Cannabis Hyperemesis Syndrome: Why Emergency Department Visits Surged During the Pandemic
Over the past decade, cannabis use has become increasingly widespread, driven by legalization, changing social attitudes, and perceptions of safety. However, alongside these shifts, a lesser-known but serious condition has emerged more prominently in hospitals: Cannabinoid Hyperemesis Syndrome (CHS).
Recent data reveal a striking rise in emergency department (ED) visits related to this condition. Between 2016 and 2022, ED visits for CHS increased from 4.36 to 22.33 per 100,000 visits, with an alarming peak of 33.06 during the COVID-19 pandemic. This surge highlights a growing public health issue that many cannabis users — and even healthcare providers — still underestimate.
What Is Cannabinoid Hyperemesis Syndrome (CHS)?
Cannabinoid Hyperemesis Syndrome is a condition characterized by recurrent episodes of severe nausea, vomiting, and abdominal pain in individuals who use cannabis regularly, often daily or multiple times per week over long periods.
Ironically, cannabis is widely known for its anti-nausea properties. Yet in some chronic users, prolonged exposure to cannabinoids appears to disrupt the body’s normal regulation of the gastrointestinal system, leading to persistent and debilitating symptoms.
Common symptoms include:
-
Intense, uncontrollable vomiting
-
Persistent nausea
-
Abdominal pain or cramping
-
Dehydration and electrolyte imbalances
-
Temporary relief from hot showers or baths, a hallmark sign of CHS
Because these symptoms mimic other gastrointestinal disorders, CHS is frequently misdiagnosed, leading to repeated emergency visits and extensive testing.
Why Did ED Visits Increase So Dramatically?
1. Increased Cannabis Consumption
Between 2016 and 2022, cannabis use rose significantly, particularly in regions where recreational and medical marijuana became legal. The pandemic further accelerated this trend, as many people turned to cannabis to cope with stress, anxiety, boredom, and social isolation.
Higher frequency, higher potency products — including concentrates and edibles — increased overall cannabinoid exposure, raising the risk of CHS.
2. Pandemic-Related Stress and Behavior Changes
The COVID-19 pandemic created a perfect storm:
-
Lockdowns limited access to social support and healthcare
-
Mental health struggles intensified
-
Daily routines were disrupted
Many users reported increased frequency and dosage of cannabis during this period. The data reflect this change, with CHS-related ED visits peaking at 33.06 per 100,000 visits, far above pre-pandemic levels.
3. Greater Awareness and Improved Diagnosis
Another contributing factor may be improved recognition of CHS among emergency physicians. As medical literature expanded and awareness increased, clinicians became more likely to identify cannabis as the underlying cause of unexplained vomiting syndromes.
While this does not fully explain the magnitude of the rise, it likely contributed to more accurate reporting and coding of CHS cases.
The Burden on Emergency Departments
CHS places a significant strain on emergency healthcare systems. Patients often:
-
Require repeated ED visits
-
Undergo extensive imaging and laboratory testing
-
Need intravenous fluids, antiemetics, and pain management
Unfortunately, standard anti-nausea medications often provide little relief for CHS, leading to prolonged ED stays and frustration for both patients and providers.
The Only Proven Treatment: Cannabis Cessation
Despite various symptomatic treatments, the only definitive cure for CHS is stopping cannabis use entirely. Most patients experience symptom resolution within days to weeks after cessation, but relapse is common if cannabis use resumes.
This presents a major challenge, as many patients:
-
Do not believe cannabis is causing their symptoms
-
Use cannabis for anxiety, pain, or sleep
-
Experience withdrawal symptoms when stopping
Effective treatment often requires education, counseling, and long-term behavioral support.
Public Health Implications
The dramatic rise in CHS-related ED visits underscores a critical need for:
-
Better public education about the risks of chronic cannabis use
-
Clear warnings alongside legalization efforts
-
Improved screening for cannabis use in patients with unexplained vomiting
As cannabis becomes more accessible, understanding its potential harms — not just its benefits — is essential.
Conclusion
The increase in emergency department visits for Cannabinoid Hyperemesis Syndrome from 4.36 to 22.33 per 100,000 visits, with a pandemic peak of 33.06, is not just a statistic — it reflects a growing and underrecognized health issue.
CHS challenges the widespread belief that cannabis is harmless and highlights the complex ways long-term use can affect the body. As legalization and use continue to expand, awareness, early diagnosis, and prevention will be crucial to reducing unnecessary suffering and strain on healthcare systems.
News in the same category
Viral Infections Can Triple the Risk of Heart Attack and Stroke
Australian HPV Vaccination Marks Cervical Cancer Milestone

