MRI vs PET: Which Imaging Modality Better Detects Prostate Cancer Recurrence?
Detecting recurrent prostate cancer after definitive treatment remains one of the most challenging aspects of prostate cancer management. For men who undergo radical prostatectomy, a rising prostate-specific antigen (PSA) level—known as biochemical failure or biochemical recurrence—often serves as the first indication that cancer has returned. However, identifying the precise location of recurrent disease is critical, as it directly influences treatment decisions and patient outcomes.
New evidence suggests that when it comes to detecting local recurrence after prostatectomy, multiparametric magnetic resonance imaging (mpMRI) may outperform prostate-specific membrane antigen (PSMA) PET-CT, particularly at the prostate bed.
Understanding Biochemical Failure After Prostatectomy
Following radical prostatectomy, PSA levels should drop to undetectable levels. Any subsequent rise in PSA is considered biochemical recurrence and raises concern for residual or recurrent disease. This recurrence may be:
-
Local, occurring in the prostate bed
-
Regional, involving pelvic lymph nodes
-
Distant, such as bone or visceral metastases
Accurately determining the site of recurrence is essential, as localized disease may be amenable to salvage radiation therapy, while more widespread disease often requires systemic treatment.
Imaging Options for Restaging Prostate Cancer
Two advanced imaging modalities are commonly used to restage patients with biochemical recurrence:
Multiparametric MRI (mpMRI)
mpMRI combines anatomical and functional imaging sequences—including T2-weighted imaging, diffusion-weighted imaging, and dynamic contrast enhancement—to provide high-resolution visualization of soft tissue. It is particularly well suited for detecting subtle changes in the prostate bed following surgery.
PSMA PET-CT
PSMA PET-CT uses radiotracers that bind to prostate-specific membrane antigen, a protein highly expressed on prostate cancer cells. This modality has transformed prostate cancer imaging by enabling highly sensitive detection of nodal and distant metastatic disease, even at low PSA levels.
Key Findings From Recent Research
In patients with biochemical failure after prostatectomy, approximately two thirds were found to have detectable local disease at restaging, underscoring how common localized recurrence is in this setting.
The study revealed striking differences in detection rates between imaging modalities:
-
Multiparametric MRI alone detected local recurrent lesions in more than one third of patients
-
PSMA PET-CT alone identified local disease in only 5.9% of patients
These findings indicate that while PSMA PET-CT excels at identifying metastatic spread, it may miss small or early local recurrences confined to the prostate bed.
Why mpMRI Performs Better for Local Recurrence
Several factors explain the superior performance of mpMRI in detecting local disease:
-
High spatial resolution allows for detailed visualization of the prostate bed and surrounding soft tissues
-
Functional imaging sequences help differentiate scar tissue from recurrent tumor
-
Sensitivity to small lesions that may not express enough PSMA to be detected by PET imaging
After prostatectomy, recurrent tumors may be small, infiltrative, and located near surgical margins, making them difficult to detect with molecular imaging alone.
Strengths and Limitations of PSMA PET-CT
Despite its lower sensitivity for local recurrence, PSMA PET-CT remains invaluable in other clinical scenarios. Its strengths include:
-
Superior detection of lymph node involvement
-
Early identification of bone and distant metastases
-
Whole-body imaging in a single study
However, limitations include reduced sensitivity for microscopic local disease and potential false negatives in tumors with low PSMA expression.
Complementary, Not Competing, Modalities
Rather than viewing mpMRI and PSMA PET-CT as competing technologies, the study highlights their complementary roles. Combining both modalities may offer the most comprehensive assessment of recurrent prostate cancer:
-
mpMRI excels at identifying local recurrence, guiding salvage radiation planning
-
PSMA PET-CT helps detect regional and distant disease, influencing systemic therapy decisions
Using both imaging techniques strategically can improve staging accuracy and personalize treatment.
Clinical Implications for Patient Care
The findings have important implications for clinicians managing patients with biochemical recurrence after prostatectomy:
-
mpMRI should be strongly considered when evaluating suspected local recurrence, even if PSMA PET-CT findings are negative
-
Negative PSMA PET-CT does not rule out treatable local disease
-
Accurate localization can enable earlier, targeted salvage therapy and potentially improve long-term outcomes
Looking Ahead
As imaging technology continues to evolve, optimizing the sequencing and combination of diagnostic tools will be essential. Ongoing research is exploring hybrid imaging approaches, such as PET-MRI, which may further enhance detection while reducing redundancy.
For now, the evidence suggests a clear message: when searching for prostate cancer recurrence after prostatectomy, multiparametric MRI remains a critical tool, particularly for identifying local disease that could otherwise go undetected.
Early and precise detection not only shapes treatment decisions—it may ultimately determine whether recurrence can be controlled or cured.
News in the same category
‘Tis the Season to Help People Avoid Holiday Heart Syndrome
Got a lump on your neck, back or behind your ear? This is what you need to know

