Are Vaccines Doing More Than Just Preventing Infection?
For decades, vaccines have been evaluated and approved based on a straightforward principle: a vaccine protects against the specific disease it is designed to prevent. Measles vaccines prevent measles. Polio vaccines prevent polio. Tuberculosis vaccines help protect against tuberculosis.
However, a growing body of scientific evidence suggests that this view may be incomplete.
Researchers around the world are increasingly documenting “non-specific” or “off-target” effects of certain vaccines—particularly live attenuated vaccines—that appear to influence overall health in ways that go beyond protection against a single pathogen. These findings are reshaping how scientists think about immunity, public health impact, and vaccine policy.
This article explores what these broader effects are, what the evidence shows, and why they matter—while staying firmly grounded in established science.
What Are Non-Specific Effects of Vaccines?
Non-specific effects (NSEs) refer to health impacts of vaccines that are not directly related to preventing the target disease. Instead, these effects may influence:
-
Overall immune system readiness
-
Susceptibility to unrelated infections
-
Inflammation and immune regulation
-
All-cause mortality, especially in children
These effects are not universal across all vaccines and are most consistently observed with live attenuated vaccines, which contain a weakened but replicating form of a virus or bacterium.
Examples of live attenuated vaccines include:
-
Measles vaccine
-
Oral polio vaccine (OPV)
-
Bacillus Calmette–Guérin (BCG) vaccine for tuberculosis
Evidence From Population and Clinical Studies
Reduced All-Cause Mortality in Children
One of the most striking observations comes from long-term population studies in low- and middle-income countries. In several settings, children who received live vaccines—particularly measles and BCG vaccines—experienced lower overall mortality than could be explained by prevention of the target disease alone.
For example:
-
In some regions, measles vaccination was associated with fewer deaths from respiratory and gastrointestinal infections.
-
BCG vaccination in newborns has been linked to reduced rates of neonatal sepsis and pneumonia.
These findings have been observed repeatedly across different populations, although the magnitude of the effect varies by context.
Protection Against Unrelated Infections
Research suggests that live vaccines may “train” the innate immune system, enhancing its ability to respond more effectively to a wide range of pathogens.
This phenomenon, often referred to as trained immunity, involves:
-
Epigenetic changes in immune cells
-
Increased responsiveness of macrophages and natural killer (NK) cells
-
Faster, stronger early immune reactions to infections
Unlike traditional immune memory (which is highly specific), trained immunity is broad and non-specific, potentially explaining why vaccinated individuals may fare better against unrelated infections.
How Could Vaccines Produce These Effects?
Beyond Antibodies: A Broader Immune Reset
Traditional vaccine evaluation focuses heavily on antibody levels. While antibodies are critical, they represent only one part of the immune system.
Live attenuated vaccines appear to:
-
Activate innate immune cells more strongly
-
Influence cytokine production and inflammatory pathways
-
Modify immune system development, especially in early life
These changes may result in a more balanced and resilient immune response, reducing the severity of future infections—even when they are caused by unrelated pathogens.
Differences Between Live and Non-Live Vaccines
It is important to be precise and evidence-based:
-
Live attenuated vaccines are most strongly associated with beneficial non-specific effects.
-
Inactivated or subunit vaccines (such as many modern vaccines) do not consistently show the same broad effects—though they are extremely effective at preventing their target diseases.
This distinction does not imply that one type is “better” overall. Each vaccine is designed for a specific purpose, safety profile, and population need.
Implications for Vaccine Policy and Scheduling
These findings raise important but complex questions:
-
Should vaccine schedules consider overall immune effects, not just disease-specific outcomes?
-
Does the order in which vaccines are given matter?
-
Could some vaccines be strategically used to strengthen early-life immunity?
Organizations such as the World Health Organization acknowledge the scientific interest in non-specific effects, while emphasizing that current immunization programs are based on strong evidence of safety and disease prevention.
At present:
-
Vaccine schedules are not changed solely based on non-specific effects.
-
More randomized controlled trials are underway to clarify causality and mechanisms.
-
Policymakers remain cautious, prioritizing proven benefits while monitoring emerging data.
What This Does Not Mean
It is crucial to address potential misunderstandings:
-
These findings do not suggest that vaccines are experimental or poorly understood.
-
They do not imply that vaccines should be used indiscriminately for unrelated diseases.
-
They do not undermine vaccine safety or effectiveness.
Instead, they highlight that vaccines may have additional positive effects that science is only beginning to understand.
The Future of Vaccine Research
As immunology advances, researchers are increasingly viewing vaccines not only as disease-specific tools, but also as immune modulators.
Future research may lead to:
-
Improved vaccine design that leverages trained immunity
-
Better timing and sequencing of vaccines in early childhood
-
New strategies for protecting vulnerable populations
What remains clear is this: vaccines already save millions of lives each year, and understanding their full range of effects may allow them to save even more.
Conclusion
Once seen as narrowly targeted interventions, vaccines are now being recognized as complex biological tools that interact deeply with the immune system. Evidence suggests that some widely used vaccines—particularly live attenuated ones—may provide health benefits beyond their intended purpose, including reduced mortality and improved resistance to other infections.
While these effects do not change current vaccination recommendations, they open an important and promising field of research—one that may ultimately strengthen public health worldwide.
In science, asking better questions leads to better answers. And vaccines, it seems, may still have more to teach us.
News in the same category

