Understanding Phlegm: Why It Builds Up and How to Naturally Reduce It
Phlegm—commonly referred to as mucus—is something many people only pay attention to when they feel sick, congested, or short of breath. Yet mucus is not a sign of illness by default. In fact, it is a vital component of your body’s daily defense system. Every day, your respiratory tract produces mucus to trap dust, allergens, bacteria, and viruses before they can enter the lungs. Under healthy conditions, most people generate about 1 to 1.5 liters of mucus daily, which is usually swallowed unconsciously without causing discomfort.
Problems arise when mucus becomes unusually thick, excessive, or difficult to clear. When phlegm lingers in the throat or chest, it can cause coughing, throat irritation, chest tightness, and breathing discomfort. Understanding what phlegm is, why it builds up, and how to manage it naturally can make a significant difference in respiratory comfort and overall well-being.
What Is Phlegm, Exactly?
Phlegm is a thick, gel-like substance produced by the mucous membranes lining the nose, throat, sinuses, and lungs. Its primary purpose is protection. Phlegm is made up of several components, including:
-
Water, which keeps airways moist
-
Mucins, special proteins that give mucus its sticky texture
-
Immune cells such as neutrophils that fight infection
-
Antibodies like IgA that neutralize pathogens
-
Trapped particles such as dust, pollen, bacteria, and viruses
Mucus works alongside tiny hair-like structures called cilia, which continuously move in a coordinated motion to push mucus upward toward the throat. From there, it is either swallowed or expelled. This process helps keep the lungs clean and functioning efficiently.
Why Does Phlegm Build Up?

