
Bee Propolis and Infertility in Endometriosis: Evidence from a Pilot Randomized Clinical Trial
Endometriosis is a common gynecological disorder characterized by the presence of endometrial-like tissue outside the uterus, leading to chronic inflammation, pelvic pain, and infertility. Even in its minimal or mild forms, endometriosis can significantly impair fertility through mechanisms such as local inflammation, altered immune responses, excessive estrogen production via aromatase activity, and abnormal angiogenesis. While surgical management and hormonal therapies are often used, safe, affordable, and fertility-supportive adjunct treatments remain limited. In this context, a pilot randomized clinical trial published in 2003 explored the potential of bee propolis as a novel therapeutic option for endometriosis-associated infertility.
The study was published in Fertility and Sterility (Volume 80, Supplement 3, September 2003) and employed a prospective, randomized, blinded, placebo-controlled design. Forty women with primary infertility lasting at least two years and laparoscopically confirmed minimal or mild endometriosis were enrolled. Immediately following diagnostic laparoscopy, participants were randomly assigned to receive either bee propolis at a dose of 500 mg twice daily or a matching placebo. The women were then followed for a period of nine months to assess pregnancy outcomes.
The biological rationale for using bee propolis in this setting was strong. Propolis is a complex resinous substance produced by bees, rich in flavonoids, phenolic acids, and other bioactive compounds. Experimental studies have shown that propolis possesses potent anti-inflammatory, antioxidant, immunomodulatory, and anti-angiogenic properties. Additionally, propolis has been reported to inhibit aromatase activity, potentially reducing local estrogen production—an important driver of endometriosis progression and persistence. These mechanisms directly target several of the pathophysiological processes believed to underlie endometriosis-related infertility.
The results of the trial were striking. The pregnancy rate in the propolis-treated group was 60%, compared with only 20% in the placebo group, a difference that was statistically highly significant (p < 0.001). Importantly, baseline characteristics such as age, duration of infertility, and disease severity were comparable between the two groups, strengthening the validity of the findings. Patient compliance with the supplementation regimen was reported as satisfactory, and no adverse effects were observed during the study period, indicating good tolerability and a favorable safety profile.
From a clinical perspective, these findings are notable for several reasons. First, the magnitude of the observed effect—a threefold increase in pregnancy rate—is unusually large for a non-hormonal, low-cost intervention. Second, the intervention was initiated immediately after laparoscopy, a time when inflammatory and angiogenic processes may be particularly active, potentially enhancing the impact of propolis’s biological actions. Third, unlike many conventional treatments, propolis does not suppress ovulation or require interruption of attempts to conceive, making it especially attractive for women actively trying to become pregnant.
Nevertheless, the authors were careful to acknowledge the limitations of the study. As a pilot trial, the sample size was small, and the study was conducted at a single center. The findings therefore cannot be considered definitive or broadly generalizable. Larger, multicenter randomized controlled trials would be required to confirm efficacy, determine optimal dosing and duration, and clarify which subgroups of patients are most likely to benefit. Additionally, while no adverse effects were reported, longer-term safety data would be valuable.
In conclusion, the 2003 pilot randomized, placebo-controlled trial published in Fertility and Sterility provides early but compelling clinical evidence that bee propolis supplementation (500 mg twice daily) may significantly improve pregnancy rates in women with infertility associated with minimal or mild endometriosis (Fertility and Sterility, 2003). By targeting inflammation, angiogenesis, immune dysregulation, and estrogen-related pathways, propolis represents a biologically plausible and well-tolerated adjunctive approach. Although confirmation in larger trials is essential, this study laid important groundwork for considering propolis as a low-cost, non-hormonal strategy in the management of endometriosis-related infertility.
News in the same category


Ginger Supplementation and Cardiovascular Inflammation: Evidence from a Double-Blind Randomized Clinical Trial
Antioxidant Supplementation and Thyroid Autoimmunity: Evidence from a Randomized Controlled Trial

Chios Mastic Gum as an Anti-Inflammatory Intervention in Crohn’s Disease and Vascular Inflammation

Garlic Supplementation and Metabolic Improvement in Non-Alcoholic Fatty Liver Disease
Potassium Deficiency – Causes, Symptoms and What To Do

14 Warning Signs of Low Magnesium Levels and What to Do About It (Science Based)
Proven Health Benefits of Beets and Fermented Beets (Science Based)

3 Reasons Onions Might Upset Your Stomach

MRI vs PET: Which Imaging Modality Better Detects Prostate Cancer Recurrence?
Hidden Spread of Pseudomonas aeruginosa From Lung to Gut in Hospitalized Patients
‘Tis the Season to Help People Avoid Holiday Heart Syndrome
Got a lump on your neck, back or behind your ear? This is what you need to know