Stop fighting with your eyeliner. 10 winter proof tricks seniors swear by
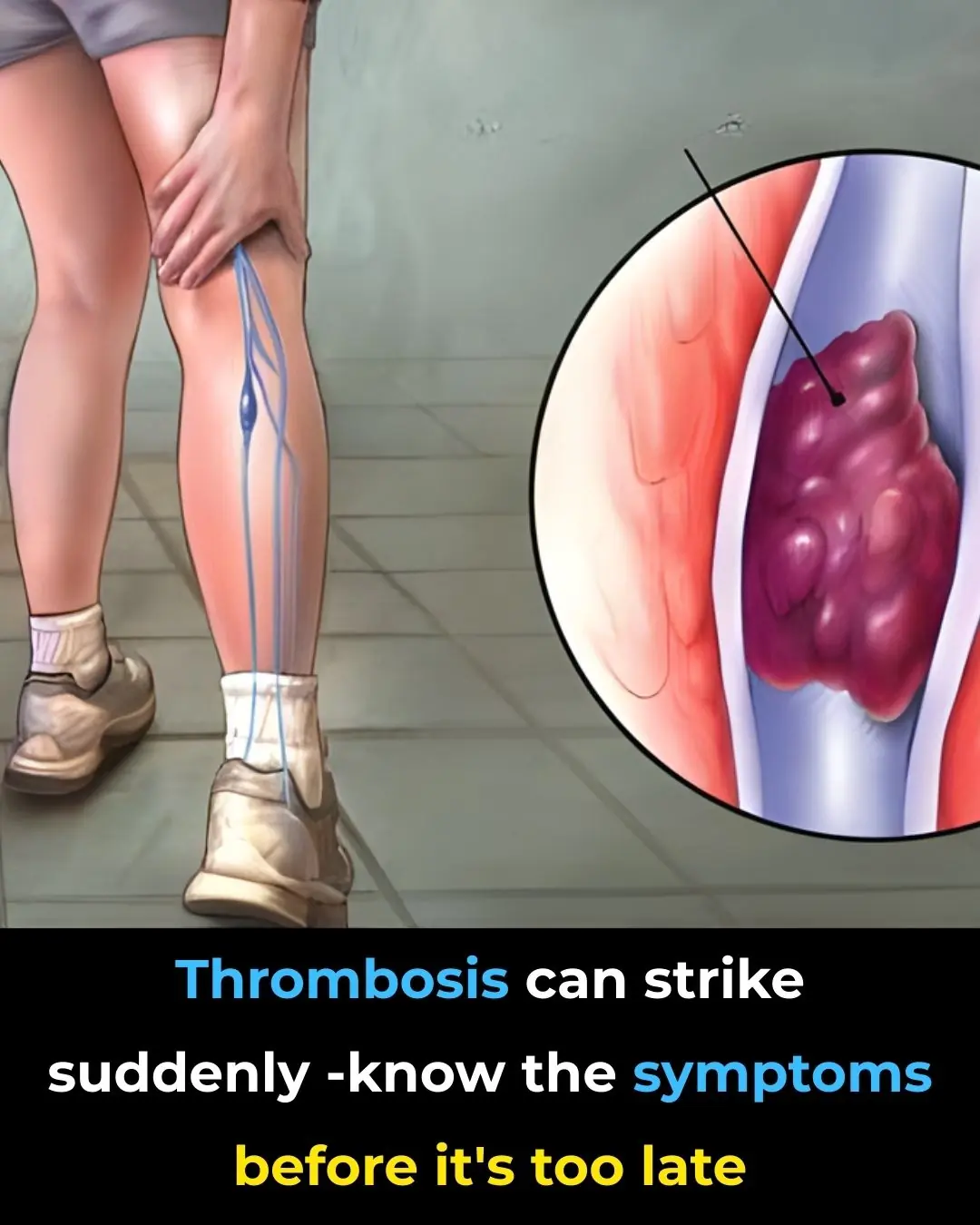
Deep Vein Thrombosis: A Silent Killer That You Need to Know