What Your Skin Could Be Telling You About Hidden Health Issues
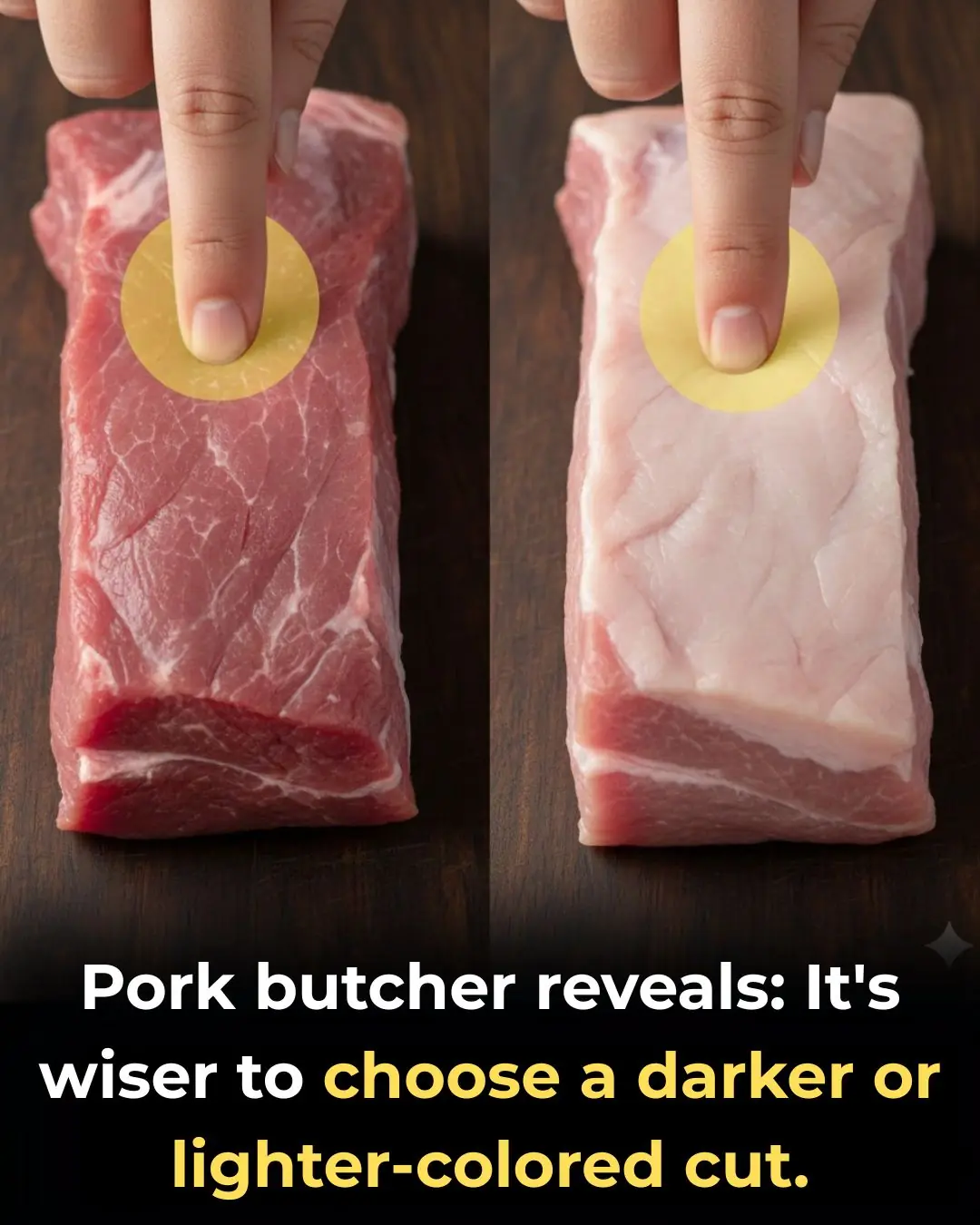
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?