Phlegm production increases when the body is irritated, inflamed, or fighting off threats. Several common factors can cause mucus to thicken or accumulate:
1. Respiratory Infections
Colds, flu, sinus infections, and bronchitis stimulate the immune system to produce more mucus to trap and eliminate invading pathogens. Clear or white mucus is common in viral infections, while yellow or green mucus may appear when immune cells are actively fighting bacteria.
2. Allergies
Exposure to allergens such as pollen, mold, dust mites, or pet dander can trigger histamine release. This causes nasal swelling, increased mucus production, and postnasal drip.
3. Smoking
Tobacco smoke irritates the airways, damages cilia, and thickens mucus. As a result, phlegm becomes harder to clear, leading to chronic coughing and congestion, often referred to as a smoker’s cough.
4. Air Pollution and Chemical Irritants
Polluted air, strong cleaning agents, perfumes, and industrial chemicals can inflame the respiratory lining. The body responds by producing more mucus to protect itself.
5. Acid Reflux (GERD)
Stomach acid that travels up into the throat can irritate the airway lining, creating a constant sensation of mucus or postnasal drip, even without nasal congestion.
6. Dry Air
Low humidity dries out airway tissues, prompting the body to compensate by producing thicker mucus, which can feel sticky and difficult to expel.
7. Chronic Respiratory Conditions
Asthma, chronic obstructive pulmonary disease (COPD), and long-term sinus inflammation are often associated with ongoing mucus production and airway congestion.
Natural Ways to Reduce Phlegm and Clear Your Airways
Before relying on medication, many people find relief through simple, evidence-based home remedies that support the body’s natural clearing mechanisms.
1. Stay Well Hydrated
Adequate fluid intake is one of the most effective ways to thin mucus. When the body is dehydrated, mucus becomes dense and sticky, making it harder to clear.
Best options: warm water, herbal teas, ginger tea, chamomile tea, and clear broths
Limit: excess caffeine and sugary drinks, which may worsen dehydration
2. Gargle with Salt Water
Salt water can calm irritated throat tissues and reduce swelling through its natural osmotic effect.
How to use: Dissolve half a teaspoon of salt in warm water and gargle two to three times daily. This may also help reduce bacterial load in the throat.
3. Use Steam Inhalation
Inhaling warm, moist air helps loosen mucus and soothe irritated airways.
Tips:
-
Use a bowl of hot water or a warm shower
-
Optional: add eucalyptus or peppermint oil
-
Limit sessions to about 10 minutes to avoid irritation or burns
4. Apply a Warm Compress
Placing a warm compress on the chest or throat improves circulation and relaxes chest muscles.
Why it helps: Heat softens mucus and supports natural drainage, especially during chest congestion.
5. Honey and Lemon
Honey offers antibacterial and anti-inflammatory benefits, while lemon’s acidity and vitamin C content help break down mucus and support immune function.
How to use: Mix one tablespoon of honey with warm water or tea and add fresh lemon juice. This combination can also calm coughing and throat irritation.
6. Use a Humidifier
Maintaining proper humidity levels prevents airway dryness and reduces thick mucus formation.
Ideal humidity: 40–50%
Important: Clean humidifiers regularly to prevent mold and bacterial growth.
7. Try Nasal Irrigation
Saline rinses or neti pots help flush out allergens, pollutants, and excess mucus from the nasal passages.
Safety tips:
-
Always use sterile or distilled water
-
Rinse once or twice daily during congestion
8. Avoid Respiratory Irritants
Reducing exposure to irritants such as cigarette smoke, air pollution, strong fragrances, and chemical fumes allows inflamed airways to recover and produce less mucus.
Foods and Habits That May Make Phlegm Worse
Certain lifestyle factors can contribute to thicker or more noticeable mucus:
-
Smoking and secondhand smoke, which strongly stimulate mucus production
-
Excess sugar, which promotes inflammation
-
Overuse of nasal decongestant sprays, which can cause rebound congestion
-
Suppressing productive coughs, since coughing is a natural way to clear mucus
-
Dairy products (for some individuals), which may make mucus feel thicker, even if they do not increase production
When Should You See a Doctor?
Medical evaluation is recommended if:
-
Mucus persists longer than three weeks
-
Phlegm becomes yellow, green, brown, or bloody
-
You experience chest pain, fever, or shortness of breath
-
Symptoms worsen or do not improve with home care
Persistent or severe phlegm may indicate an underlying condition that requires medical treatment.
Conclusion
Phlegm is a normal and essential part of the body’s respiratory defense system. However, when mucus becomes thick, excessive, or long-lasting, it can interfere with breathing, sleep, and daily comfort. Simple lifestyle measures—such as staying hydrated, using steam, managing humidity, avoiding irritants, and supporting the immune system—can significantly reduce mucus buildup.
By recognizing your personal triggers and paying attention to warning signs, you can manage phlegm more effectively and know when professional medical care is necessary.
Disclaimer: This content is for informational purposes only and is not intended to replace professional medical advice. Always consult a qualified healthcare provider regarding your health concerns or medical conditions.
News in the same category
How Cancer Spreads Through The Lymphatic System (And How To Keep It Healthy)
This tasty recipe drops blood pressure by massive amounts naturally
The #1 enemy of your thyroid: stop eating this food immediately!

First Three Colors You See Reveals What’s Really Bothering You

Hotel Workers Reveal What Goes On
![Reduce Foot And Ankle Swelling [Top 9 Causes]](https://onplusnewscom.8cache.com/onplusnewscom/images/2025/12/13/1765633594jVo6Fro3lO.webp)
Reduce Foot And Ankle Swelling [Top 9 Causes]
5 early signs of poor circulation & how to boost blood flow

Foods to Eat When You’re Sick: Nutritional Support for Faster Recovery
Strange Body Symptoms Explained: What Your Body May Be Telling You

Understanding Magnesium: Types, Symptoms, and Scientific Support

Herbal Balms You Should Keep at Home: Traditional Uses and Scientific Perspectives
How to flush sugar out of your body fast
Bronchiectasis: Symptoms Most People Overlook
Respiratory Failure: Causes and Emergency Signs