Pineapple: Proven Health Benefits, Calories, Juice Benefits
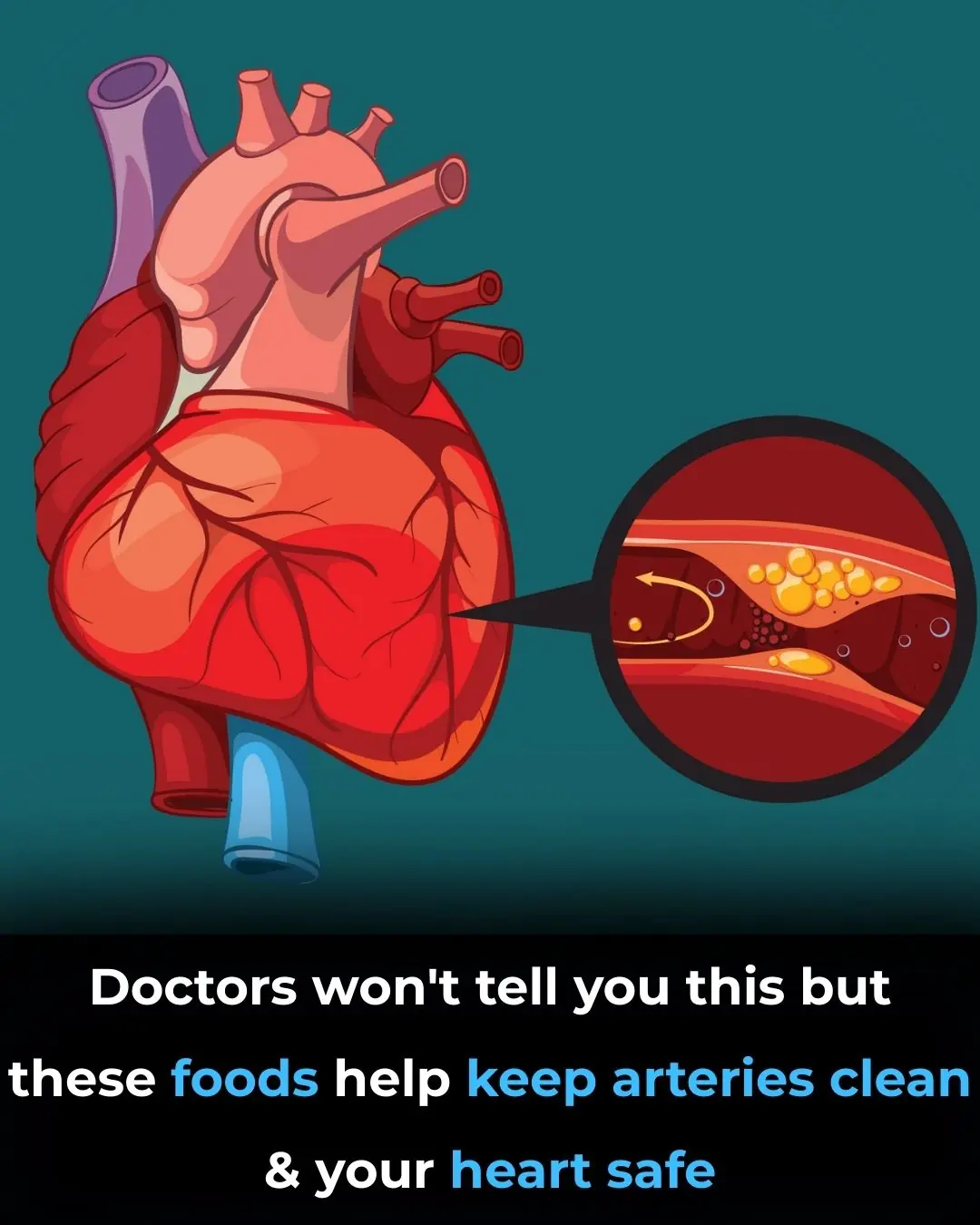
The Best Foods to Cleanse and Prevent Clogged Arteries

