High-Dose Thiamine and Cancer Cell Metabolism: Evidence from Experimental Cell-Line Studies
High-Dose Thiamine and Cancer Cell Metabolism: Evidence from Experimental Cell-Line Studies
Cancer cell proliferation is closely linked to altered cellular metabolism. One of the most well-known metabolic features of cancer is the Warburg effect, in which tumor cells preferentially generate energy through aerobic glycolysis—converting glucose to lactate even in the presence of oxygen. This metabolic shift allows cancer cells to grow rapidly but also creates a potential therapeutic vulnerability. A 2014 experimental study titled “High Dose Vitamin B1 Reduces Proliferation in Cancer Cell Lines Analogous to Dichloroacetate”, published in Cancer Chemotherapy and Pharmacology, explored whether extremely high doses of thiamine (vitamin B1) could interfere with this metabolic advantage and suppress cancer cell growth.
In this study, researchers Hanberry, Berger, and Zastre investigated the effects of pharmacological doses of thiamine on two aggressive human cancer cell lines: neuroblastoma (SK-N-BE) and pancreatic cancer (Panc-1). These cancer types are known for rapid proliferation and poor clinical outcomes, making them relevant models for exploring novel metabolic interventions. The researchers exposed the cancer cells to very high concentrations of thiamine—far exceeding normal nutritional levels—and monitored changes in growth rate, metabolism, and cell survival.
The results demonstrated a marked reduction in cancer cell proliferation following high-dose thiamine treatment. Both neuroblastoma and pancreatic cancer cells showed significantly slower growth compared with untreated controls. Importantly, this growth suppression was not due to simple toxicity but was linked to a fundamental shift in cellular energy metabolism. The authors observed that high-dose thiamine altered how cancer cells processed glucose, directly targeting the metabolic pathways that support rapid tumor growth.
Mechanistically, the study focused on pyruvate dehydrogenase (PDH), a key mitochondrial enzyme that links glycolysis to oxidative phosphorylation. In many cancer cells, PDH activity is suppressed, diverting pyruvate away from the mitochondria and toward lactate production. This supports the glycolytic phenotype characteristic of the Warburg effect. High-dose thiamine was found to reactivate PDH, effectively forcing cancer cells to shift back toward a more “normal,” oxygen-dependent energy pathway. As a result, treated cancer cells consumed less glucose, produced less lactate, and showed reduced reliance on glycolysis.
This metabolic reprogramming had significant downstream consequences. By restoring mitochondrial oxidative metabolism, high-dose thiamine increased metabolic stress within cancer cells and promoted apoptosis, or programmed cell death. The activation of apoptosis suggests that cancer cells were unable to adapt effectively to the forced metabolic shift, leading to self-destruction rather than continued proliferation. Notably, this mechanism closely resembles the action of dichloroacetate (DCA), a metabolic drug known to activate PDH and reverse the Warburg effect. The authors highlighted this similarity, proposing that thiamine, at sufficiently high doses, may function as a metabolic modulator analogous to DCA.
The implications of these findings are conceptually important. Rather than targeting DNA replication or cell division directly, high-dose thiamine interferes with cancer growth by disrupting the metabolic foundation that tumors rely on. This strategy may be particularly valuable for cancers that are resistant to conventional chemotherapy but remain dependent on altered energy metabolism. However, the authors were careful to emphasize the limitations of their work. The experiments were conducted entirely in vitro, using isolated cancer cell lines, and the thiamine concentrations required to achieve these effects were far above typical dietary or supplemental levels.
In conclusion, the 2014 study published in Cancer Chemotherapy and Pharmacology provides experimental evidence that extremely high-dose thiamine can suppress cancer cell growth by reactivating pyruvate dehydrogenase, reversing the Warburg metabolic phenotype, and promoting apoptosis (Cancer Chemotherapy and Pharmacology, 2014). While these findings do not support clinical use at present, they highlight cancer metabolism as a promising therapeutic target and suggest that thiamine, under specific conditions, may influence tumor biology in ways that warrant further investigation through animal studies and carefully controlled clinical trials.
News in the same category
Quercetin as an Exercise Mimetic: Enhancing Mitochondrial Biogenesis and Physical Performance

Dual “Don’t-Eat-Me” Signals: A New Paradigm in Cancer Immune Evasion
Cinnamon and Neuroprotection: Evidence for Anti-Alzheimer’s Mechanisms

How to Improve Blood Circulation Naturally (Research Based)
The Most Effective Ways to Naturally Get Rid of Clogged Ears
Get Rid of Throat Mucus Faster With These Home Treatments (Evidence Based)

The Most Likely Symptoms of a Gallbladder Problem (Don’t Ignore Them)
Why Hearing Running Water Makes You Suddenly Need to Pee
The strange phenomenon of sleep paralysis: When the body stops listening

Surprising Health Benefits of Purslane (Portulaca oleracea)
Ageratum Conyzoides: A Valuable Herb with Many Health Benefits
The man died of colorectal cancer, his family broke down in tears: "He ate healthily but liked to do three things."
Women Who Regularly Eat These 4 Foods Can Prevent Premature Graying, Keeping Hair Dark and Shiny Even at 60
The Root that Helps the Liver Detoxify and Effectively Reduce Inflammation

There’s this crusty little spot that keeps scabbing and reopening, and I can’t get in to see anyone yet. What could this be?