Vitamin K2 Supplementation and Vascular Health in Chronic Kidney Disease

Daily Prune Consumption and Bone Health in Postmenopausal Women
Montmorency Tart Cherry Juice as an Adjunctive Therapy in Ulcerative Colitis

Methylene Blue–Based Photodynamic Therapy as a Selective Strategy Against Breast Cancer Cells
Regenerating True Articular Cartilage: A Breakthrough in Joint Repair

Deuterium-Depleted Water and Long-Term Survival in Cancer Patients: Evidence from a Hungarian Population-Based Analysis

Daily cocoa extract supplements lowered cardiovascular disease deaths by 27%

Ivermectin stopped aggressive cancer cells from moving and spreading in lab tests
The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain
Quickly Drain You Lymph System Using Theses Simple Techniques to Boost Immunity and Remove Toxins

The Top 20 Essential Oils to Relieve Pain and Inflammation (Research Based)
Headache Above or Behind the Left Eye: Causes and Treatments
Root Canals May Lower Risk of Heart Disease, Diabetes

Mother-to-Infant Microbiome Transmission: Beyond Bacteria to Genes

Vitamin C Supplementation and Its Targeted Impact on the Human Gut Microbiome
News Post

FDA Approves Steam-Based Device for Prostate Cancer Treatment, but Questions Remain
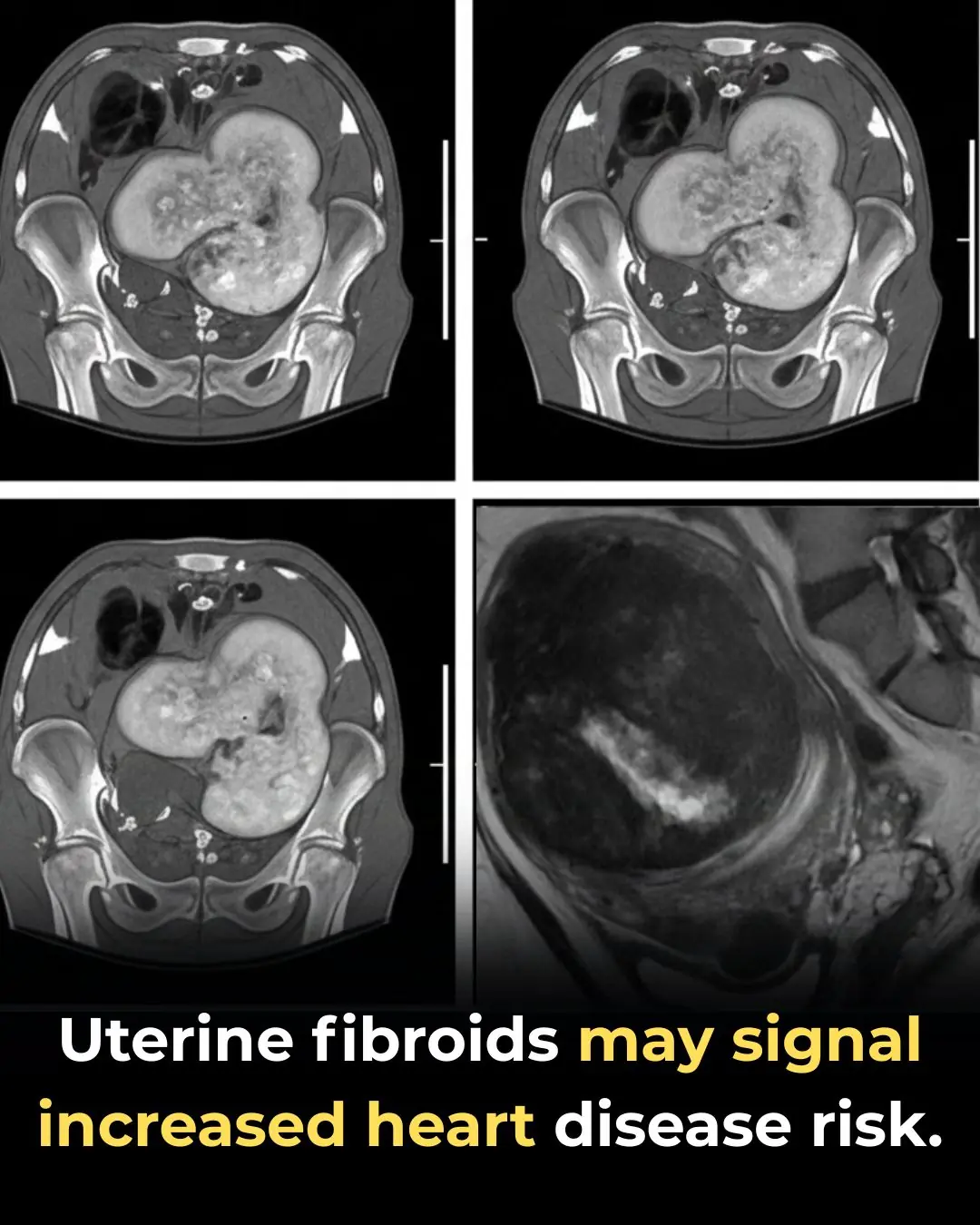
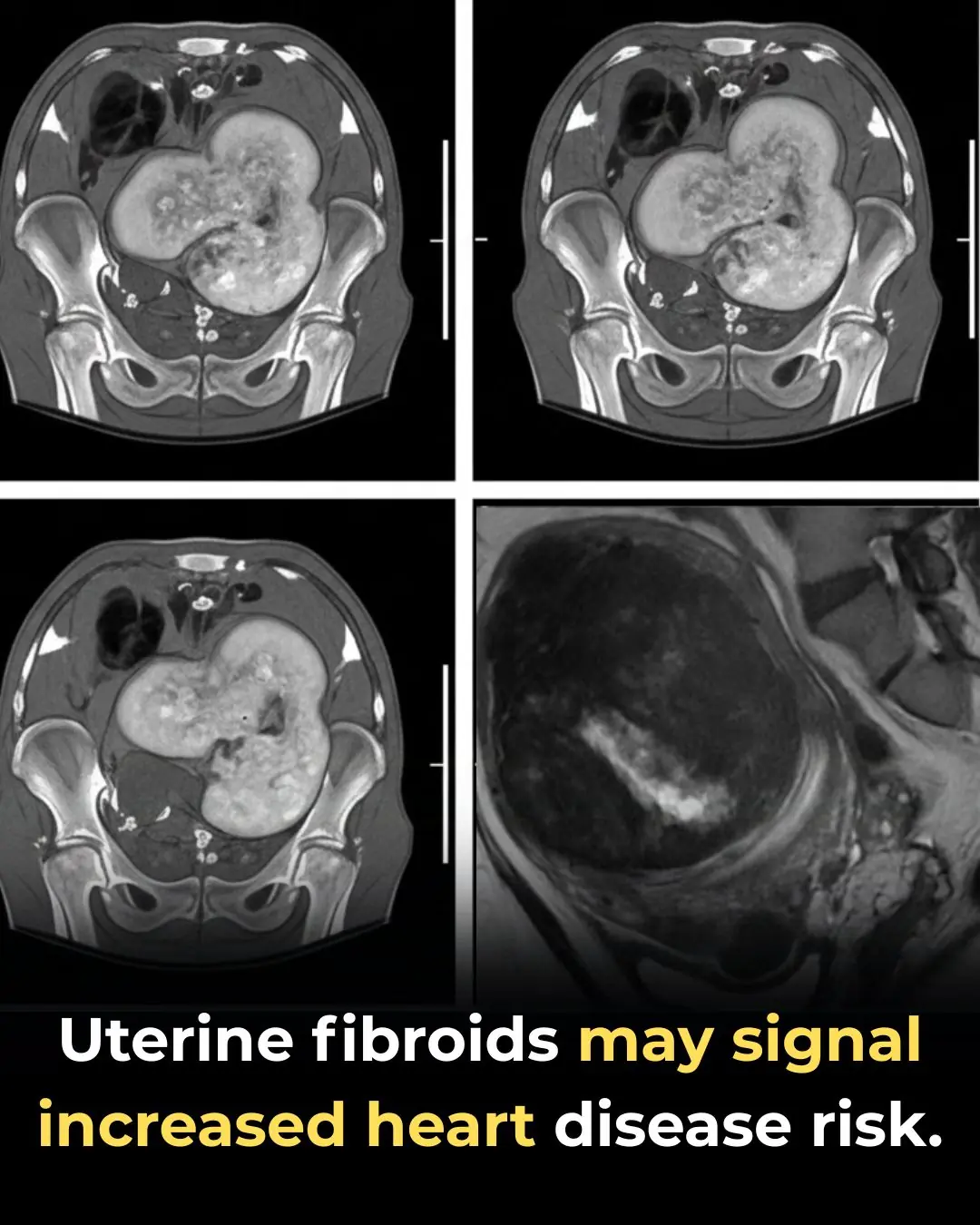
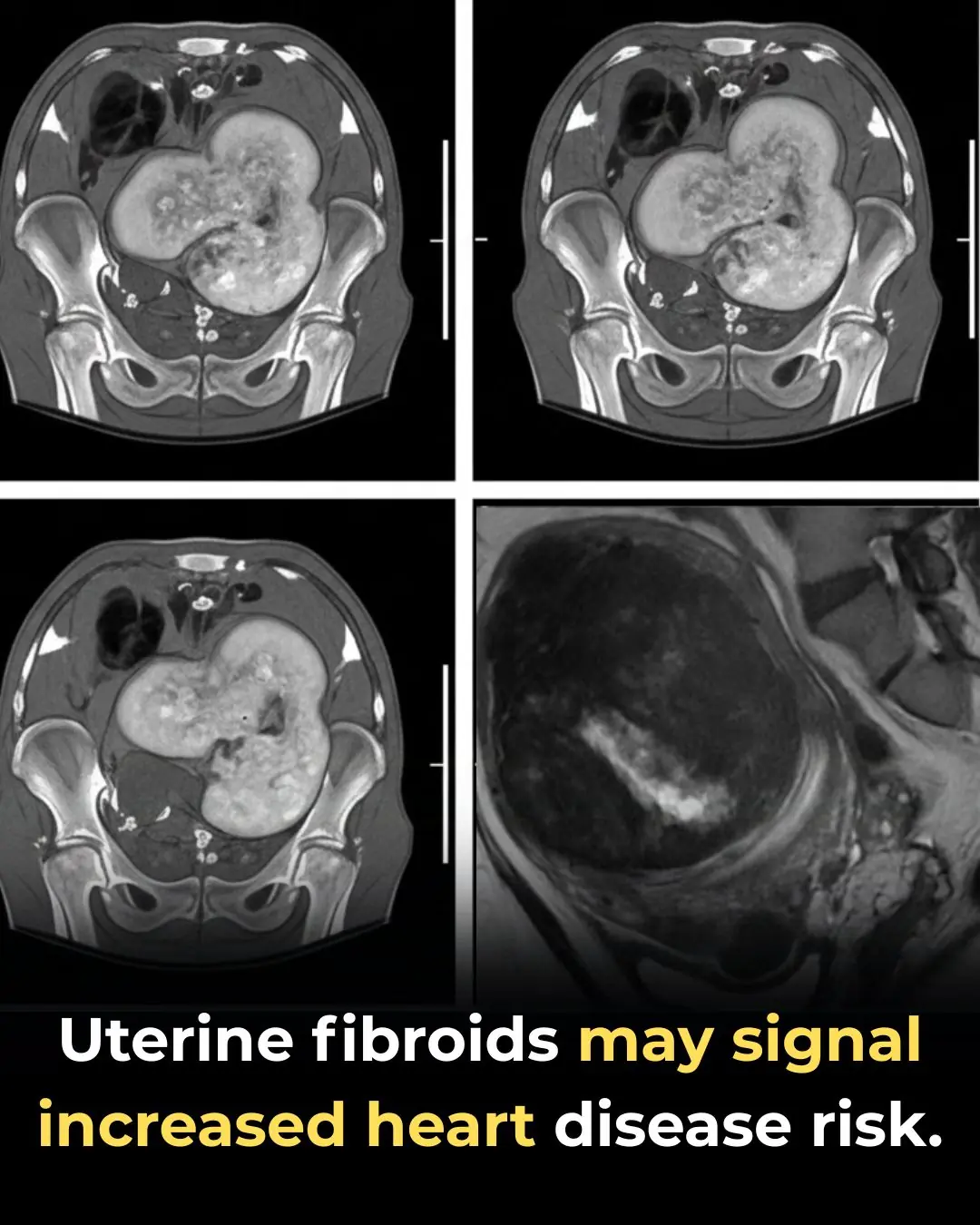
Uterine Fibroids May Signal Increased Risk of Heart Disease, New Research Suggests