13 Warning Signs of High Blood Sugar and 9 Ways to Take Control of Your Health
Progress Fighting Pancreatic Cancer — One of the Deadliest Malignancies

Avoid This Drink to Reduce The Risk of Stroke and Heart Attack

Drinking about 3 cups of green tea per day is associated with fewer white matter lesions in the brain—changes linked to aging and dementia risk

Magnesium Supplementation and Rapid Improvement in Major Depression

Targeting Fat Metabolism in Acute Myeloid Leukemia Stem Cells: The Therapeutic Potential of Avocadyne
High-Dose Thiamine and Fatigue Relief in Hashimoto’s Disease: Insights from a Case Series
Psilocybin and the Biology of Aging: Emerging Experimental Evidence
Aspirin as an Immune-Modulating Agent in the Suppression of Cancer Metastasis

Gum disease bacteria found in alzheimer’s brains

Fecal Microbiota Transplantation and Its Potential Role in Severe Autism Spectrum Disorder

Raw Carrots and Their Impact on Cholesterol and Colon Function

Breakthrough in Pancreatic Cancer Immunotherapy
Blue Blood in the Ocean: How Horseshoe Crabs Help Protect Human Health
News Post

Pour a handful of salt into the toilet bowl

Trick To Stop Mosquito Bite From Itching
Sudden Confusion or Trouble Speaking: When It’s More Than Just Fatigue
A Family of Four Diagnosed With Liver Cancer: Experts Identified the Cause the Moment They Entered the Kitchen

My nana says this works like a charm

Stop fighting with your eyeliner. 10 winter proof tricks seniors swear by
Did not know this