4 Types of Vegetables Most Effective in Preventing Cancer, According to Doctors: Eating Them Regularly Is Great for Your Health
Stroke and Cerebral Infarction Prevention: Remember These 3 Indicators, 1 Disease, and 6 Key Habits

Optimism as a Psychosocial Predictor of Exceptional Longevity

Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health

Mebendazole as a Repurposed Therapy for Glioblastoma: Evidence from Preclinical Research
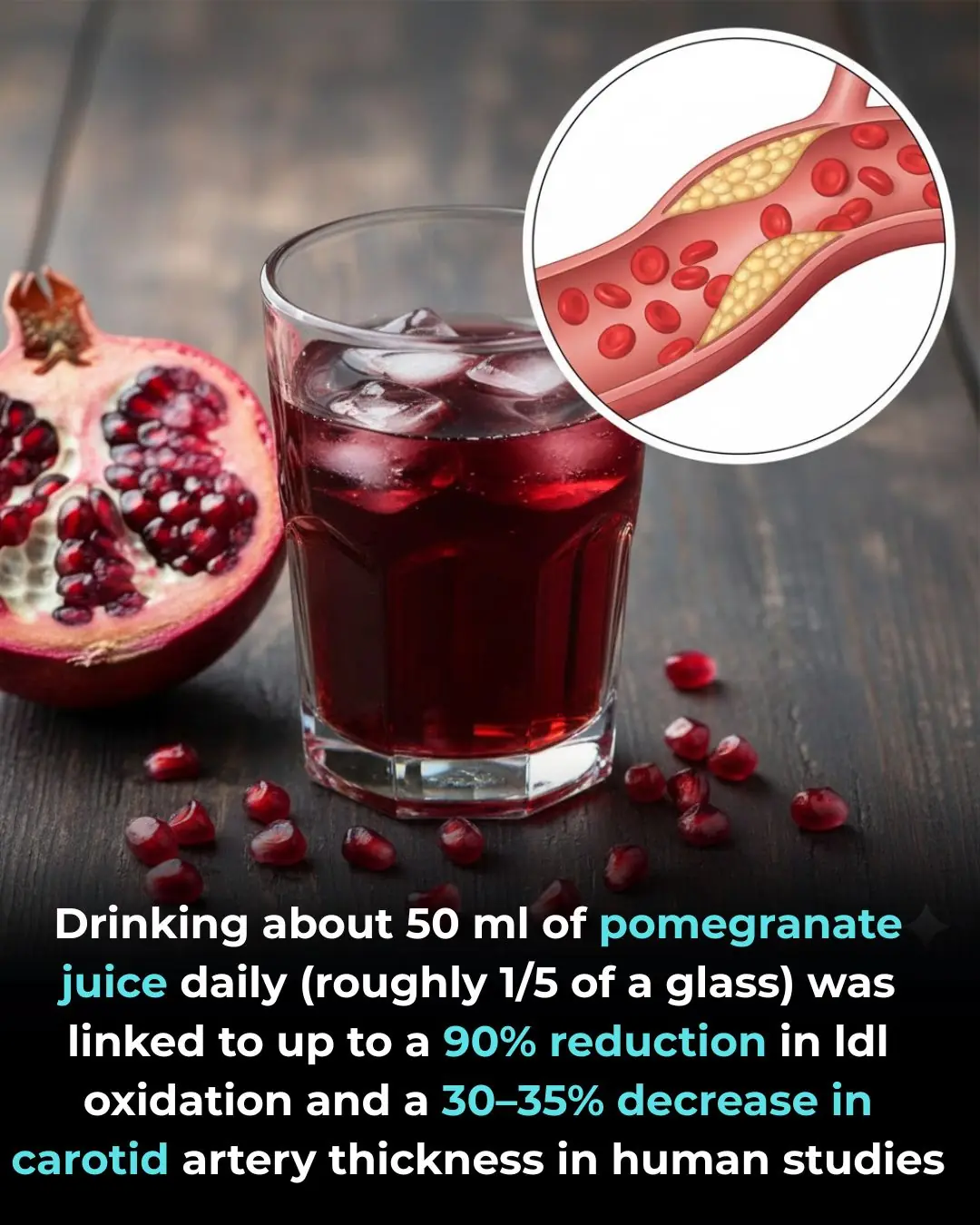
Pomegranate Juice and Cardiovascular Protection: Evidence from Human Clinical Studies

