The Therapeutic Role of Glutamine in Post-Infectious Irritable Bowel Syndrome
Post-infectious irritable bowel syndrome with diarrhea predominance (PI-IBS-D) is a chronic gastrointestinal disorder that frequently develops after an episode of acute infectious gastroenteritis. It is characterized by persistent abdominal pain, frequent loose stools, impaired quality of life, and, in many patients, increased intestinal permeability. Current treatments often focus on symptom management rather than addressing underlying pathophysiological mechanisms. In this context, glutamine supplementation has emerged as a promising therapeutic strategy due to its central role in maintaining gut barrier integrity.
A randomized, double-blind, placebo-controlled clinical trial investigated the efficacy of oral glutamine supplementation in adults diagnosed with PI-IBS-D who exhibited increased intestinal permeability. Participants received 15 grams of glutamine per day for a duration of eight weeks. The results demonstrated a substantial clinical benefit, with a mean reduction of 120 points in the Irritable Bowel Syndrome Symptom Severity Score (IBS-SSS), corresponding to an approximate 40% improvement from baseline. Importantly, clinically significant symptom relief—defined as a reduction of at least 50 points—was achieved in 79.6% of patients receiving glutamine, compared with only 5.8% in the placebo group. This marked difference highlights the strong therapeutic effect of glutamine supplementation.
Beyond symptomatic improvement, the study provided evidence of a mechanism-based benefit through the restoration of gut barrier function. Intestinal permeability was assessed using the urinary lactulose-to-mannitol ratio, a well-established marker of epithelial integrity. In the glutamine-treated group, this ratio decreased by more than 50% from baseline and returned to normal levels, whereas no such improvement was observed in the placebo group. These findings suggest that glutamine directly supports intestinal epithelial repair and tight junction function, which are often compromised in PI-IBS-D.
Notably, improvements in clinical symptoms closely correlated with reductions in intestinal permeability. Patients who experienced normalization of gut barrier function also reported significant reductions in abdominal pain severity, stool frequency, and stool looseness, along with meaningful enhancements in overall quality of life. This relationship reinforces the concept that increased intestinal permeability is not merely an associated feature of PI-IBS-D but a key driver of symptom severity.
Safety and tolerability were also important outcomes of the trial. Approximately 96% of participants receiving glutamine experienced some degree of symptom improvement, while adverse events were minimal and no serious safety concerns were reported. This favorable safety profile is particularly relevant given the chronic nature of IBS and the need for long-term management strategies. Unlike many pharmacological treatments, glutamine represents a low-risk nutritional intervention that targets disease mechanisms rather than solely alleviating symptoms.
These findings are consistent with existing literature highlighting the role of glutamine as a primary fuel source for enterocytes and a critical regulator of intestinal barrier integrity (The American Journal of Clinical Nutrition). Furthermore, research on gut permeability and functional bowel disorders supports the therapeutic potential of interventions aimed at restoring epithelial function (Gut).
In conclusion, glutamine supplementation appears to be a highly effective and safe treatment for adults with PI-IBS-D and increased intestinal permeability. By addressing both symptoms and underlying gut barrier dysfunction, glutamine offers a mechanism-driven approach that may significantly improve patient outcomes and represents a valuable addition to current IBS management strategies.
News in the same category
Frequency-Specific Electromagnetic Fields and Cancer Cell Behavior: Evidence and Limitations