My scalp is red, itchy, and flaky — and my doctor can’t see me until after the holidays. What could this be?
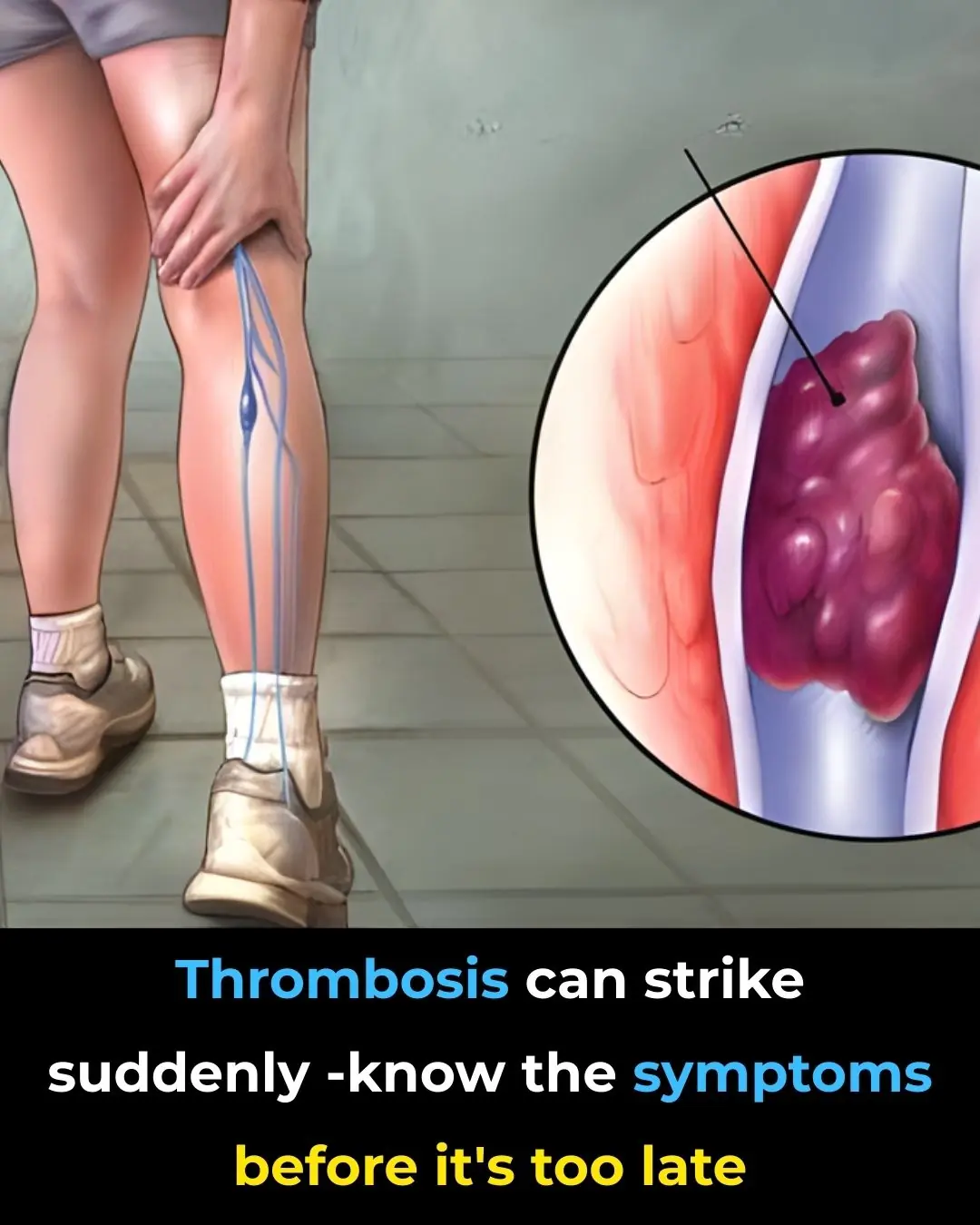
Deep Vein Thrombosis: A Silent Killer That You Need to Know

Pineapple: Proven Health Benefits, Calories, Juice Benefits
The Best Foods to Cleanse and Prevent Clogged Arteries

13 Warning Signs of High Blood Sugar and 9 Ways to Take Control of Your Health
Progress Fighting Pancreatic Cancer — One of the Deadliest Malignancies