The secret button on a computer with ‘magical’ functions that not everyone knows about
Viral Infections Can Triple the Risk of Heart Attack and Stroke
Australian HPV Vaccination Marks Cervical Cancer Milestone

My outdoor faucet suddenly froze and now I’m seeing water seeping indoors — what should I do before a plumber can come?

Vitamin K2 Supplementation and Vascular Health in Chronic Kidney Disease

Daily Prune Consumption and Bone Health in Postmenopausal Women
Montmorency Tart Cherry Juice as an Adjunctive Therapy in Ulcerative Colitis

Methylene Blue–Based Photodynamic Therapy as a Selective Strategy Against Breast Cancer Cells
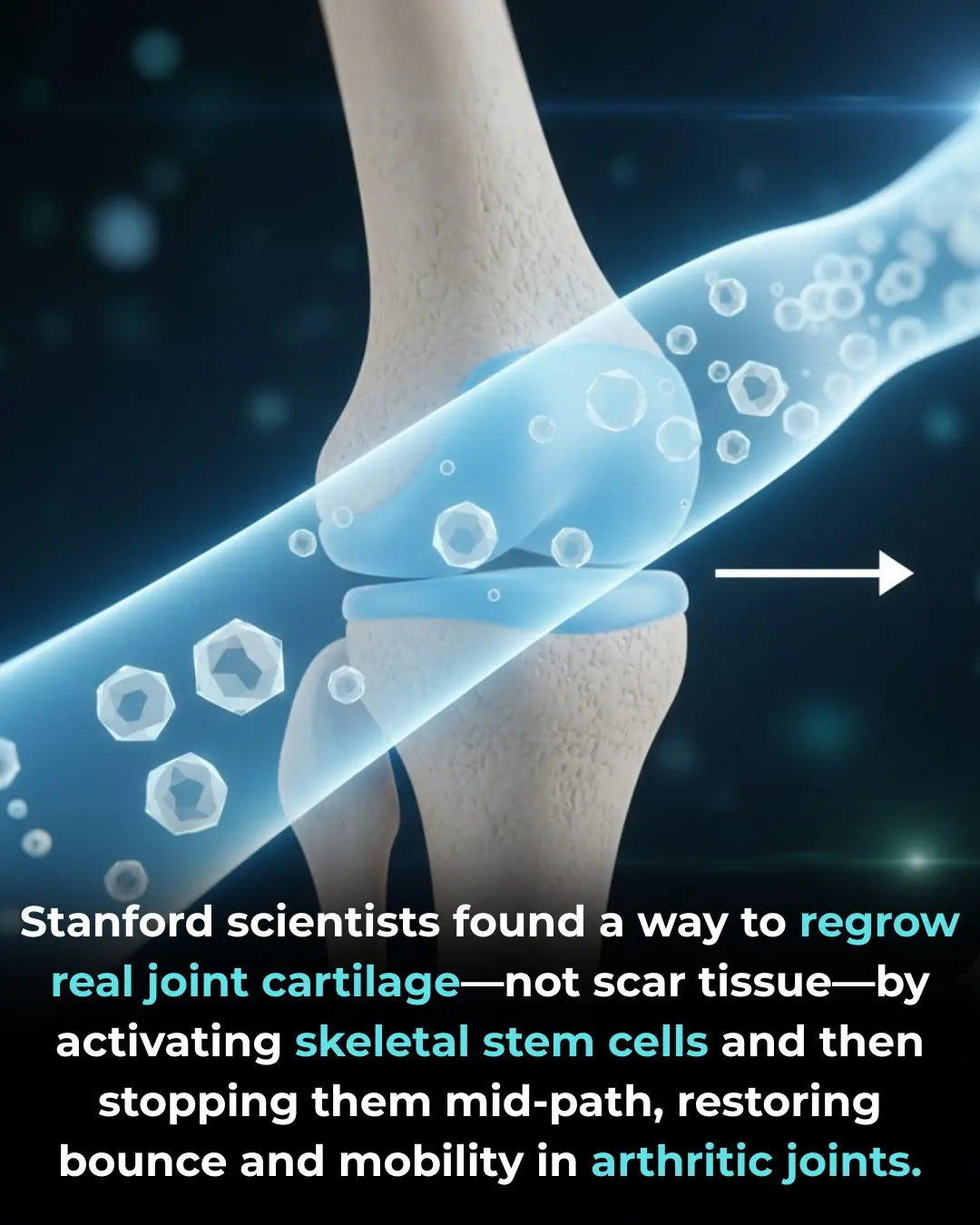
Regenerating True Articular Cartilage: A Breakthrough in Joint Repair

Deuterium-Depleted Water and Long-Term Survival in Cancer Patients: Evidence from a Hungarian Population-Based Analysis

Daily cocoa extract supplements lowered cardiovascular disease deaths by 27%

Ivermectin stopped aggressive cancer cells from moving and spreading in lab tests
These brown crusty spots keep showing up, and my doctor is booked for weeks given Christmas. Should I be concerned?
There’s this crusty little spot that keeps scabbing and reopening, and I can’t get in to see anyone yet. What could this be?

I had no clue about this

My fingertips keep splitting open in the cold, but I can’t get in to see the doctor anytime soon. What can I do now?