Understanding Fatty Liver Disease: Risk Factors and Early Signs
How Can You Tell If You Have Fatty Liver Disease? 🤔
This is a question I receive very frequently on my social media platforms, so today I would like to explain it clearly and simply 👩🏻⚕️
Fatty liver disease refers to an abnormal accumulation of fat—mainly triglycerides—inside liver cells. Under normal conditions, the liver contains small amounts of fat, but when fat makes up more than 5–10% of the liver’s weight, it is considered fatty liver disease.
Many people with fatty liver disease experience few or no symptoms, especially in the early stages. Some individuals may notice persistent fatigue, low energy levels, or mild discomfort or pressure in the upper right side of the abdomen. Because symptoms are often subtle or absent, the condition may go unnoticed for years and is frequently discovered incidentally during routine blood tests or imaging studies such as ultrasound.
However, fatty liver disease should not be underestimated. In some cases, it can progress to more serious liver conditions, including inflammation (steatohepatitis), fibrosis, and eventually cirrhosis, which may significantly impair liver function and increase the risk of liver failure or liver cancer.
Common Causes of Fatty Liver Disease
The most frequent causes of fatty liver disease in the United States and other Western countries include:
-
Excessive alcohol consumption
-
Overweight and obesity
-
Metabolic disturbances such as insulin resistance (commonly seen in type 2 diabetes), elevated blood triglycerides, and high cholesterol levels
-
Exposure to certain toxins
-
Use of specific medications, including corticosteroids, tamoxifen, and some chemotherapy drugs
-
Inherited metabolic disorders
-
Pregnancy (in rare cases)
When excess body weight, insulin resistance, and high levels of triglycerides and/or cholesterol occur together, this condition is known as metabolic syndrome. Metabolic syndrome plays a key role in the development of non-alcoholic fatty liver disease (NAFLD), as it alters the way the body processes and stores fat.
In these situations, fat accumulates in liver cells either because the body produces more fat than it can handle or because fat metabolism and excretion become inefficient. Over time, this excess fat is stored within liver cells, leading to fatty liver disease.
It is important to note that eating a high-fat diet alone does not directly cause fatty liver disease. Instead, the condition is strongly linked to overall metabolic health, lifestyle factors, and insulin resistance rather than fat intake by itself.
How Is Fatty Liver Disease Diagnosed?
Diagnosis usually involves a combination of:
-
Blood tests showing elevated liver enzymes
-
Imaging studies such as abdominal ultrasound, CT scan, or MRI
-
In some cases, specialized tests or a liver biopsy to assess the degree of inflammation or fibrosis
Trusted Medical Sources
The information in this article is supported by well-established medical institutions, including:
-
World Health Organization (WHO)
-
Mayo Clinic
-
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
-
Harvard Medical School – Harvard Health Publishing
-
American Liver Foundation
These organizations emphasize that early detection and lifestyle changes—such as weight management, balanced nutrition, regular physical activity, and limiting alcohol intake—are key to preventing disease progression.
In addition to lifestyle factors, genetics and hormonal changes may also influence the development of fatty liver disease. Some individuals are more genetically predisposed to storing fat in the liver, even when they do not appear significantly overweight. Hormonal shifts, particularly during pregnancy or menopause, can temporarily affect fat metabolism and liver function, increasing susceptibility in certain cases.
The good news is that fatty liver disease is often reversible, especially in its early stages. Scientific evidence consistently shows that modest weight loss—typically 5–10% of total body weight—can significantly reduce liver fat and improve liver enzyme levels. Regular physical activity improves insulin sensitivity, helping the liver process and export fat more efficiently. Even moderate exercise, such as brisk walking for 30 minutes most days of the week, can make a meaningful difference.
Nutritional quality also plays a crucial role. Diets rich in whole foods—such as vegetables, fruits, whole grains, lean proteins, and healthy fats—support liver health and metabolic balance. Reducing the intake of ultra-processed foods, refined carbohydrates, and sugary beverages is particularly important, as these foods contribute to insulin resistance and excess fat production in the liver. According to Harvard Health Publishing and the American Liver Foundation, limiting added sugars—especially fructose—can help slow or reverse fatty liver progression.
For individuals who consume alcohol, reducing or eliminating alcohol intake is essential. Even moderate alcohol consumption can worsen liver damage when fatty liver disease is already present. Medical follow-up is also important, especially for people with diabetes, obesity, or abnormal cholesterol levels, as managing these conditions lowers the risk of long-term liver complications.
Ultimately, fatty liver disease is not only a liver condition—it is a reflection of overall metabolic health. Early awareness, proper diagnosis, and sustainable lifestyle changes can protect the liver and prevent progression to more severe disease.
News in the same category
🧬 What Makes This Vaccine Different?
Onion Juice and Alopecia Areata: Expanded Overview