Saffron as a Potential Antidepressant: Evidence from Clinical Trials
Metabolic Effects and Limitations of an Extreme Single-Food Diet: Insights from a Sardine-Based Experiment
The Anti-Inflammatory Potential of Yogurt in Human Health
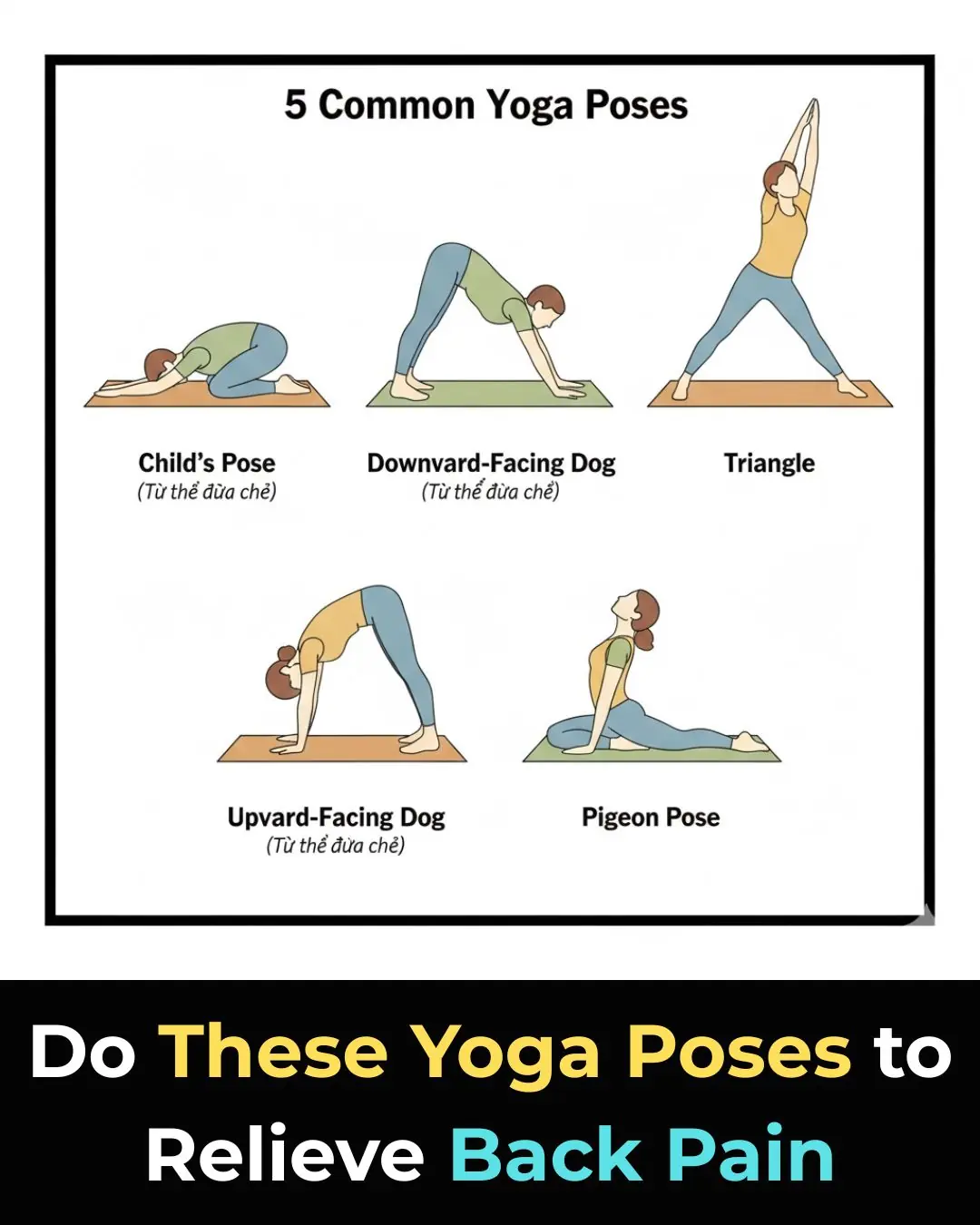
7 Yoga Poses That Can Help Relieve Lower Back Pain

How To Get Rid Of Eczema: 13 Natural Remedies Backed By Research

Scientists Explain The Effects of Eating Too Much Sugar
10 Simple Ways to Help Your Body Detoxify and Cleanse Itself