Synergistic Tumor Suppression by Vitamin K2 and Active Vitamin D in Triple-Negative Breast Cancer Cells

Thiamine Tetrahydrofurfuryl Disulfide (TTFD) as a Potential Supportive Intervention in Autism: Evidence from a Pilot Study
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail
How do people who take naps and those who don't? Experts reveal surprising truth
News Post

Tips for removing grease from an air fryer

There’s a warm spot on my hardwood floor even though the heat isn’t running under there, and no technician can come soon. What could cause that?

Eating these 5 fruits will help you avoid magnesium deficiency, keeping your heart healthy and your bones strong
I found little white crystals growing on the pipes in my basement, and I can’t get anyone to inspect it right now. What is happening?

Chop this fruit into small pieces and add it to the pot: Boiling duck will remove the gamey smell and make the meat five times softer and sweeter.

Don't put the scallions straight into the refrigerator after buying them; follow this method, and they'll last for a whole month without spoiling.

Should you tie your hair up or leave it down while sleeping to avoid hair loss
Marinating meat with just fish sauce and sugar isn't enough: Add this ingredient to make the meat melt in your mouth, just like in a 5-star restaurant.
Hidden Spread of Pseudomonas aeruginosa From Lung to Gut in Hospitalized Patients
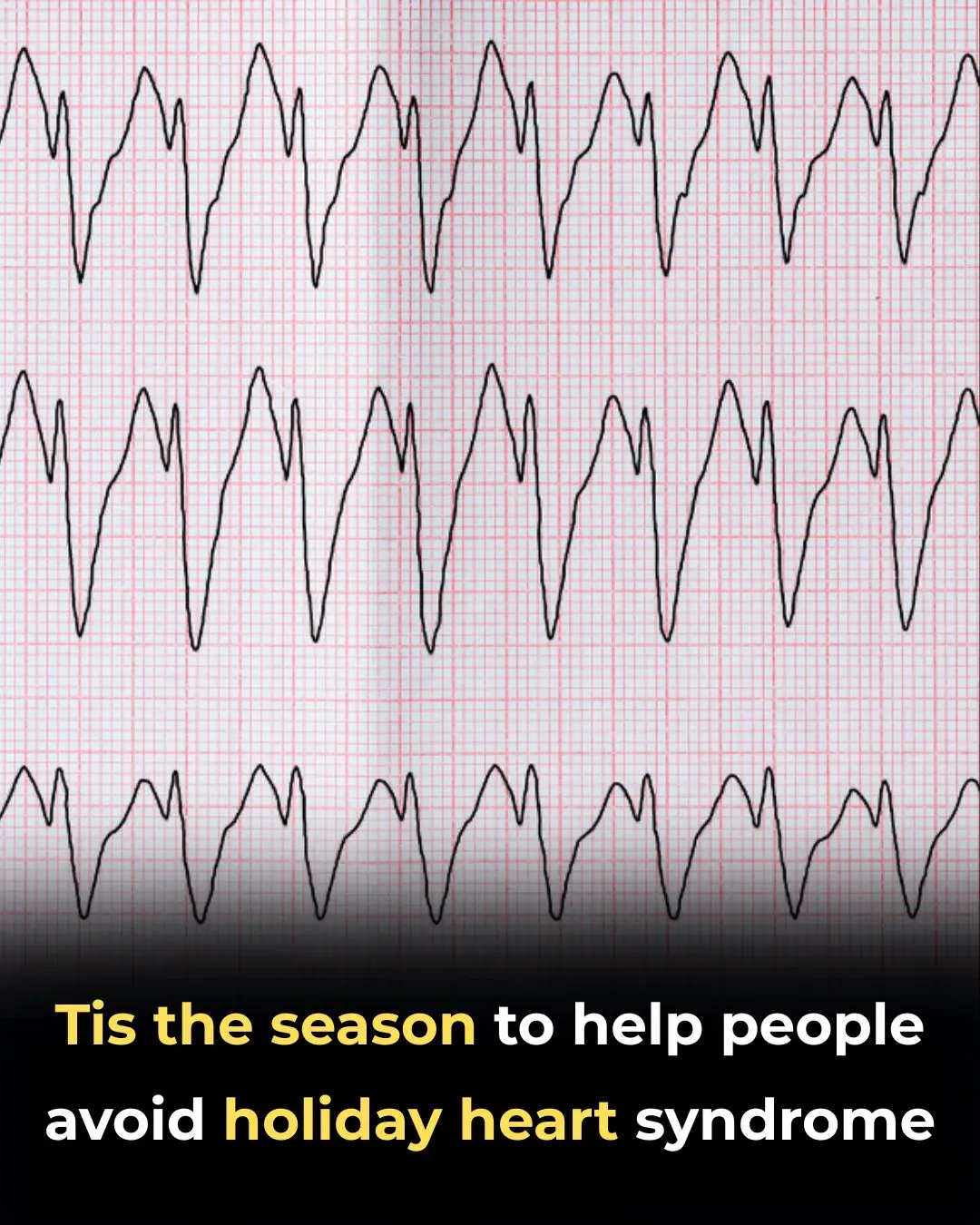
‘Tis the Season to Help People Avoid Holiday Heart Syndrome
Got a lump on your neck, back or behind your ear? This is what you need to know

What Your Skin Could Be Telling You About Hidden Health Issues
We have always wasted electricity without knowing it

