normally, the brain also sends inhibitory signals down the spinal cord to reduce pain, a mechanism called antinociception. In chronic pain conditions like fibromyalgia, this balancing system may fail: pain signals are turned up, while pain-inhibiting signals are turned down.
The Role of the Dorsal Root Ganglia
An especially important structure in this process is the dorsal root ganglia (DRG)—clusters of sensory nerve cell bodies located alongside the spinal cord. Dysfunction within the DRG has been strongly associated with small fiber neuropathy.
Following an initial trigger such as injury, infection, or nutritional deficiency, neurons in the DRG may undergo abnormal sprouting, becoming hypersensitive to stress-related chemicals like catecholamines. This leads to neuronal hyperexcitability, meaning pain signals fire too easily and too often.
This mechanism helps explain why stress frequently worsens fibromyalgia symptoms. Activation of the sympathetic “fight-or-flight” response can directly provoke pain by stimulating these sensitized neurons. Combined with impaired pain inhibition from the brain, this creates a self-sustaining cycle of chronic pain.
Agmatine: A Promising Support for Neuropathic Pain
Given this neurological model of fibromyalgia pain, therapies that calm overactive nerve signaling may be particularly helpful. While high-dose thiamine has shown benefit in some cases, another intriguing compound is agmatine.
Agmatine is produced naturally in the body from the amino acid arginine and has several neuroprotective properties. Research suggests it may be especially useful in neuropathic pain conditions.
Agmatine works through multiple mechanisms:
-
NMDA receptor inhibition: It dampens the pain-amplifying NMDA receptors
-
Reduced glutamate release: Lowering excitatory signaling in the nervous system
-
Activation of GABA-A receptors: Enhancing inhibitory, calming signals in the brain
-
Neuroprotective effects: Supporting cell survival, reducing inflammation, and limiting oxidative stress
Studies indicate that agmatine may help relieve pain associated with small fiber neuropathy, spinal cord injury, and tactile allodynia—conditions that share similar pain pathways with fibromyalgia.
Dosage and Practical Considerations
Research typically uses agmatine doses ranging from 1,000 to 2,000 mg per day, often divided into multiple doses. When combined with other supportive strategies—such as nutrient repletion, stress regulation, and addressing underlying causes—many individuals report meaningful improvements in pain and quality of life.
It’s important to note that while agmatine can significantly reduce symptoms, it may not address the root cause of nerve dysfunction. Identifying and treating underlying contributors such as nutrient deficiencies, metabolic issues, or immune dysfunction remains essential.
Final Thoughts
In summary, fibromyalgia pain may not be purely muscular in origin. For many individuals, it may reflect small fiber neuropathy and dysregulated pain signaling within the nervous system. Overactivation of glutamate and NMDA receptors, combined with impaired pain inhibition, can create persistent and severe pain.
Agmatine offers a promising tool to help rebalance these pathways and reduce pain intensity. While it should not replace comprehensive medical care, it may serve as a valuable part of a broader, individualized treatment plan. As always, working with a knowledgeable healthcare professional is key to addressing both symptoms and root causes effectively.
News in the same category
5 Foods You Must Avoid If You Have High Blood Pressure
21 Effective Home Remedies for Kidney Stones to Relieve Pain Fast

People with heart problems should avoid these 4 things to reduce stimulation to the heart
12 Bizarre Symptoms of Vitamin D Deficiency You Need to Know

8 warning signs of colon cancer you should never ignore

The daily drink that helps clear blocked arteries naturally

This old school home remedy will soothe your back, joints & knee pain in just 7 days!