Mix garlic with milk and you will thank me

Discover the Power of a Leaf That Can Support Your Well-being 💪

Euphorbia Hirta: Exploring the Remarkable Potential of a Traditional Plant for Respiratory & Whole-Body Support

The Hidden Banana Blossom: Nature’s Secret Weapon Against Diabetes, High Blood Pressure, and Chronic Stomach Pain

Natural Energy Tonic: Ginger + Tomato

WHO Classified Processed Meats as Cancer-Causing Foods, and Here’s What You Should Know
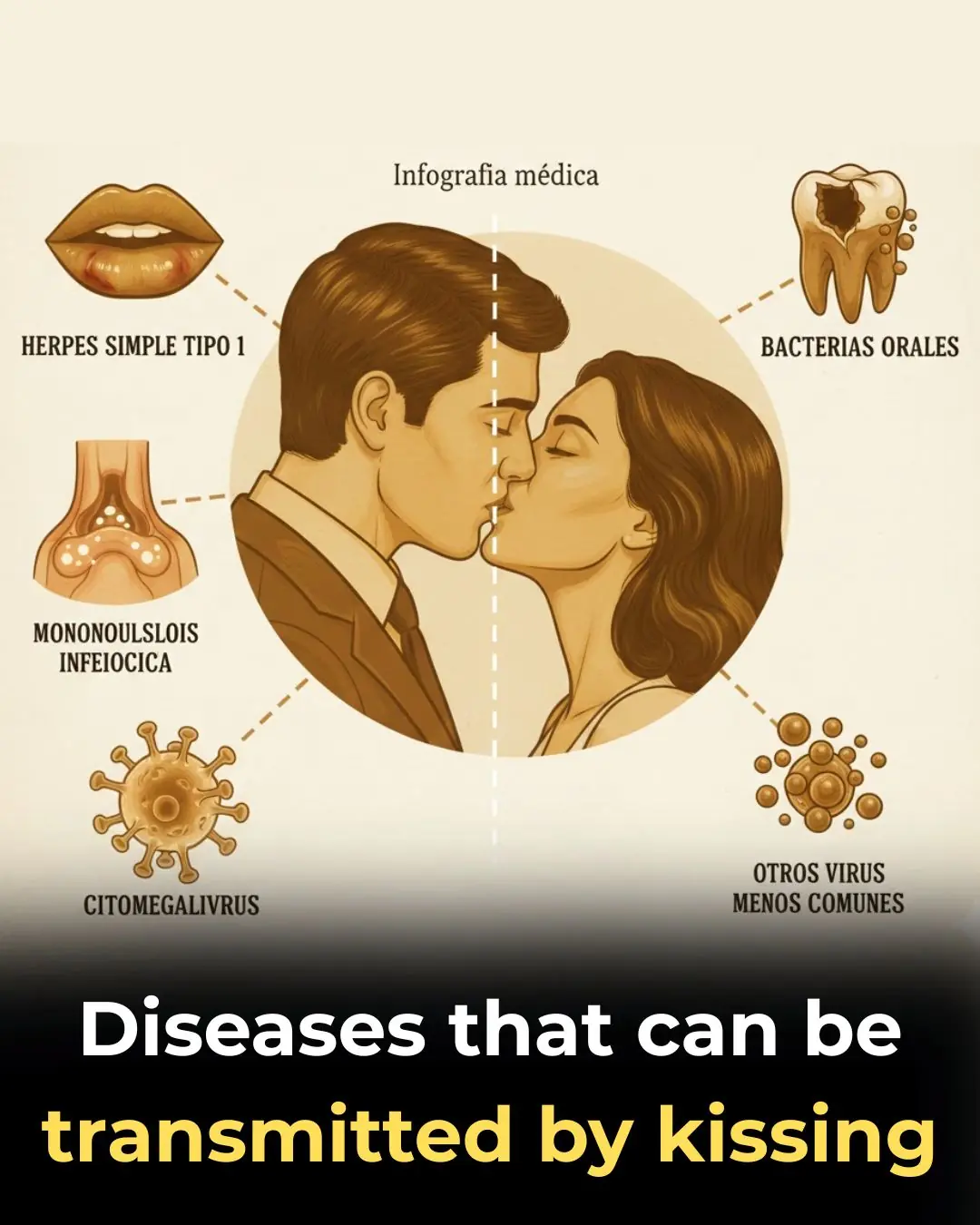
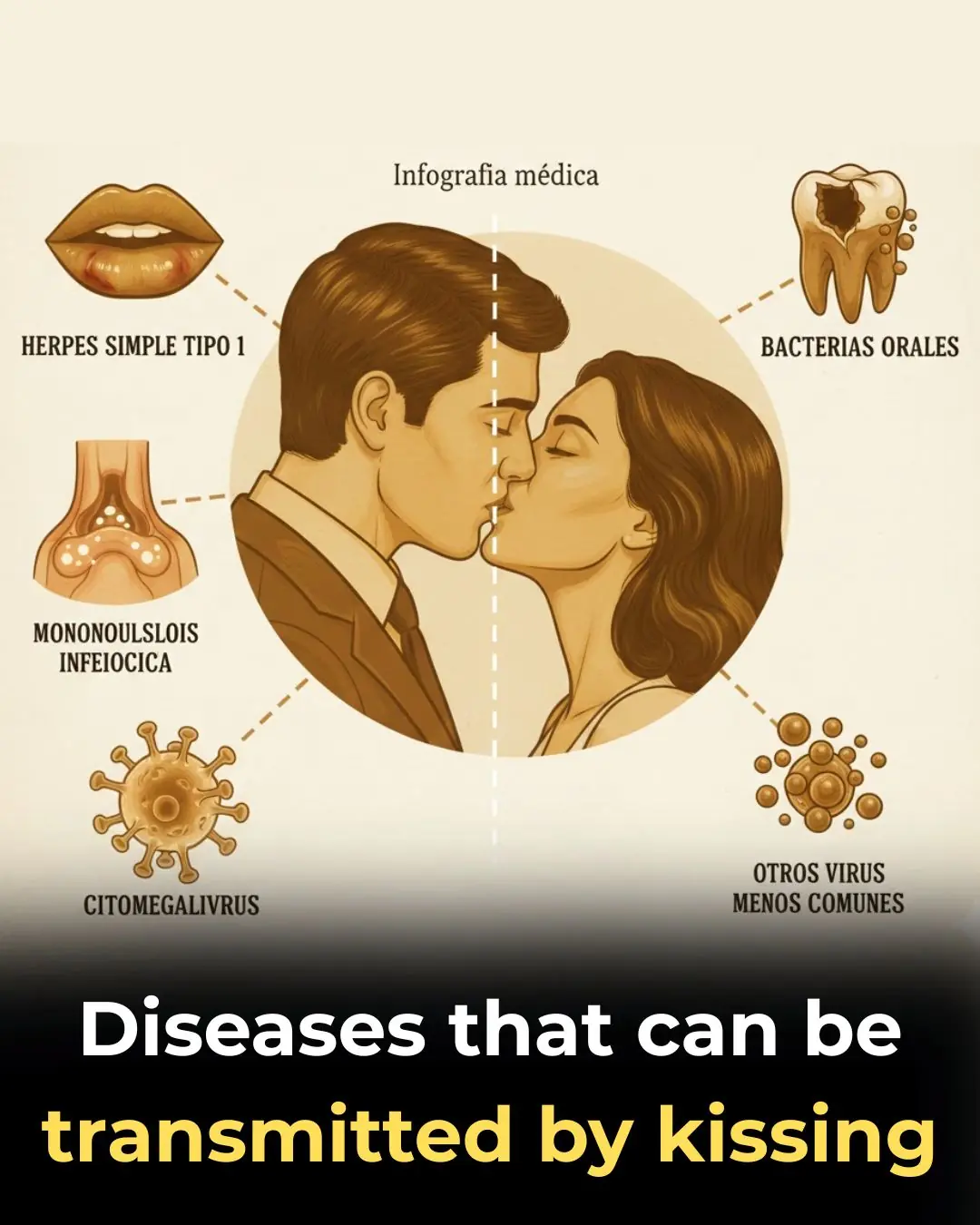