The Hidden Power of Nutrition: 14 Overlooked Nutrients That Transform Health
Lung Infections: Common Types and How to Treat Them
Obsessive-Compulsive Disorder (OCD): Misunderstood Signs
Dizziness and Balance Problems: What They May Indicate
News Post
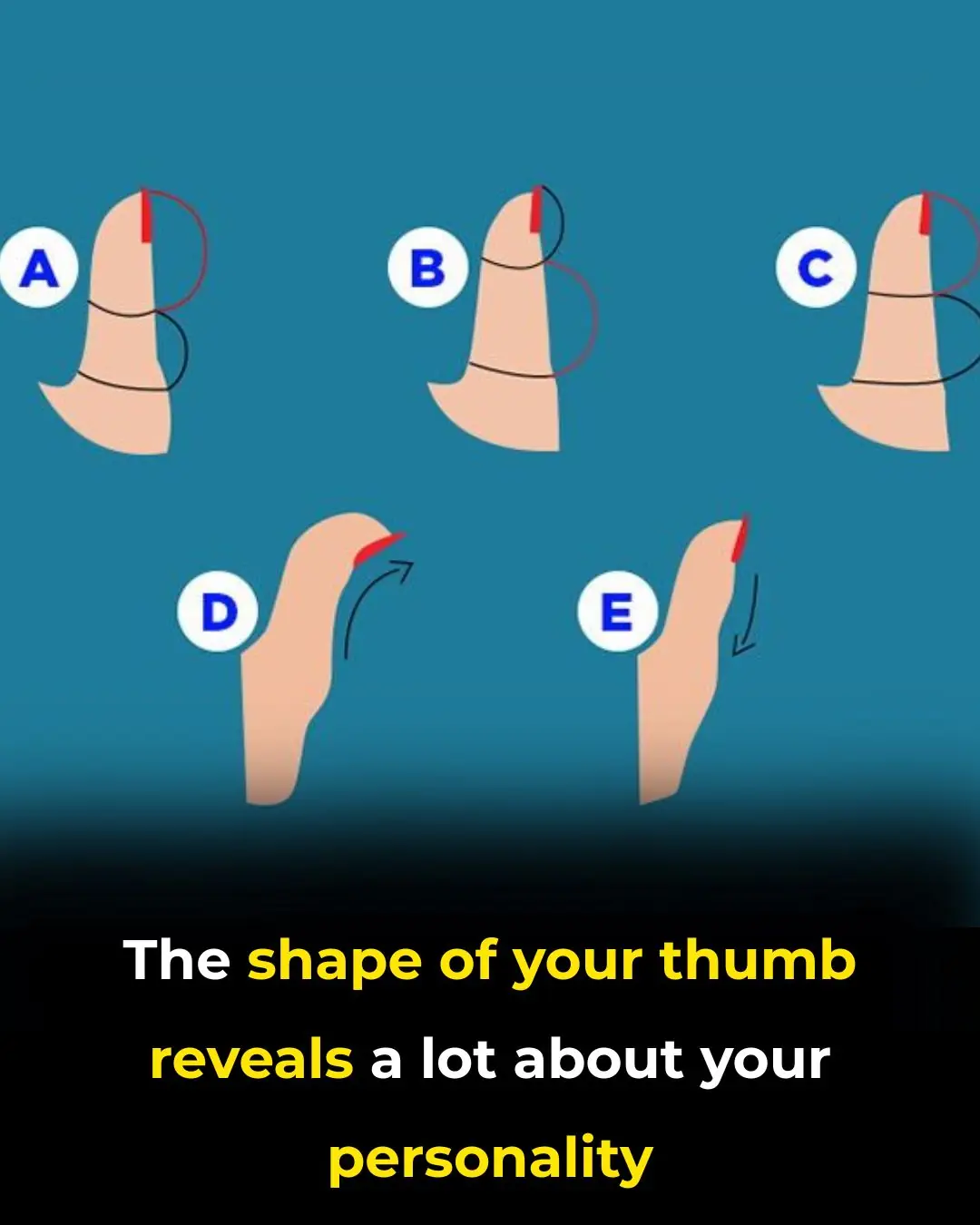
The Secrets Your Thumb Shape Reveals
5 Signs Your Lungs are Being Exposed to Mold
How Cancer Spreads Through The Lymphatic System (And How To Keep It Healthy)
This tasty recipe drops blood pressure by massive amounts naturally
The #1 enemy of your thyroid: stop eating this food immediately!