Why D-Dimer Testing Alone May Miss Pulmonary Embolism in Pregnancy

Don’t Soak Frozen Meat in Cold Water: A Chef’s 5-Minute Thawing Trick That Keeps Meat Tasty and Nutritious
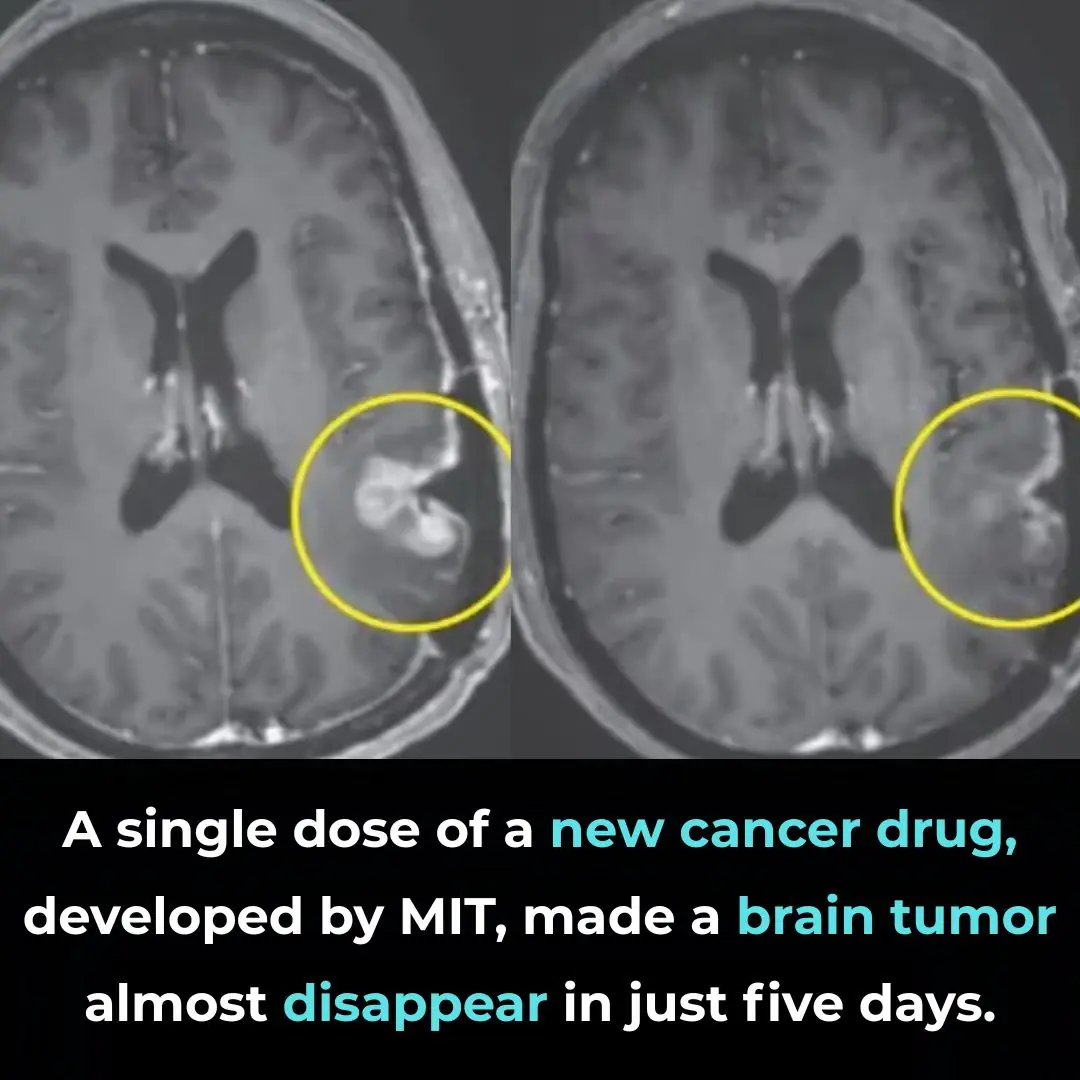
A Breakthrough in Glioblastoma Immunotherapy: Rapid Tumor Regression with CARv3-TEAM-E

Pomegranate Seed Oil Supplementation and Cognitive Improvement in Mild Cognitive Impairment

Selective Anti-Cancer Effects of Frankincense: Evidence from Laboratory Studies

Kimchi Consumption and Immune Balance: Evidence from a 12-Week Human Clinical Study
Selective Anti-Cancer Activity of Dandelion Root Extract in Colorectal Cancer
Inducing Lethal Autophagy in Glioblastoma Through Drug Repurposing

mRNA Flu Vaccines Show Higher Effectiveness Than Traditional Quadrivalent Shots, Phase 3 Trial Finds
Early Signs of Multiple Sclerosis
News Post
Yes, yes yes! This is what I've been looking for!
Periodontal Treatment as a Strategy for Cardiovascular and Cerebrovascular Protection
Frequency-Specific Electromagnetic Fields and Cancer Cell Behavior: Evidence and Limitations

Saffron as a Potential Antidepressant: Evidence from Clinical Trials
Metabolic Effects and Limitations of an Extreme Single-Food Diet: Insights from a Sardine-Based Experiment
The Anti-Inflammatory Potential of Yogurt in Human Health
Mixing white salt with fabric softener solves many household problems and saves money

Misconceptions that turn water purifiers into breeding grounds for germs – stop using them immediately or you could harm your whole family

Secrets to longevity after age 50: The 'golden' drink for lasting health.

