
Garlic Supplementation and Metabolic Improvement in Non-Alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) is now one of the most common chronic liver conditions worldwide, closely linked to obesity, insulin resistance, and dyslipidemia. Although lifestyle modification remains the cornerstone of treatment, long-term adherence to diet and exercise programs is often difficult, and there are currently no universally approved pharmacological therapies specifically for NAFLD. As a result, considerable research interest has focused on food-derived interventions that may simultaneously improve liver fat, inflammation, and metabolic dysfunction. A 15-week randomized, placebo-controlled clinical trial investigating daily garlic supplementation provides important evidence in this regard.
In this controlled human study, adults diagnosed with NAFLD were randomly assigned to receive either 800 mg of garlic per day or a placebo for 15 weeks. Liver fat was assessed using imaging, while liver enzymes and metabolic markers were measured through blood tests. By the end of the intervention, approximately half of the participants in the garlic group showed clear improvement in fatty liver status, compared with a much smaller proportion in the placebo group. Importantly, this difference remained statistically significant even after adjusting for potential confounding factors such as body-weight change, total calorie intake, and physical activity. This indicates that the observed benefits were not simply due to weight loss or lifestyle changes, but rather to the biological effects of garlic itself.
Beyond improvements in liver fat, garlic supplementation was associated with significant reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST), two key markers of liver injury and inflammation. Elevated ALT and AST levels reflect hepatocellular stress and are commonly used to monitor NAFLD progression. The reduction of these enzymes suggests that garlic did not merely improve imaging findings, but also reduced underlying liver inflammation and cellular damage. This distinction is clinically important, as inflammation is a major driver of progression from simple fatty liver to non-alcoholic steatohepatitis (NASH) and fibrosis.
The trial also demonstrated that garlic exerted broad metabolic benefits. Participants receiving garlic experienced significant reductions in fasting blood glucose and HbA1c, indicating improved glycemic control and insulin sensitivity. In parallel, lipid profiles improved markedly, with decreases in total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides. These changes are particularly relevant for NAFLD patients, who face elevated risks of cardiovascular disease—the leading cause of mortality in this population. Notably, no serious adverse effects were reported during the study, supporting the safety and tolerability of garlic at the tested dose.
Taken together, these findings suggest that garlic acts on multiple interconnected pathways relevant to NAFLD. Rather than targeting liver fat alone, garlic appears to influence insulin signaling, lipid metabolism, and inflammatory processes simultaneously. This multi-system effect is consistent with known biological properties of garlic, including its sulfur-containing compounds, which have been shown in experimental studies to modulate oxidative stress, improve insulin sensitivity, and regulate lipid synthesis and breakdown. The ability to improve liver enzymes, glucose metabolism, and lipid profiles within a single intervention distinguishes garlic from many other dietary approaches that affect only one aspect of the disease.
It is important to emphasize that, while promising, these results do not imply that garlic is a cure for NAFLD. The study duration was relatively short, and long-term outcomes such as fibrosis progression or regression were not assessed. Moreover, garlic supplementation should be viewed as an adjunct to, rather than a replacement for, established lifestyle interventions. Nevertheless, the rigor of the study design strengthens confidence in the findings. As a randomized, placebo-controlled human trial, it provides higher-quality evidence than observational studies or animal experiments.
In conclusion, this 15-week randomized, placebo-controlled clinical trial demonstrates that daily supplementation with 800 mg of garlic can significantly improve fatty liver status, reduce liver injury markers, and enhance metabolic health in adults with NAFLD, independent of weight loss or lifestyle changes (randomized placebo-controlled clinical trial in adults with NAFLD). By simultaneously targeting liver fat accumulation, inflammation, glucose control, and lipid metabolism, garlic emerges as one of the few food-derived interventions shown to improve multiple NAFLD-related markers in a controlled human setting. These findings support further long-term studies to clarify garlic’s role as a safe, accessible adjunct therapy in the management of NAFLD.
News in the same category


Thymoquinone and Breast Cancer Cell Suppression: Evidence from Preclinical Research

Ginger Supplementation and Cardiovascular Inflammation: Evidence from a Double-Blind Randomized Clinical Trial
Antioxidant Supplementation and Thyroid Autoimmunity: Evidence from a Randomized Controlled Trial

Chios Mastic Gum as an Anti-Inflammatory Intervention in Crohn’s Disease and Vascular Inflammation
Potassium Deficiency – Causes, Symptoms and What To Do

14 Warning Signs of Low Magnesium Levels and What to Do About It (Science Based)
Proven Health Benefits of Beets and Fermented Beets (Science Based)

3 Reasons Onions Might Upset Your Stomach

MRI vs PET: Which Imaging Modality Better Detects Prostate Cancer Recurrence?
Hidden Spread of Pseudomonas aeruginosa From Lung to Gut in Hospitalized Patients
‘Tis the Season to Help People Avoid Holiday Heart Syndrome
Got a lump on your neck, back or behind your ear? This is what you need to know