First Three Colors You See Reveals What’s Really Bothering You
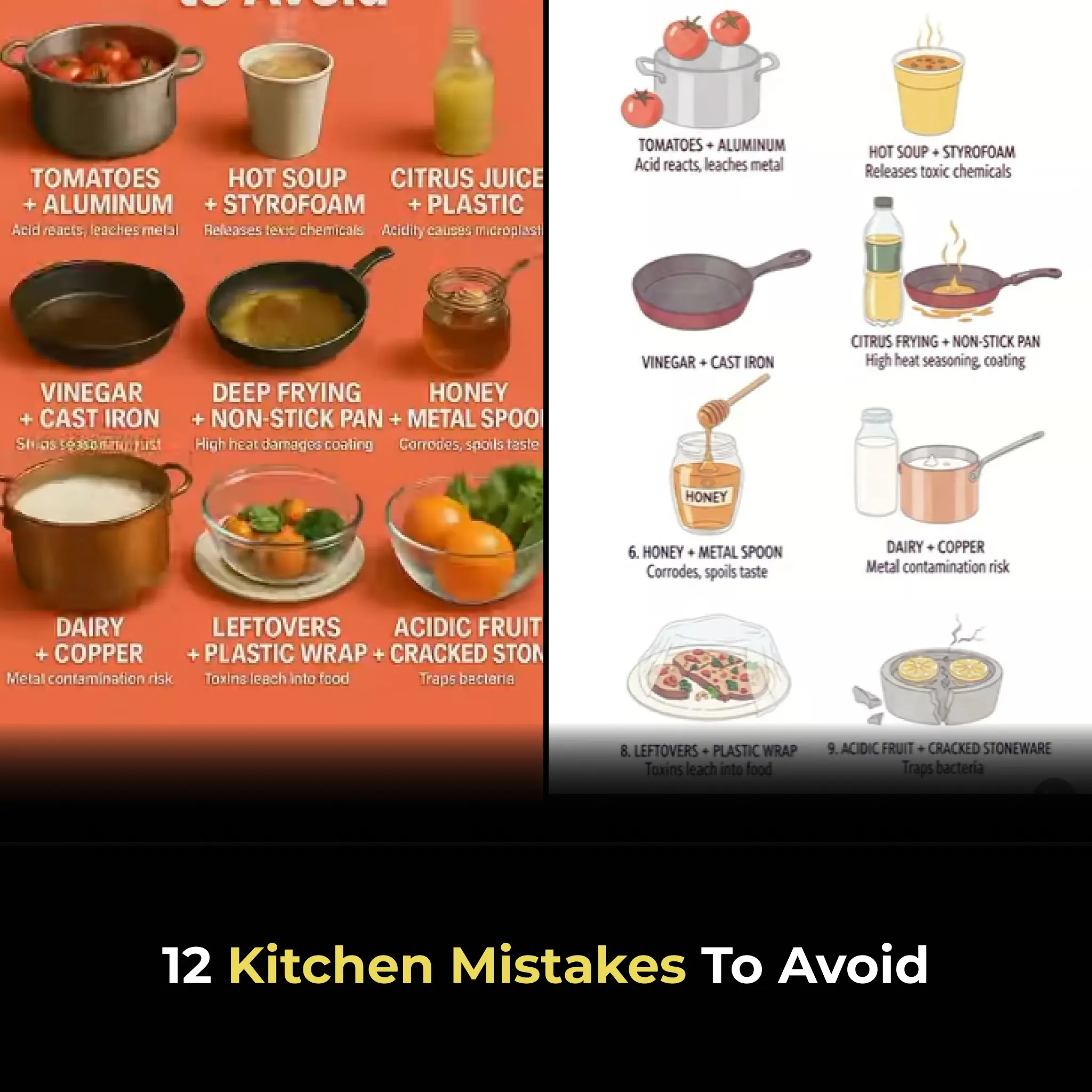
12 Kitchen Mistakes to Avoid

12 Herbal Balms You Should Keep at Home
Don’t Throw Away Rice Water

Say Goodbye to Swelling

Chew Just 4 Papaya Seeds a Day – The Tiny Habit Thousands Wish They Started Years Ago

The Overnight Remedy People Swear By for Cracked Heels!