Avoid This Drink to Reduce The Risk of Stroke and Heart Attack
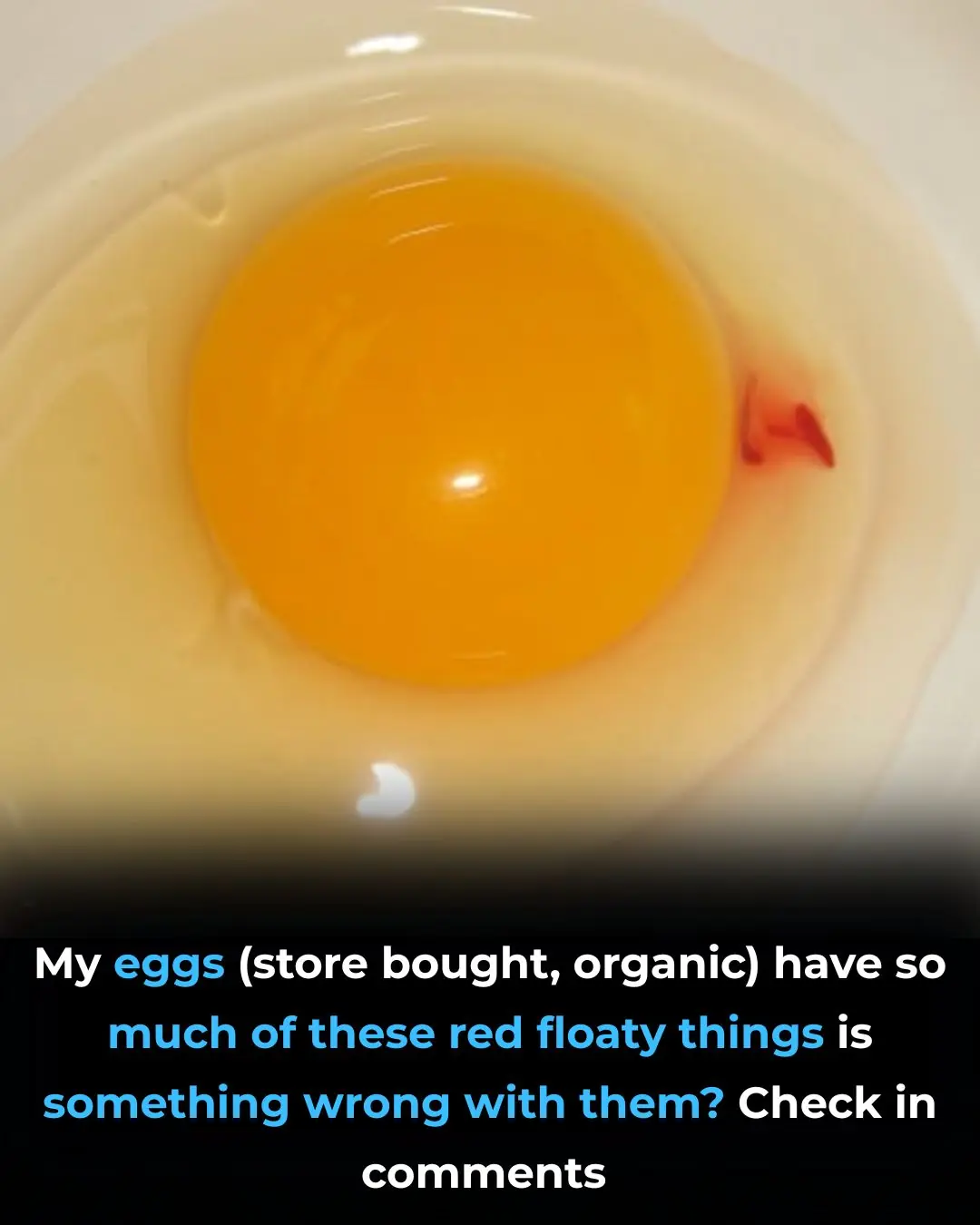
Should We Eat Eggs With BL00D Spots

Drinking about 3 cups of green tea per day is associated with fewer white matter lesions in the brain—changes linked to aging and dementia risk

Magnesium Supplementation and Rapid Improvement in Major Depression

Targeting Fat Metabolism in Acute Myeloid Leukemia Stem Cells: The Therapeutic Potential of Avocadyne