What Your Skin Could Be Telling You About Hidden Health Issues
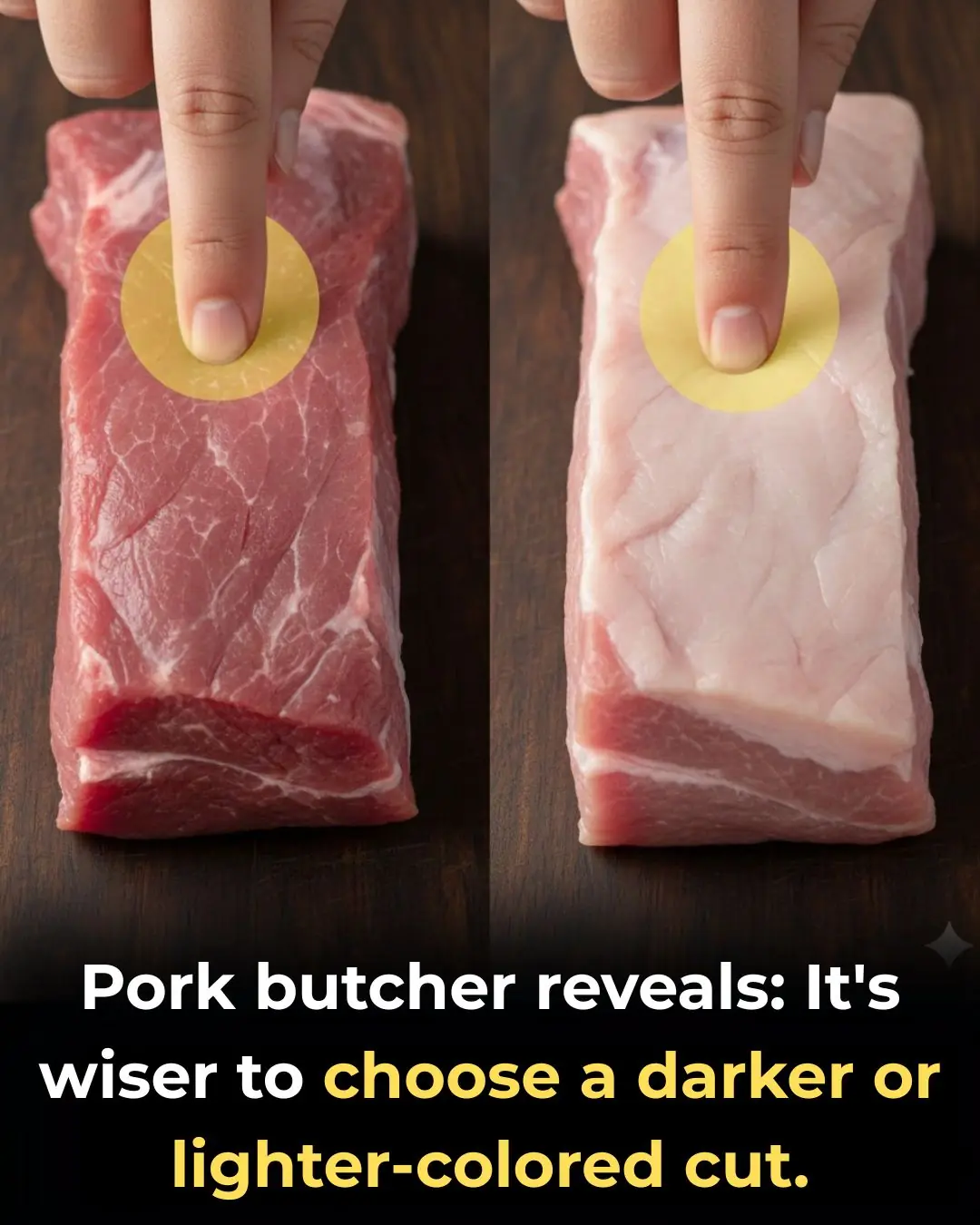
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?

4 Types of Vegetables Most Effective in Preventing Cancer, According to Doctors: Eating Them Regularly Is Great for Your Health
Stroke and Cerebral Infarction Prevention: Remember These 3 Indicators, 1 Disease, and 6 Key Habits

Optimism as a Psychosocial Predictor of Exceptional Longevity

Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health
News Post

Bee Propolis and Infertility in Endometriosis: Evidence from a Pilot Randomized Clinical Trial

Thymoquinone and Breast Cancer Cell Suppression: Evidence from Preclinical Research

Ginger Supplementation and Cardiovascular Inflammation: Evidence from a Double-Blind Randomized Clinical Trial
Antioxidant Supplementation and Thyroid Autoimmunity: Evidence from a Randomized Controlled Trial

Chios Mastic Gum as an Anti-Inflammatory Intervention in Crohn’s Disease and Vascular Inflammation
If you drink cucumber water every morning, this is what happens to your body

I soaked my feet in apple cider vinegar. 15 mins later, this is what happened

I need this ‘Liquid Gold.’
Potassium Deficiency – Causes, Symptoms and What To Do

14 Warning Signs of Low Magnesium Levels and What to Do About It (Science Based)
Proven Health Benefits of Beets and Fermented Beets (Science Based)
Putting this in the vase box not only helps protect the chrysanthemums but also makes the vase more delicious

How to preserve cilantro so it stays fresh, green, and fragrant for a whole month

3 Reasons Onions Might Upset Your Stomach

Vaseline Uses and Benefits for Skin, Lips and Hair | Petroleum Jelly Benefits

Beetroot Face Gel for Clear Skin – Rosy Cheeks & Pink Blushing Skin

How i use CUCUMBER for Skin & Eyes : Remove Dark Circles & Get Glowing Skin

Tips for removing grease from an air fryer