Health Risks Associated With Kissing: Common Infections to Be Aware Of
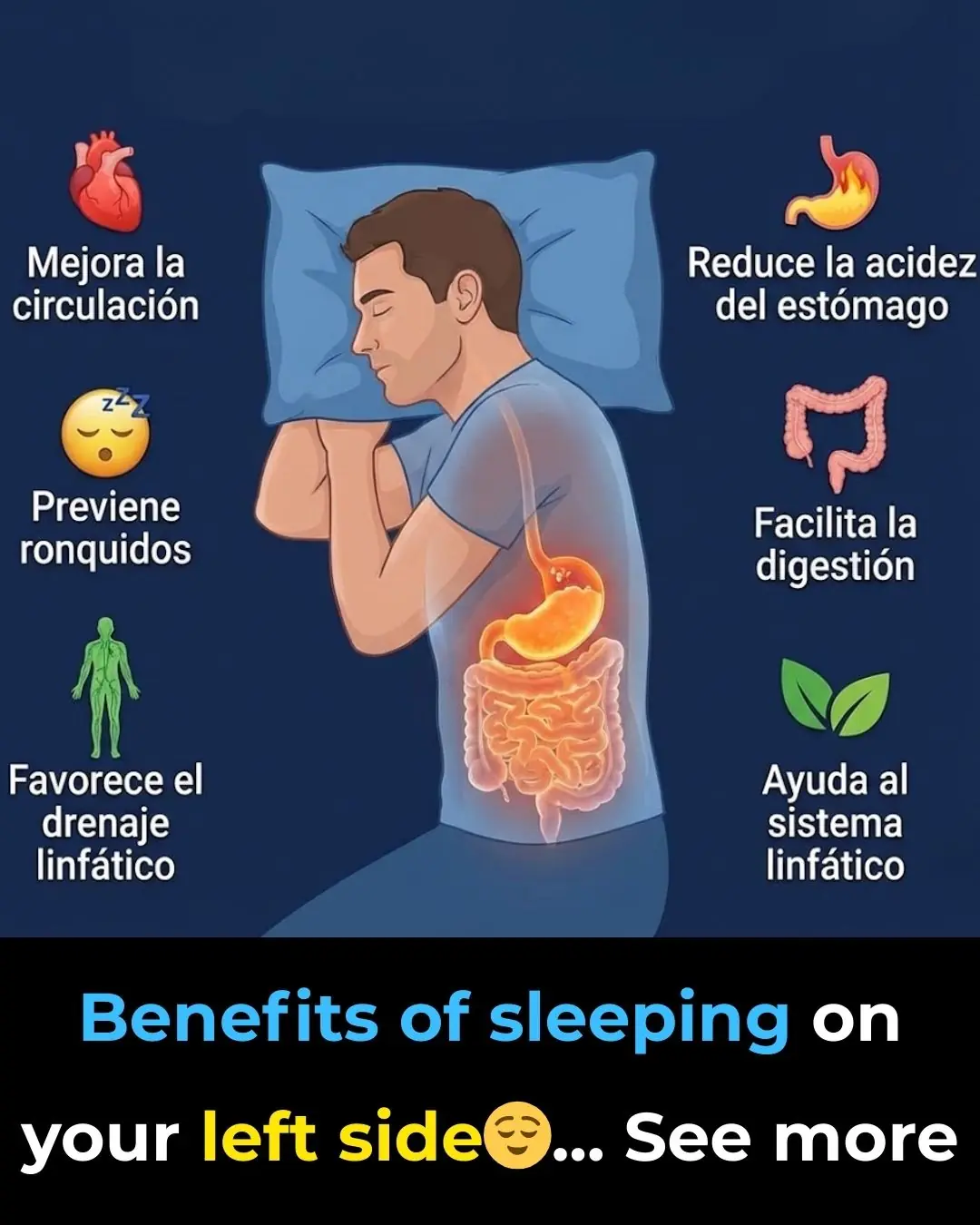
Is it better to sleep on your right or left side? Here's what science says
The best foods for a happy menopause
If you notice this insect in your home, call professional pest control services immediately