The phone has a special button that helps detect hidden cameras in motels and hotels, a fact many people are unaware of

Chinese actress triumphs over stomach cancer for 25 years: Her secret is doing 3 things every day.

Rice water: A wonderful "treasure," don't throw it away! How to use it for effective and cost-saving health care.
When a married woman is attracted to another man, she does these 9 things
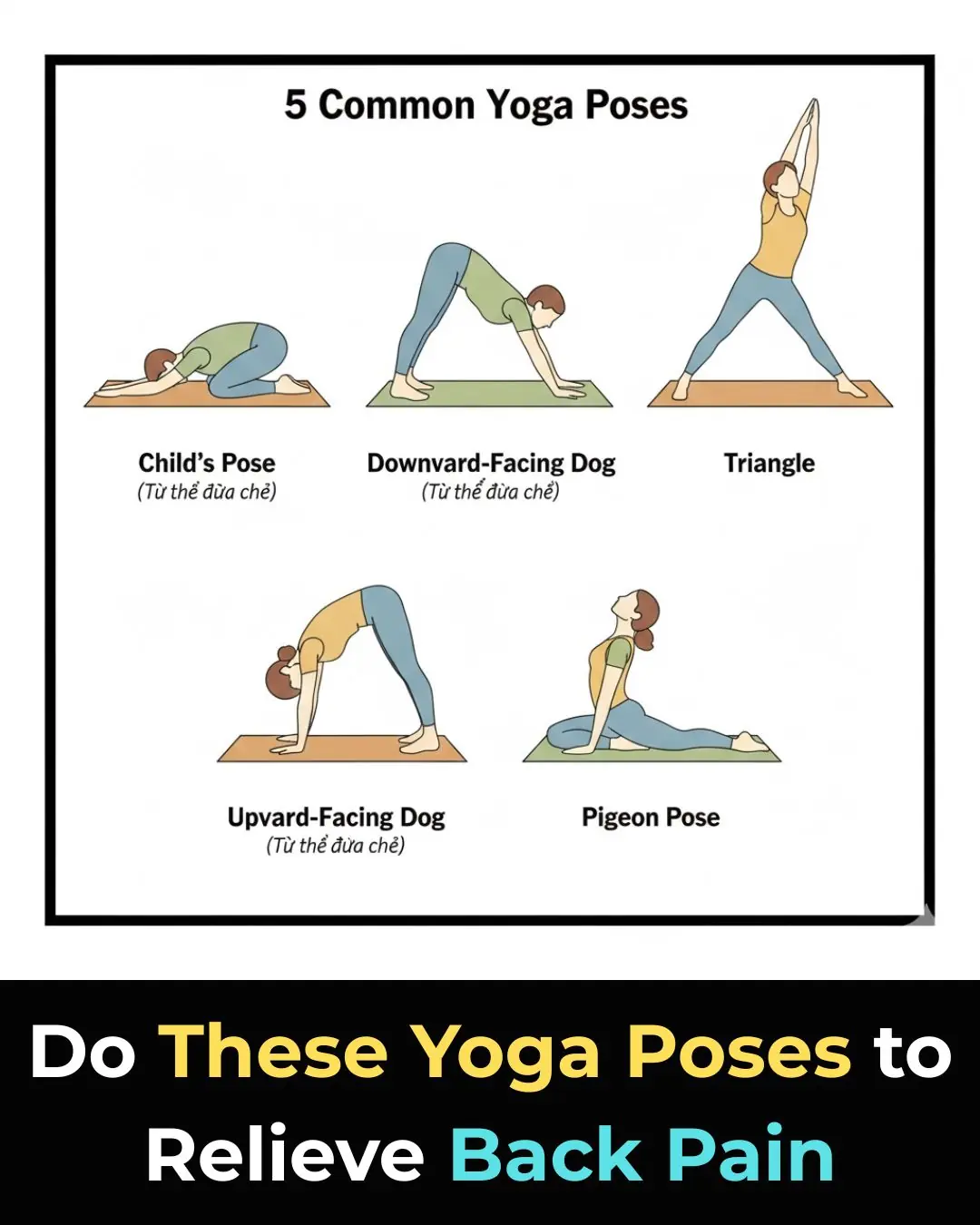
7 Yoga Poses That Can Help Relieve Lower Back Pain

Three holy water rituals many people practice at home before Christmas

Even old, non-stick pans can be "revived" with just a few simple tips that everyone should know
Eek, I might have a few of these!

Fry the fish with these two ingredients, and it will be crispy, fragrant, and won't stick to the pan.