Sleep Apnea: Symptoms, Risks, and Treatment Solutions
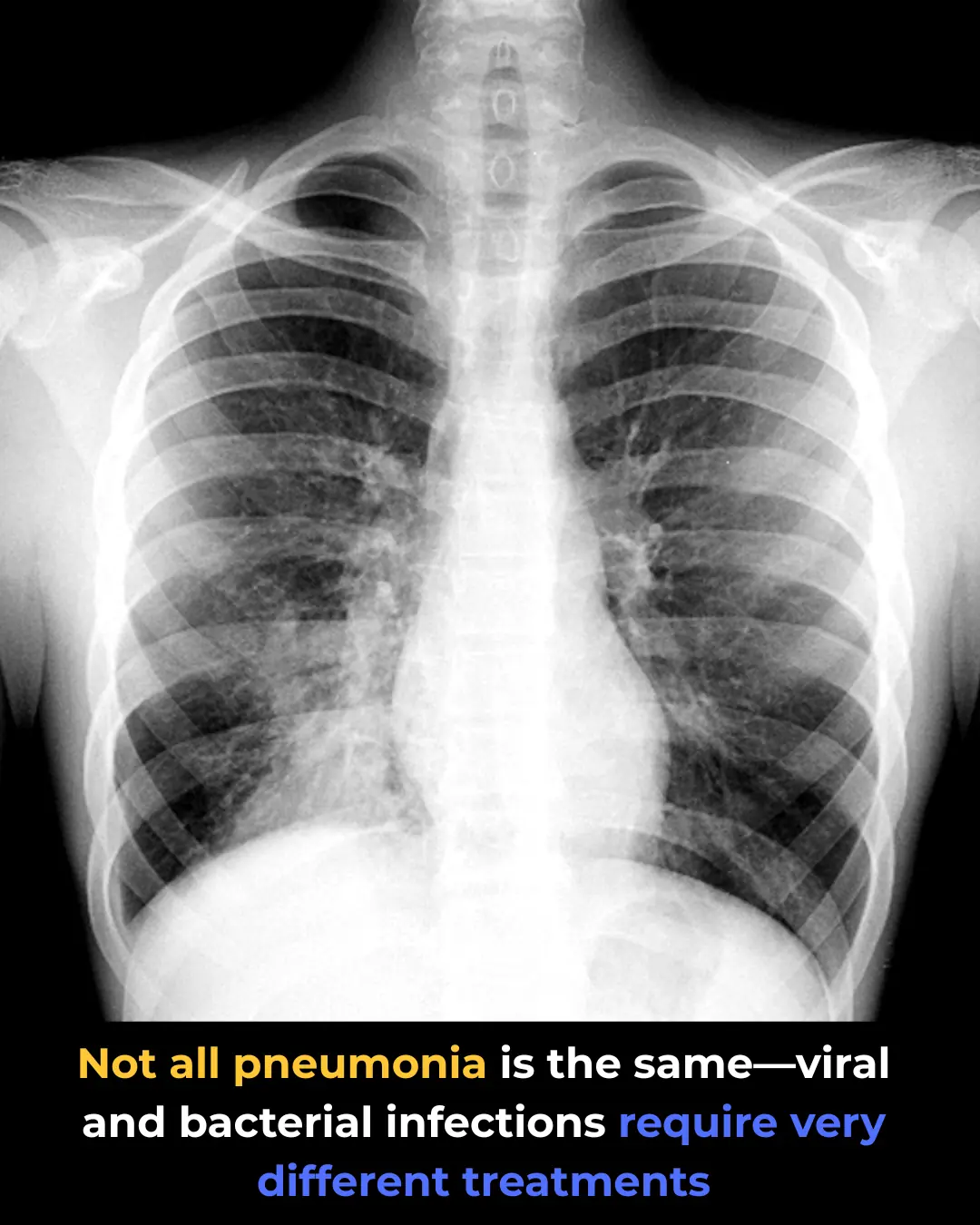
Viral Pneumonia vs. Bacterial Pneumonia: Key Differences

Allergic Rhinitis: What Triggers It and How to Manage It
COPD Exacerbation: Symptoms That Indicate a Flare-Up
Bile Reflux vs. Acid Reflux: Key Differences You Need to Know
Ulcerative Colitis vs. Crohn’s Disease: What Makes Them Different
How to lower blood sugar without giving up carbs

Top 8 warning signs of ovarian cancer women absolutely need to know
Don’t Ignore These Warning Signs of Vitamin B12 Deficiency!
Why you keep waking up with dry mouth—and what it may be telling you

Here’s What Eating Blueberries Every Day Does to Your Body, Says a Registered Dietitian
How To Get Rid Of Eczema: 13 Natural Remedies Backed By Research
News Post
Why This Doctor Chooses Not to Prescribe Statins for High Cholesterol — and What He Recommends Instead
5 Foods You Must Avoid If You Have High Blood Pressure
21 Effective Home Remedies for Kidney Stones to Relieve Pain Fast

Don’t Sleep With Your Pets
The Meaning of Having an Unmade Bed
Put a few ice cubes in the washing machine with your wrinkled clothes and do this, and you'll see an unexpected miracle.
A 2013 study conducted by researchers

Experienced tofu makers share tips on how to distinguish between clean tofu and tofu containing gypsum.

Don't put the purchased sấu fruit in the refrigerator right away: Follow this one extra step, and the sấu fruit will stay fresh and delicious for a whole year, retaining its original flavor.

How Retired Buses in France Are Becoming Mobile Book Rooms for Thoughtful Travel

How Turkey’s ‘Micro Animal Closets’ Are Offering Care to Stray Animals in Urban Parks

How Portugal Is Turning Urban Parking Towers into Night Shelters for the Homeless

How Retroftted City Buses Are Providing Warmth and Rest for the Homeless in Canada

People with heart problems should avoid these 4 things to reduce stimulation to the heart
12 Bizarre Symptoms of Vitamin D Deficiency You Need to Know

8 warning signs of colon cancer you should never ignore

The daily drink that helps clear blocked arteries naturally

This old school home remedy will soothe your back, joints & knee pain in just 7 days!

Sleep Apnea: Symptoms, Risks, and Treatment Solutions