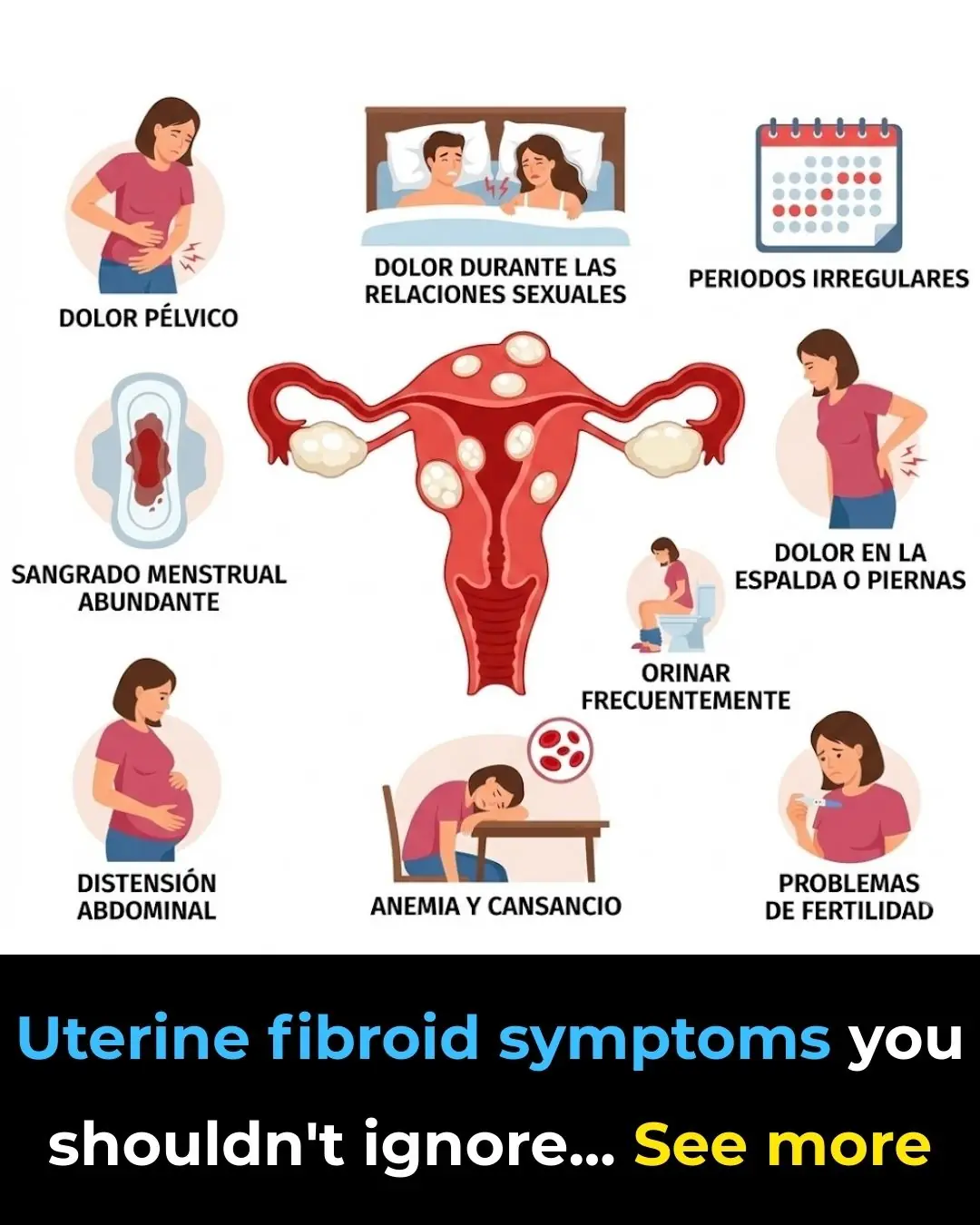
Uterine fibroids: 5 things we should know
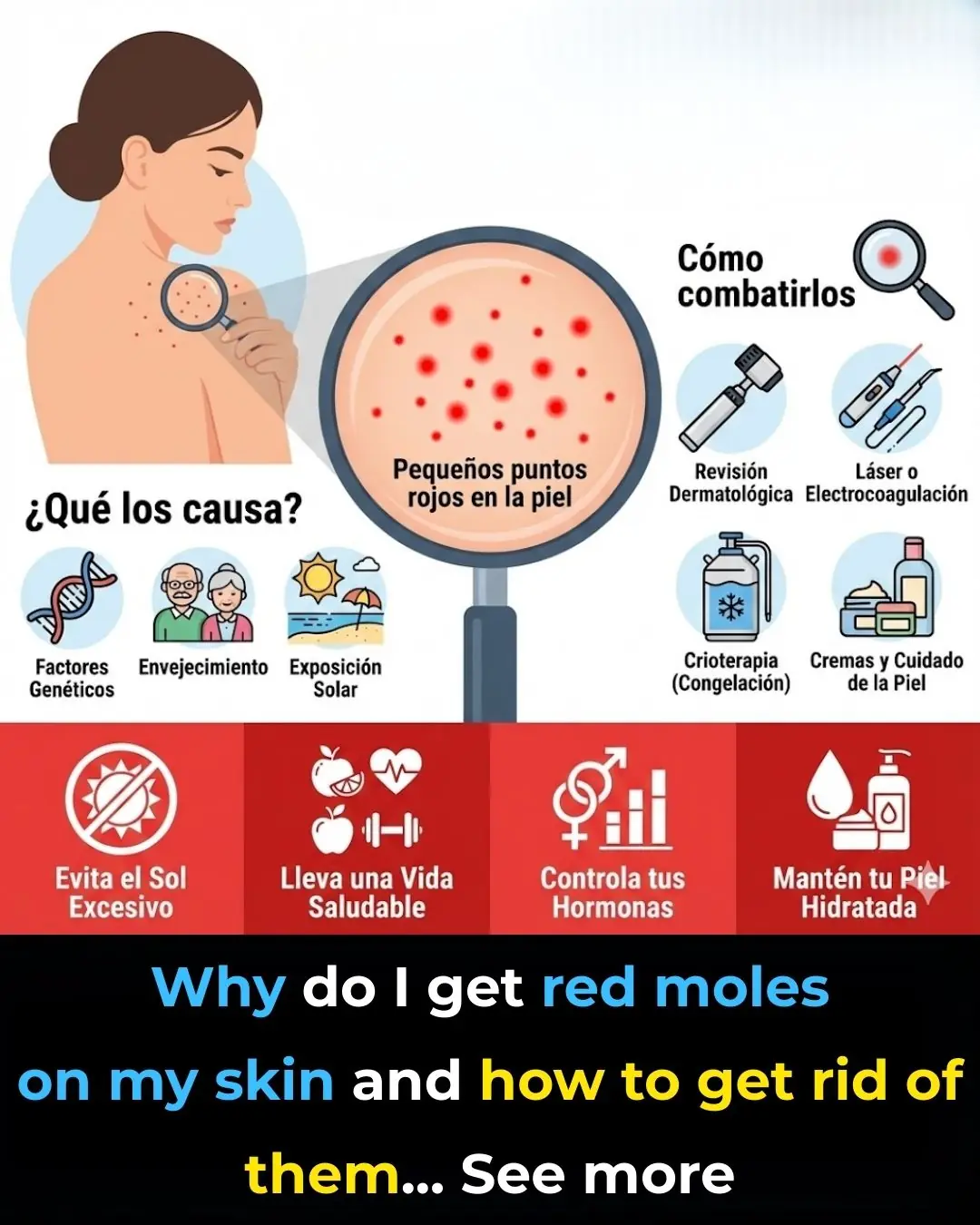
Why do red moles appear on the skin? Here's what science says
18 Signs of Histamine Intolerance (and what causes it)