Mop the floor with this, and it will be sparkling clean like new.
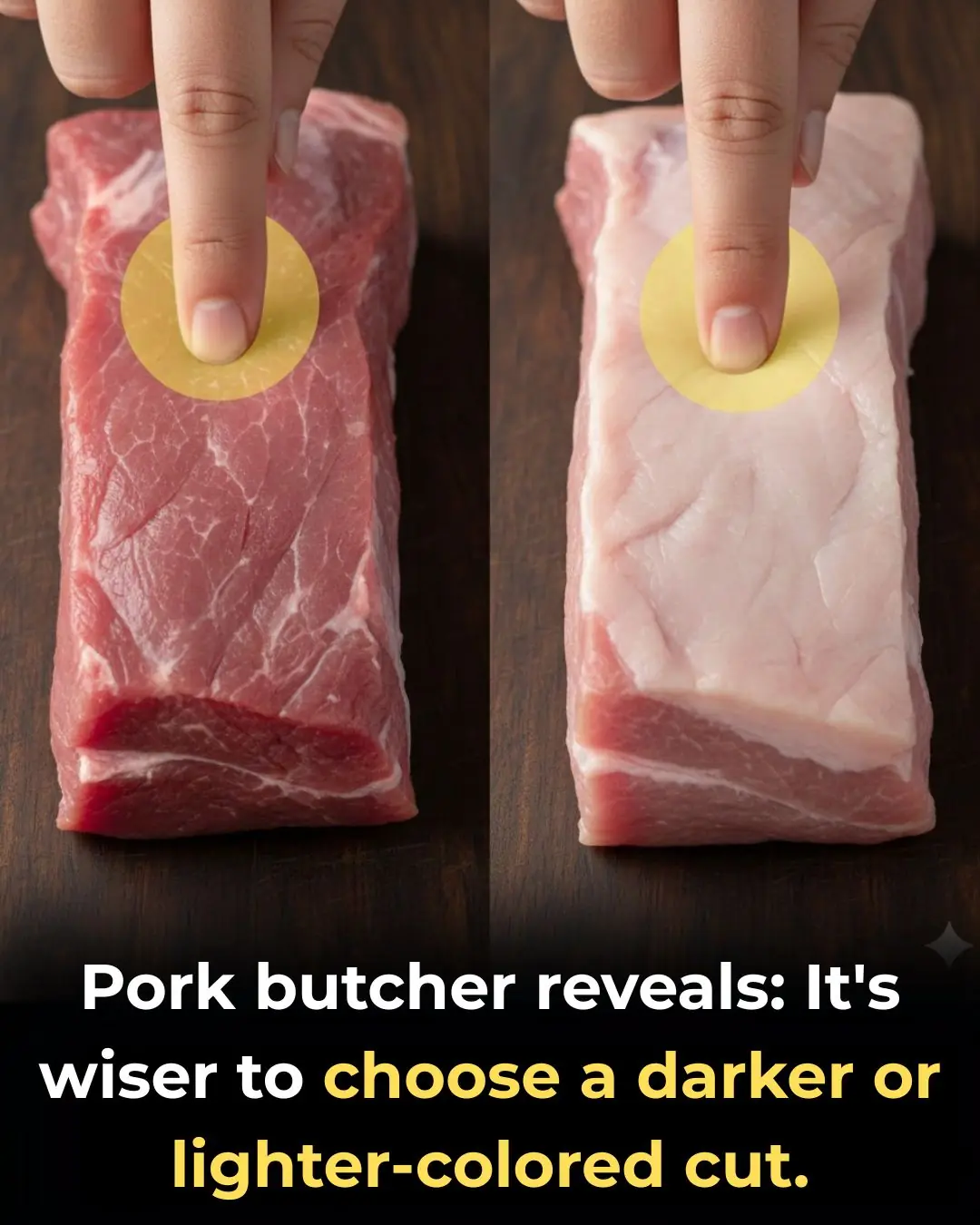
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?
How to Choose Fresh and Delicious Pork: Should You Pick Lighter or Darker Pieces?

DURING A FAMILY DINNER AT MY DAUGHTER’S HOUSE, I FELT SICK AND WENT TO THE KITCHEN TO DRINK SOME WATER. WHAT I SAW IN HER KITCHEN MADE ME… CALL 911!

After My Grandfather Died, I Was Given the Key to His Hidden Attic Compartment – When I Opened It, I Learned He Had Lied to Me My Whole Life

I came home unannounced from a vacation in the U.S. and froze when I saw my daughter lying in a hospital special care unit, while my son-in-law was posting photos of himself relaxing on a luxury yacht with another woman