What Your Skin Could Be Telling You About Hidden Health Issues
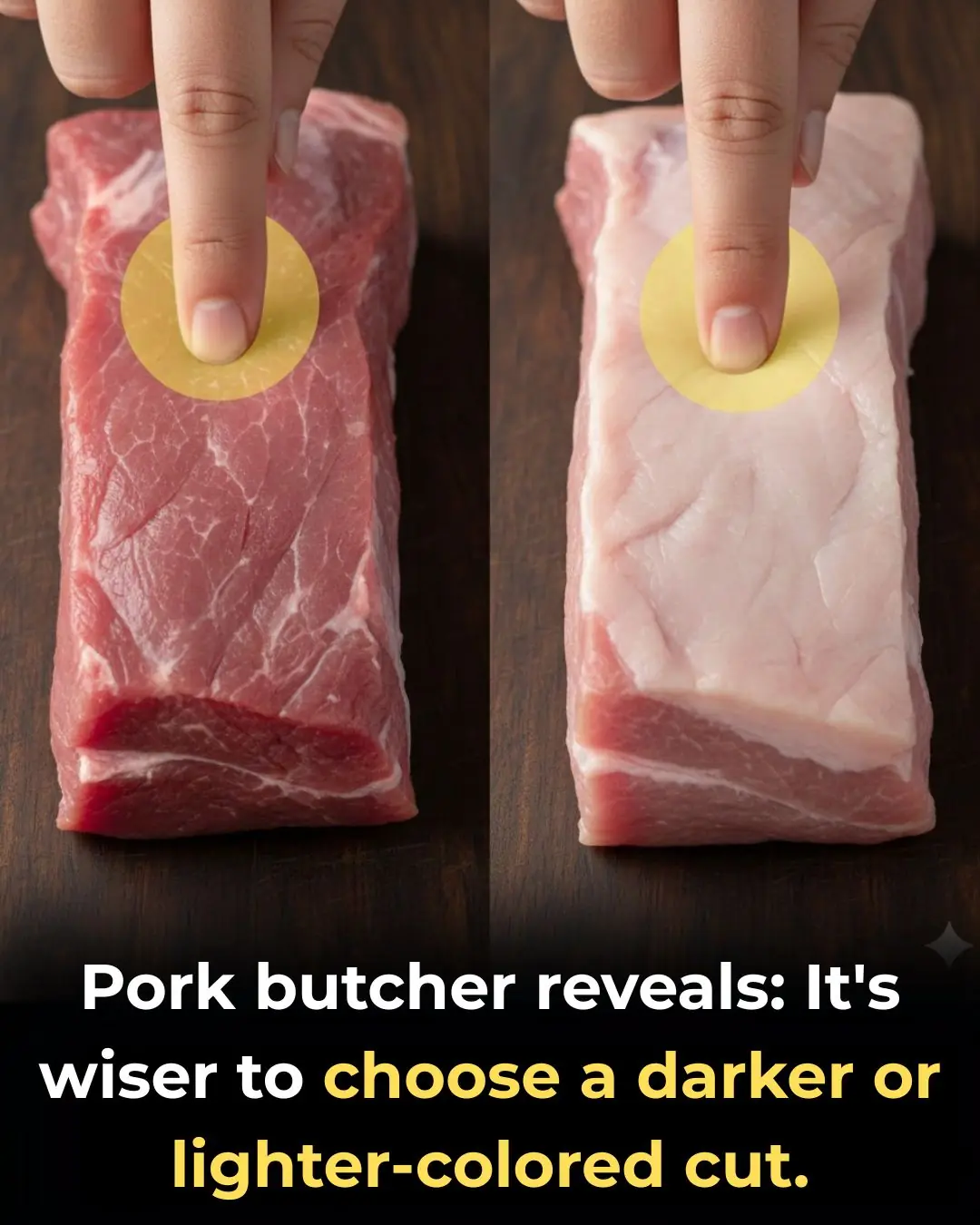
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?

4 Types of Vegetables Most Effective in Preventing Cancer, According to Doctors: Eating Them Regularly Is Great for Your Health
Stroke and Cerebral Infarction Prevention: Remember These 3 Indicators, 1 Disease, and 6 Key Habits

Optimism as a Psychosocial Predictor of Exceptional Longevity

Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health
News Post

Thymoquinone and Breast Cancer Cell Suppression: Evidence from Preclinical Research

Ginger Supplementation and Cardiovascular Inflammation: Evidence from a Double-Blind Randomized Clinical Trial
Antioxidant Supplementation and Thyroid Autoimmunity: Evidence from a Randomized Controlled Trial

Chios Mastic Gum as an Anti-Inflammatory Intervention in Crohn’s Disease and Vascular Inflammation

Garlic Supplementation and Metabolic Improvement in Non-Alcoholic Fatty Liver Disease
If you drink cucumber water every morning, this is what happens to your body

I soaked my feet in apple cider vinegar. 15 mins later, this is what happened

I need this ‘Liquid Gold.’
Potassium Deficiency – Causes, Symptoms and What To Do

14 Warning Signs of Low Magnesium Levels and What to Do About It (Science Based)
Proven Health Benefits of Beets and Fermented Beets (Science Based)
Putting this in the vase box not only helps protect the chrysanthemums but also makes the vase more delicious

How to preserve cilantro so it stays fresh, green, and fragrant for a whole month

3 Reasons Onions Might Upset Your Stomach

Vaseline Uses and Benefits for Skin, Lips and Hair | Petroleum Jelly Benefits

Beetroot Face Gel for Clear Skin – Rosy Cheeks & Pink Blushing Skin

How i use CUCUMBER for Skin & Eyes : Remove Dark Circles & Get Glowing Skin

Tips for removing grease from an air fryer