Fig Leaves: Discover studies and ways to use this powerful plant

Doctors Reveal: Drinking Coconut Water May Cause…
What Happens to Your Body If You Eat One Garlic Bulb a Day? It’s Amazing!
News Post
Cannabis Compounds and Ovarian Cancer: Expanded Overview
🧪 Key Findings from the Mouse Study
🧬 What Makes This Vaccine Different?

🌟 Breakthrough in Cancer Treatment: Targeted Light Therapy
Onion Juice and Alopecia Areata: Expanded Overview

Mix garlic with milk and you will thank me

Discover the Power of a Leaf That Can Support Your Well-being 💪

Euphorbia Hirta: Exploring the Remarkable Potential of a Traditional Plant for Respiratory & Whole-Body Support

The Hidden Banana Blossom: Nature’s Secret Weapon Against Diabetes, High Blood Pressure, and Chronic Stomach Pain

Natural Energy Tonic: Ginger + Tomato
She Pushed Him Out of the Office. She Had No Idea Who He Was

WHO Classified Processed Meats as Cancer-Causing Foods, and Here’s What You Should Know
He didn’t know what was happening behind his back while he was serving the nation.

STAY AWAY FROM MY MOTHER. OR ELSE..
HHS to Reexamine Cell Phone and 5G Radiation Risks Following Direction From RFK Jr
His Teacher Noticed One Detail That Saved His Life

I RAISED HER. I WARNED HER, I LOST HER

Poor Cleaner Pays Bus Fare For A Stranded Stranger, Unaware He’s A Billionaire Who Was…