FDA Approves Steam-Based Device for Prostate Cancer Treatment, but Questions Remain
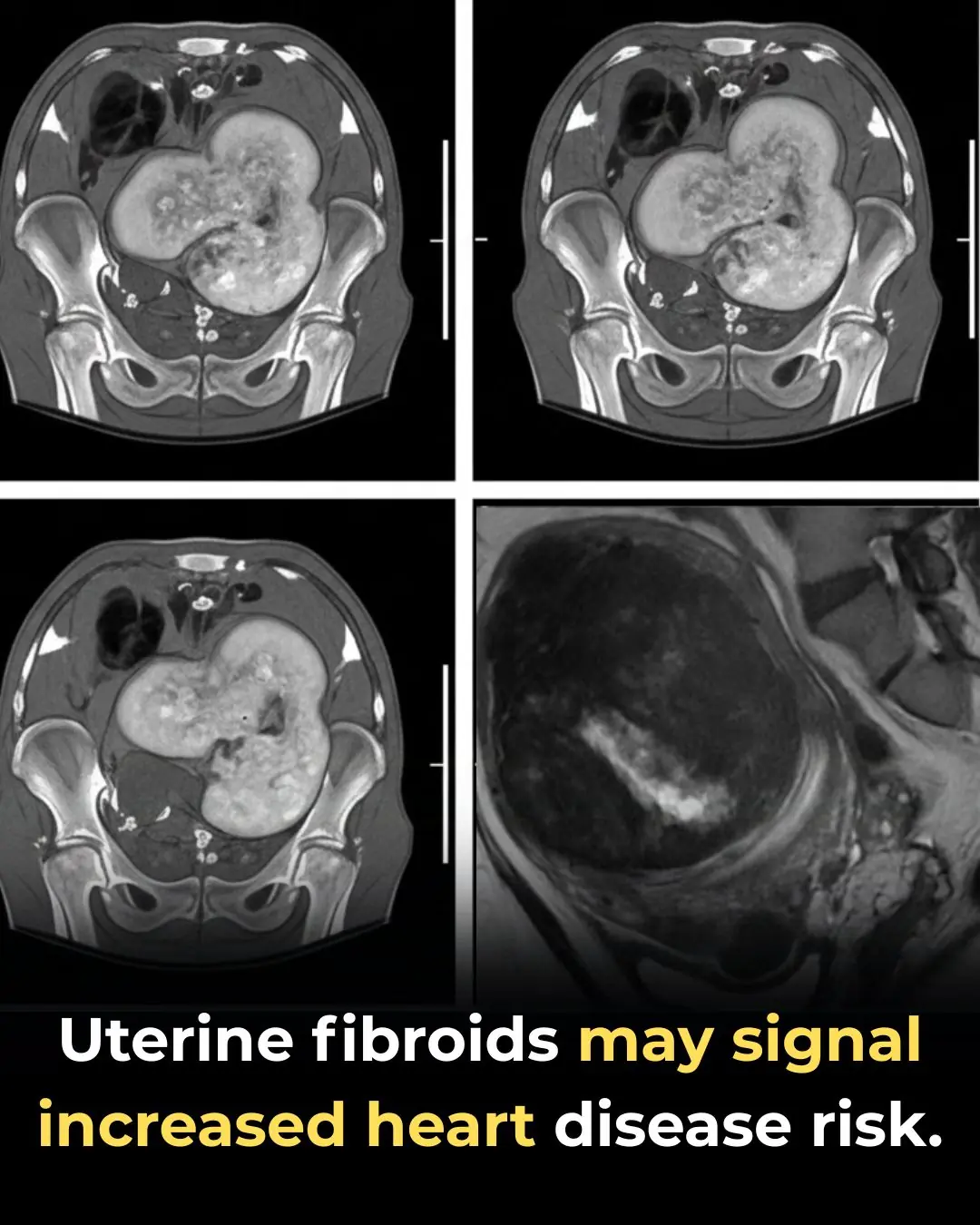
Uterine Fibroids May Signal Increased Risk of Heart Disease, New Research Suggests
Cannabis Hyperemesis Syndrome: Why Emergency Department Visits Surged During the Pandemic
News Post
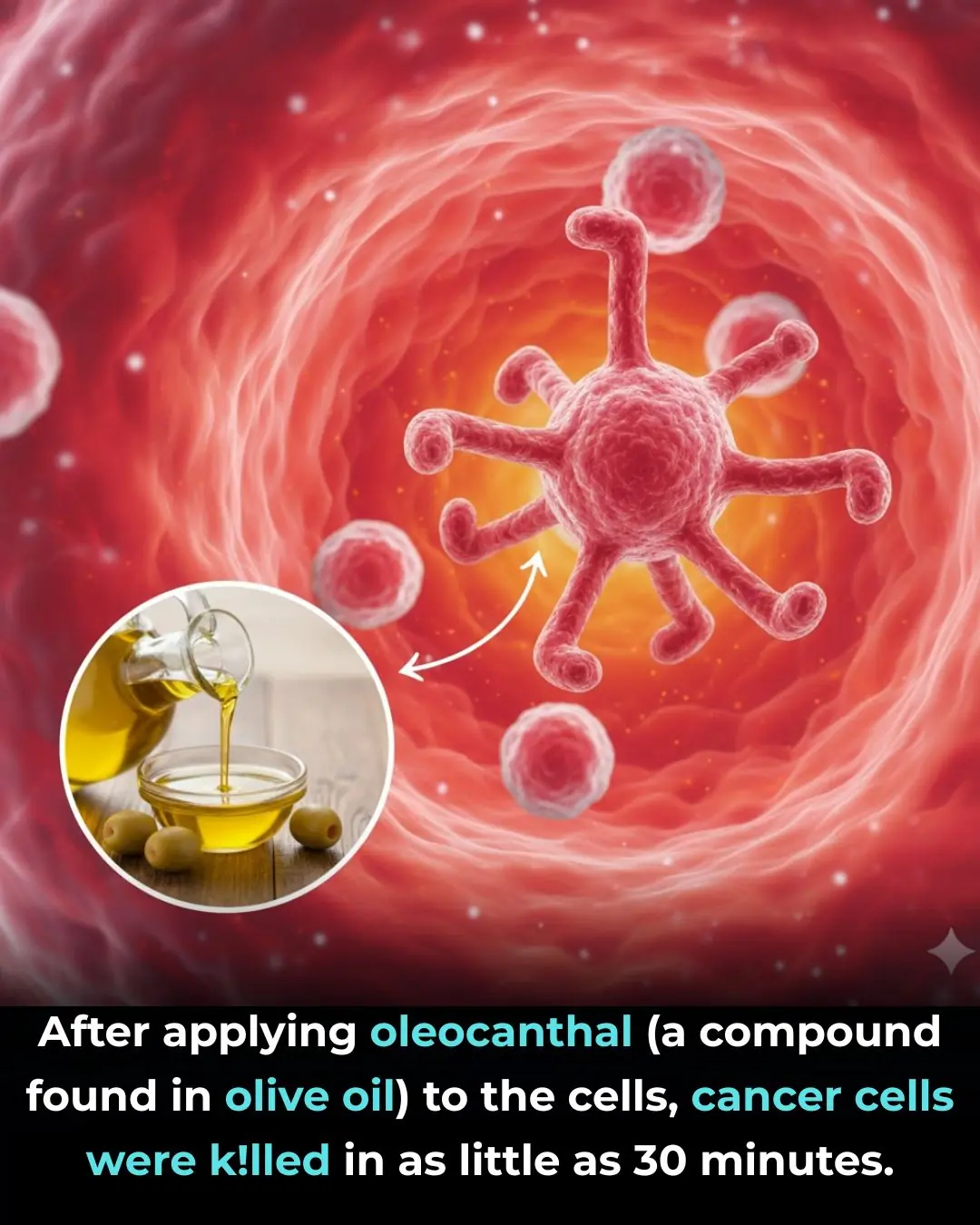
Oleocanthal from Extra-Virgin Olive Oil: A Multi-Targeted Anti-Inflammatory and Anti-Cancer Compound
Fenbendazole and Unexpected Cancer Remission: Insights from a 2024 Case Report
Quercetin as an Exercise Mimetic: Enhancing Mitochondrial Biogenesis and Physical Performance

Dual “Don’t-Eat-Me” Signals: A New Paradigm in Cancer Immune Evasion
Cinnamon and Neuroprotection: Evidence for Anti-Alzheimer’s Mechanisms
My heels are splitting open—no lotion helps. What else can I do? Should I see doc?
My aunt swears by this trick to reduce the look of thinning eyebrows that takes almost 0 work. Here's how it works

These purple veins appeared out of nowhere, and my doctor appointment is still weeks away. Should I worry?

Brown flat spots keep showing up on the back of my hands. Doctor appt is forever away. What should I do?

How to Improve Blood Circulation Naturally (Research Based)
The Most Effective Ways to Naturally Get Rid of Clogged Ears
Get Rid of Throat Mucus Faster With These Home Treatments (Evidence Based)

The Most Likely Symptoms of a Gallbladder Problem (Don’t Ignore Them)

If A Woman Says These 6 Things Regularly, She’s Way Smarter Than You Even Realize
11 Clever Phrases Smart People Use to End Pointless Arguments

Mopping the floor with this ingredient will make it sparkling clean, like new, and dust-free for a whole week.
Is it safe to eat rice that has been left in a rice cooker overnight
When thawing pork, do not soak it in water.