15 Powerful Reasons You Should Drink Aloe Vera Juice: A Refreshing Boost for Your Health

Hotel Workers Reveal What Goes On
Norway’s Unique Approach to Raising Confident and Healthy Children: A Deep Connection with Nature

Japan’s Bullet Trains: The Pinnacle of Precision and Passenger Respect
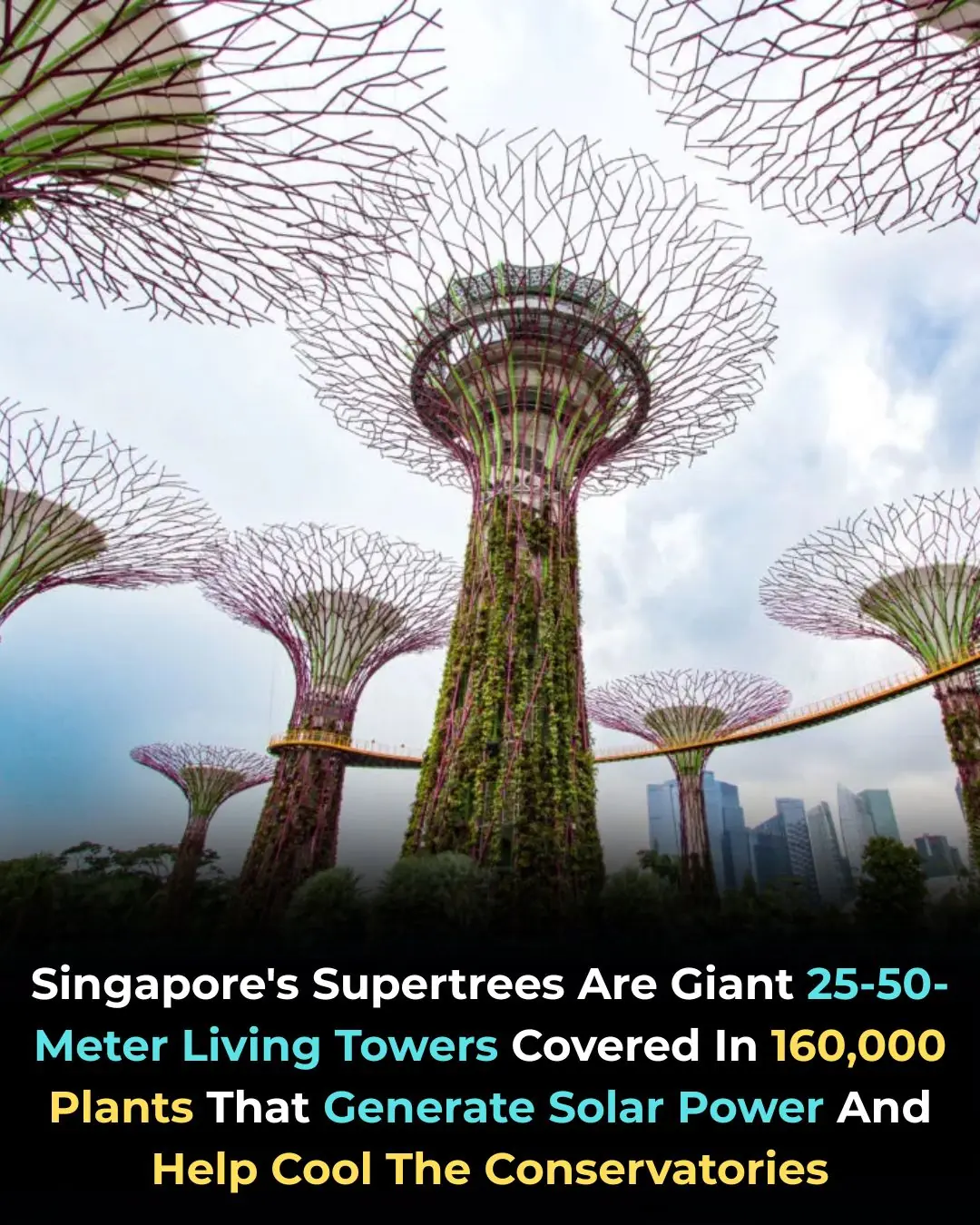
Singapore’s Supertrees: A Fusion of Architecture, Nature, and Clean Energy
The Hidden Health Risks of Eating Instant Noodles 2-3 Times a Week: What Science Really Says
